The Diabetes, Obesity and Metabolism Institute (DOMI) at the Icahn School of Medicine at Mount Sinai made further outstanding progress in 2022 in the study of diabetes, obesity, and metabolic syndromes. Under the leadership of Andrew F. Stewart, MD, Professor of Medicine (Endocrinology, Diabetes and Bone Disease), the Institute has expanded significantly in the last 10 years, with physician-scientists from departments throughout the Mount Sinai Health System.
“Under Dr. Stewart’s leadership, DOMI continues its impressive growth trajectory,” says Andrea Dunaif, MD, Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes and Bone Disease, Icahn Mount Sinai. “Dr. Stewart has assembled an outstanding cadre of investigators to study a broad spectrum of topics relevant to diabetes, metabolism, and obesity, ranging from the central nervous system control of metabolism, through fat cell biology, to therapies to regenerate pancreatic beta cells.”
“These are exciting times for diabetes research and care at the Icahn School of Medicine at Mount Sinai,” Dr. Stewart says. “We have created a diverse but very integrated diabetes and metabolism research environment that includes broad expertise in type 1 and type 2 diabetes, in beta cell biology and therapy, in fat cells and insulin resistance, in brain cells that control metabolism, in liver cells and liver failure, in cell culture, in intact animals and in humans, and in the immune system abnormalities in type 1 diabetes. We also are an institute without walls, welcoming faculty and trainees from throughout the medical school, exemplified by members of the Division of Endocrinology, Diabetes and Bone Disease—illustrated by Drs. Emily Gallagher and Andrea Dunaif—the Cardiovascular Research Institute, the Psychiatry Department, the Precision Immunology Institute (PrIISM), the Division of Pediatric Endocrinology, the Division of Liver Disease, and many others.”
Significant efforts in 2022 at DOMI include Dr. Stewart’s findings on the mechanism of beta cell regeneration, and a novel study into the mechanisms linking elevated triglyceride levels and triple negative breast cancer, led by Dr. Gallagher, Associate Professor of Medicine (Endocrinology, Diabetes and Bone Disease). Below are summaries of notable research by two more leaders at DOMI, Sarah A. Stanley, MBBCh, PhD, Associate Professor of Medicine (Endocrinology, Diabetes and Bone Disease), and Neuroscience; and Donald Scott, PhD, Professor of Medicine (Endocrinology, Diabetes and Bone Disease).
Stanley Lab

3-D image of sympathetic neurons in the coeliac ganglia that innervate the pancreas to modulate glucose control.
Publication:
Mapping and targeted viral activation of pancreatic nerves in mice reveal their roles in the regulation of glucose metabolism
Nature Biomedical Engineering, July 2022
Summary:
A lack of comprehensive mapping of ganglionic inputs into the pancreas and of technology for the modulation of the activity of specific pancreatic nerves has hindered the study of how they regulate metabolic processes. Here, we show that the pancreas-innervating neurons in sympathetic, parasympathetic, and sensory ganglia can be mapped in detail by using tissue clearing and retrograde tracing (the tracing of neural connections from the synapse to the cell body), and that genetic payloads can be delivered via intrapancreatic injection to target sites in efferent pancreatic nerves in live mice through optimized adeno-associated viruses and neural-tissue-specific promoters. We also show that, in male mice, the targeted activation of parasympathetic cholinergic intrapancreatic ganglia and neurons doubled plasma-insulin levels and improved glucose tolerance, and that tolerance was impaired by stimulating pancreas-projecting sympathetic neurons. The ability to map the peripheral ganglia innervating the pancreas and to deliver transgenes to specific pancreas-projecting neurons will facilitate the examination of ganglionic inputs and the study of the roles of pancreatic efferent innervation in glucose metabolism.
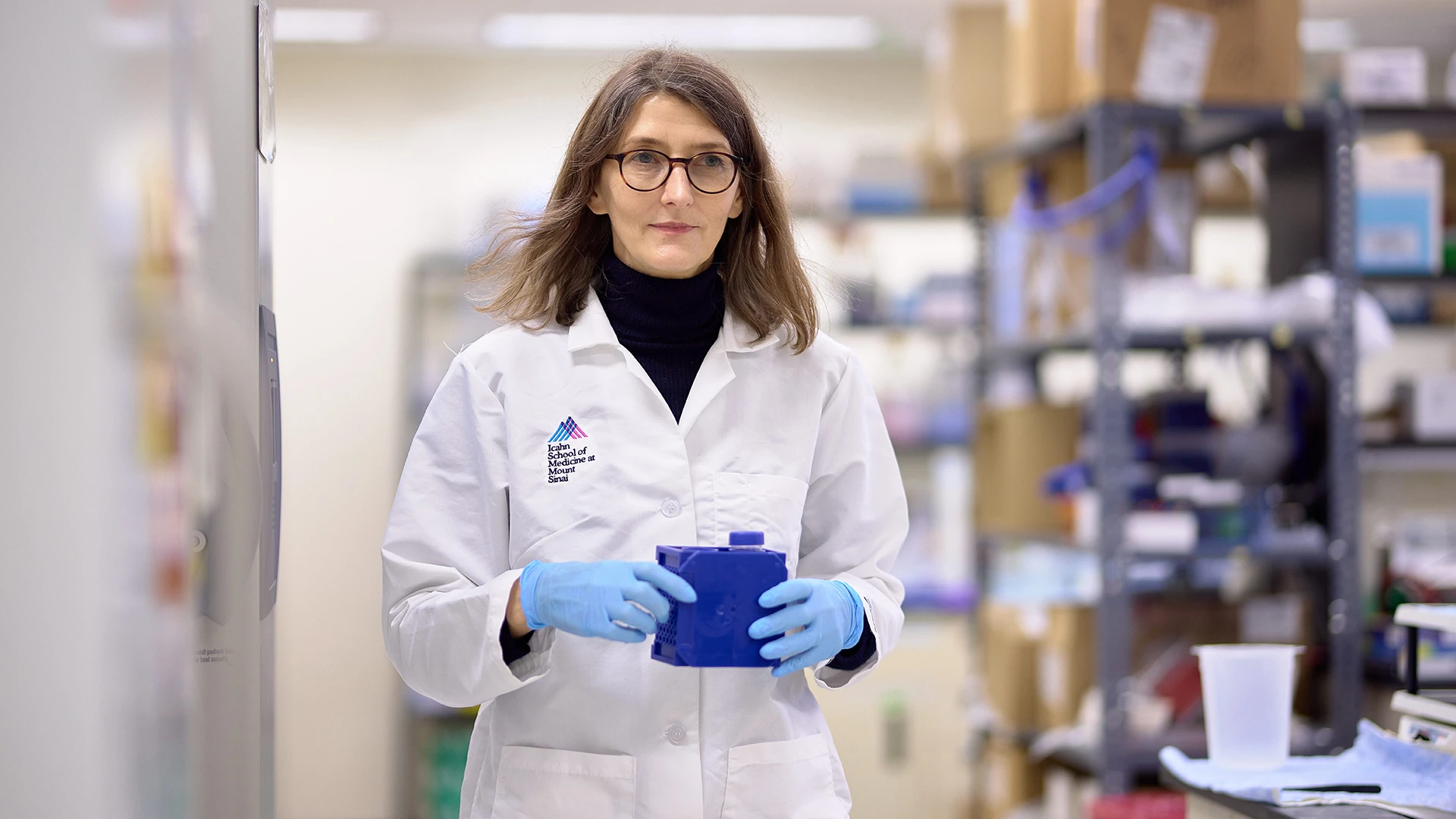
Sarah A. Stanley, MBBCh, PhD
Takeaway Message: Sarah A. Stanley, MBBCh, PhD
Neural signals are relayed between the brain and peripheral organs, such as the pancreas, by the peripheral nervous system. However, the roles of these nerves in regulating organ function are poorly understood.
In the lab, we have developed state-of-the-art tools that allow us to map and control the neural signals to the pancreas. These tools will allow us to determine how the neural circuits to the pancreas develop, and importantly, whether there is rewiring of the pancreas in diseases such as diabetes.
The techniques also allow us to deliver genes that can modulate nerve function. By switching pancreatic nerves on or off and examining the effects on pancreas function, we can begin to understand the roles of neural signals to the pancreas in controlling blood glucose. When we switch on specific pancreatic nerves, we can lower blood glucose in nondiabetic mice without causing hypoglycemia. These results suggest it may be possible to harness neural signals to improve insulin release and lower blood glucose. Our ongoing studies are now assessing if this approach is effective in diabetic mice.
Our studies could potentially have translational implications. There are already approved nerve stimulators used for conditions such as migraine and epilepsy and approved drugs that target specific receptors. It is possible that these could be repurposed to target the signals to the pancreas and so improve glucose control.
Our tools highlight the importance of an understudied area, the peripheral nervous system, in regulating pancreatic function and suggest it may be possible to harness these signals to treat diabetes. The techniques we developed could also provide insights into the contribution of neural signals to other pancreatic diseases, such as pancreatitis and pancreatic cancer.
Scott Lab
Publication:
“Maladaptive positive feedback production of ChREBPβ underlies glucotoxic β-cell failure”
Nature Communications, July 2022
Summary:
Preservation and expansion of beta cell mass is a therapeutic goal for diabetes. Here we show that the hyperactive isoform of carbohydrate response-element binding protein (ChREBPβ) is a nuclear effector of hyperglycemic stress occurring in beta cells in response to prolonged glucose exposure, high-fat diet, and diabetes. We show that transient positive feedback induction of ChREBPβ is necessary for adaptive beta cell expansion in response to metabolic challenges. Conversely, chronic excessive beta cell-specific overexpression of ChREBPβ results in loss of β cell identity, apoptosis, loss of β cell mass, and diabetes. Furthermore, β cell “glucolipotoxicity” can be prevented by deletion of ChREBPβ. Moreover, ChREBPβ-mediated cell death is mitigated by overexpression of the alternate CHREBP gene product, ChREBPα, or by activation of the antioxidant Nrf2 pathway in rodent and human beta-cells. We conclude that ChREBPβ, whether adaptive or maladaptive, is an important determinant of beta-cell fate and a potential target for the preservation of beta cell mass in diabetes.

ChREBPβ is required for adaptive beta cell expansion but contributes to glucose toxicity with prolonged hyperglycemia, and effects of its overexpression can be rescued by activation of the Nrf2 antioxidant pathway.
Takeway Message: Donald Scott, PhD
Diabetes results from insufficient beta cell mass. When blood glucose levels rise, such as in response to a high-fat diet, beta cells respond by producing and releasing more insulin to manage blood glucose levels. Prolonged hyperglycemia, which may occur due to insulin resistance, hinders the ability of beta cells to produce and secrete insulin. This leads to a vicious cycle of rising glucose levels and declining beta cell activity, eventually leading to the death or dedifferentiation of beta cells, a phenomenon known as glucose toxicity. Thus, preservation and regeneration of functional beta cell mass are important therapeutic goals for diabetes research.
We discovered a molecular mechanism involving carbohydrate response-element binding protein (ChREBPβ), a glucose-sensing transcription factor, that is involved in both beta cell regeneration and glucose toxicity. We found that a hyperactive isoform of this protein, ChREBPβ, is required (at least in mice) for beta cells to replicate in response to an elevated demand for insulin caused by a high-fat diet or significant glucose exposure. However, overproduction of ChREBPβ from prolonged hyperglycemia or by genetic manipulation leads to glucose toxicity and beta cell death. Moreover, we found that genetic deletion of ChREBPβ or activation of the antioxidant Nrf2 pathway mitigates the effects of ChREBPβ-mediated cell death and protects beta cells from glucose toxicity.
Future studies will include exploring the impact of ChREBPβ overproduction in patients with type 1 diabetes. We also plan to screen for small molecules that block ChREBPβ production and thus prevent glucose toxicity and the subsequent beta cell death. Furthermore, we plan to investigate whether the molecular mechanism that was described in this study occurs in other tissues in which ChREBPβ is expressed, such as kidney, liver, and adipose tissue, and therefore contributes to diabetic complications. In summary, our findings create an opportunity to develop beta cell-targeted therapeutic agents that inhibit ChREBPβ production, and thus preserve beta cell mass.
From left: Donald Scott, PhD, with Isabelle Tse, Lab Manager; Sharon Baumel-Alterzon, PhD, Instructor; Liora Katz, PhD, Assistant Professor of Medicine (Endocrinology, Diabetes and Bone Disease); and Fatema Haidery, graduate student.