Ash Tewari, MBBS, MCh, FRCS (Hon.), DSc (Hon.), was quick to recognize the promise of artificial intelligence and machine learning in medicine. Beginning in the 1990s, with prostate cancer diagnoses rising, he saw an opportunity to harness the increasing amount of prostate cancer data to improve diagnosis and treatment. Ever since, he has stayed on the cusp of innovation.
Now that powerful AI tools have caught up to his ideas, he is leading several projects that could transform the field—through better predictive tools and more effective surgery.
“Artificial intelligence is not just reshaping prostate cancer,” says Dr. Tewari, Professor and Chair, Milton and Carroll Petrie Department of Urology, Mount Sinai Health System, and Director of the Center of Excellence for Prostate Cancer at the Mount Sinai Tisch Cancer Center, Icahn School of Medicine at Mount Sinai. “It is helping us tackle the disease more effectively, from predicting outcomes with greater accuracy, to identifying surgical approaches that optimize functional recovery and quality of life after surgery.”
“We have developed AI models to help evaluate patients who fall into the gray zone of prostate cancer, where the next best step is often uncertain. This approach helps us individualize care, reduce unnecessary procedures, and move closer to true precision medicine,” Dr. Tewari says. “These tools can also help identify which patients are more likely to benefit from neoadjuvant therapies, who may achieve durable responses, and who are less likely to experience biochemical recurrence or metastasis over the long term.”
And that is just the beginning. “Artificial intelligence can extend beyond data to become a partner in education, communication, and surgical innovation,” he adds.
Improving Diagnosis and Treatment Through Big Data
After becoming interested in big data science in the 1990s, Dr. Tewari learned coding and began training computer models to sift through patient data and better predict which patients need a prostate biopsy. Such models can generate risk predictions based on a host of variables, including age, cancer grade, PSA values, and comorbidities.
In the years that followed, advances in genomics, MRI imaging, and histopathology added more data with even greater predictive value—and greater complexity.
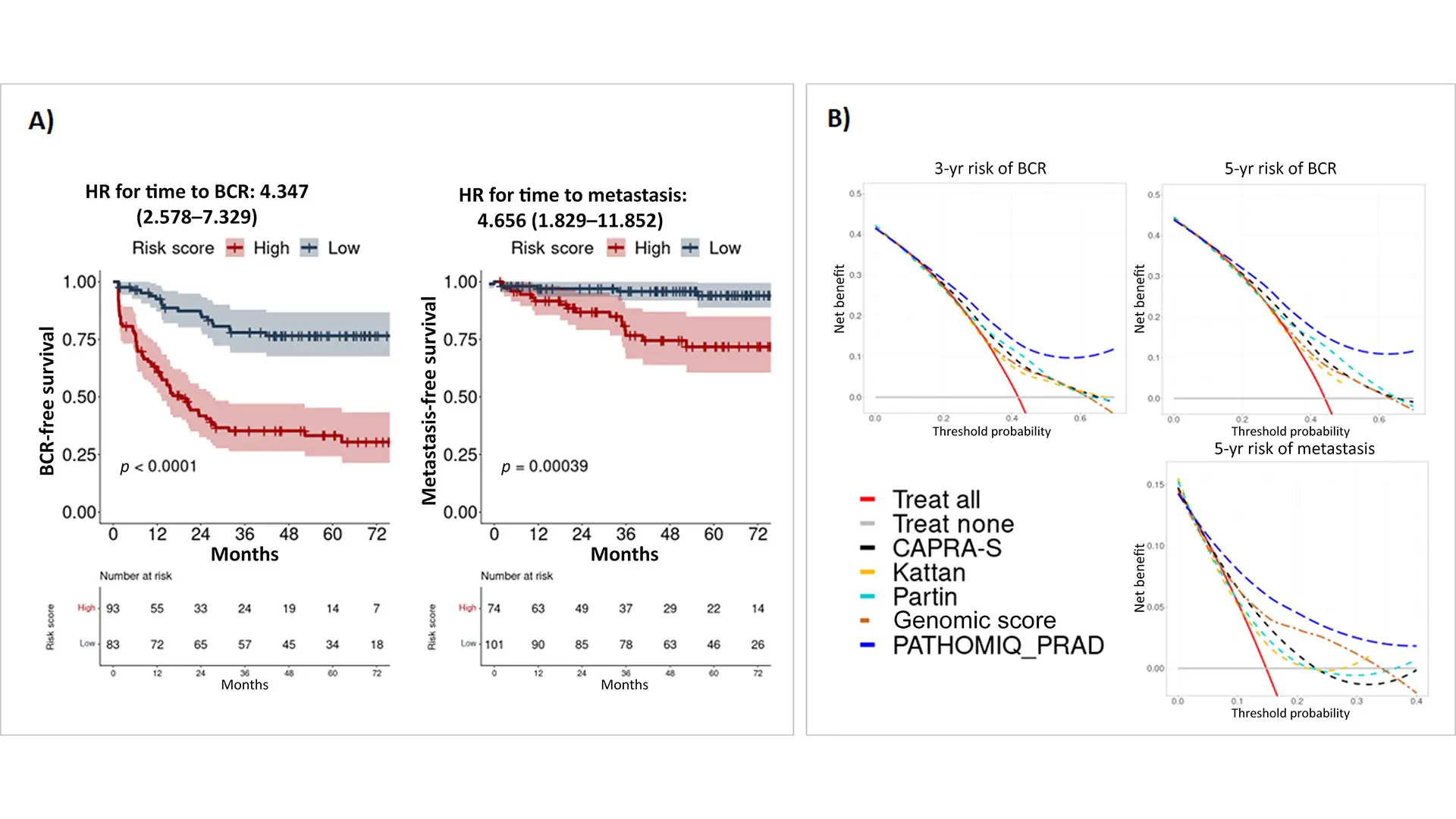
Modern AI allowed Dr. Tewari and his collaborators to leverage the data. They developed a tool, PATHOMIQ_PRAD, to stratify patients with intermediate-risk prostate cancer, identifying those at higher risk of rapid disease progression. The tool uses deep learning to extract morphological features from datasets derived from biopsy or surgical hematoxylin- and eosin-stained whole-slide images. By providing more timely, accurate predictions, patients at risk can benefit from earlier interventions and more targeted, personalized treatment plans. The research was published in European Urology in 2025.
Building on the success of PATHOMIQ_PRAD, Dr. Tewari and his team have now extended the PATHOMIQ artificial intelligence platform to address one of the most critical challenges in prostate cancer care: identifying which patients are truly appropriate candidates for active surveillance.
While active surveillance can spare patients from unnecessary treatment and preserve quality of life, selecting the right patients remains challenging. Traditional clinical and pathological criteria often fail to capture subtle biological features associated with disease progression.
Using AI-driven analysis of histopathology, the extended PATHOMIQ model is designed to predict which patients are most likely to benefit from active surveillance and which may require earlier intervention. Dimple Chakravarty, PhD, Associate Professor, Department of Urology, is spearheading this expansion of PATHOMIQ into active surveillance, including the design and launch of a prospective clinical study that will use the AI model to guide patient enrollment and outcome prediction in active surveillance cohorts.
“This allows us to move from population-based guidelines to truly individualized decision-making,” Dr. Tewari says. “The goal is to confidently identify patients who can safely avoid treatment while ensuring that those with higher-risk biology are not undertreated.
With support from a National Institutes of Health (NIH) R01 grant, Dr. Tewari is continuing to expand his AI research. One goal is to create an electronic prostate-specific awareness tool that can identify a patient’s prostate cancer risk based on factors such as lifestyle, demographics, and family history.
“We cannot biopsy everyone or check everyone’s PSA. My hope with this project is to identify people with a higher risk so they can move to the next level of investigation and cancer can be detected earlier,” he says.
A specific goal of this project is to develop a multiphoton microscopy (MPM) and artificial intelligence enabled Race-Specific Stroma-Weighted Automated Gleason Grading (SWAG) system to improve risk stratification in cases of high-risk prostate cancer.
Black men have a 70 percent higher rate of developing high-risk prostate cancer than white men. Black men also have a much higher incidence of aggressive cancer, even in low-risk grades, and are twice as likely to die of prostate cancer, making this problem a concern for the NIH’s National Cancer Institute. While many non-biological factors contribute to this higher cancer burden in Black men, Dr. Tewari’s team has found that tumor biology plays a critical role in the observed disparities. Furthermore, their findings showed the crucial underlying role of activated stroma in orchestrating tumor-promoting inflammatory flare-ups and tumor microenvironment alterations common to Black men's tumors.
Similar tools can help inform decisions, such as when to perform a biopsy and even what area of the prostate to target to increase the odds that the biopsy correctly identifies a tumor. AI-enabled predictive tools could also help physicians decide between treatment approaches, such as focal therapy, robotic radical prostatectomy, and radiation therapy.
In another project, Dr. Tewari’s team is using AI to study “super healers”—men who recover quickly and regain full potency in as little as six weeks after surgery. They aim to create an AI model that can forecast which patients are strong candidates for full recovery and which may benefit from more targeted rehabilitation.
AI-Powered Surgery
Artificial intelligence also has the potential to improve surgical techniques and postsurgical outcomes for prostate cancer patients. In one project, Dr. Tewari and his colleagues are developing AI-powered, real-time video annotation tools to enhance surgical precision. The tool identifies each surgical step and detects deviations, offering instant feedback to support surgeons. “The system will be a valuable addition to resident education and can also provide intraoperative decision support, potentially improving surgical outcomes,” Dr. Tewari says.
The research was described in Urologic Oncology: Seminars and Original Investigations in a paper with colleagues, including Laura Zuluaga, MD, a research fellow at the Icahn School of Medicine, and senior author Ketan Badani, MD, Professor of Urology, Icahn School of Medicine, and Vice Chair of Urology and Robotic Operations at the Mount Sinai Health System.
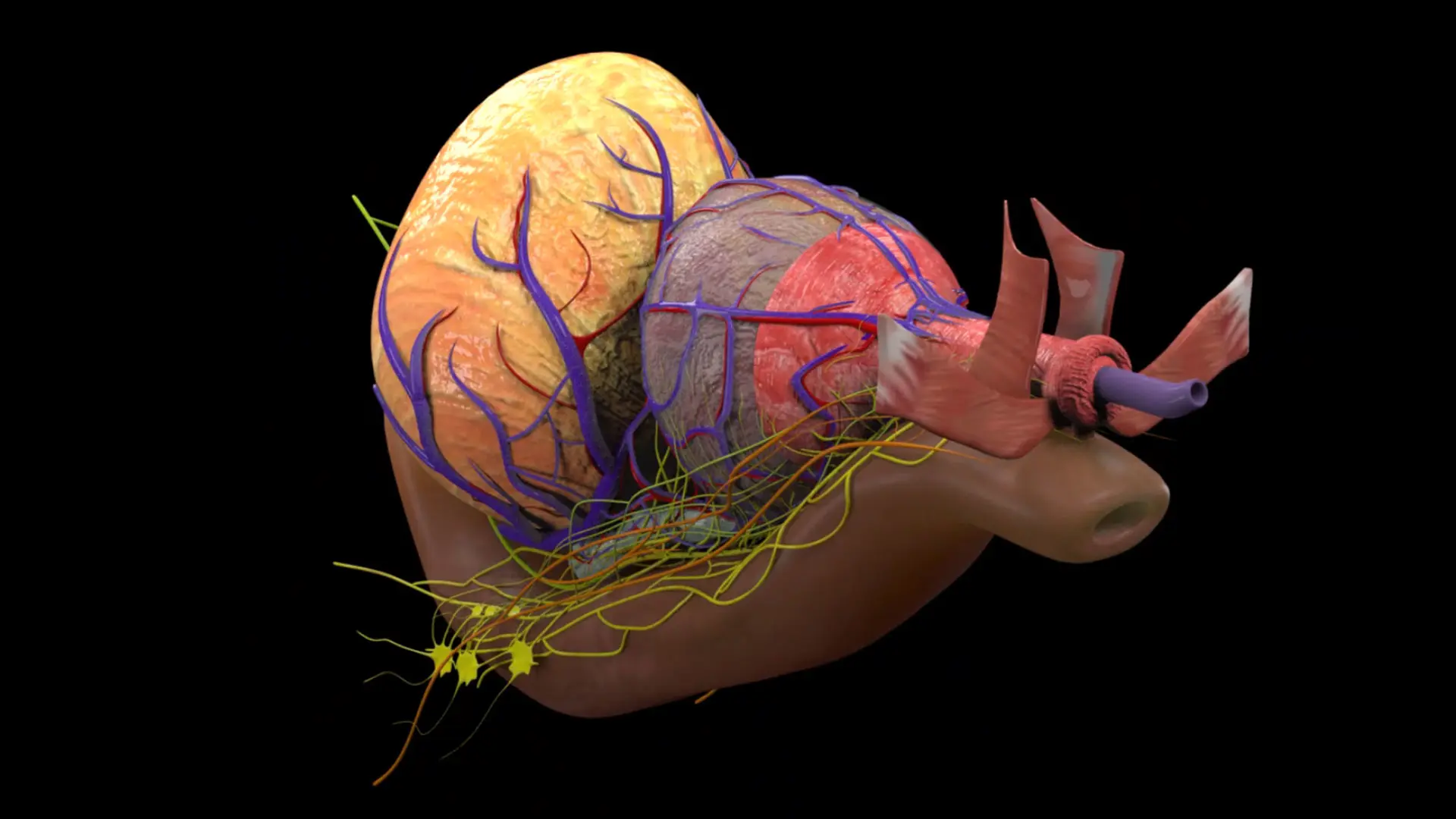
The possibilities do not end there. In a preliminary project, Dr. Tewari is also working on an AI model trained to recognize nerve tissue. Overlaid with real-time video from the robotic surgical system, the annotation tool makes the nerves appear to glow, making them easier to avoid during tumor dissection. Such technology could enhance nerve-sparing approaches, maximizing the recovery of sexual and urinary function while also maximizing cancer removal.
As Dr. Tewari and his colleagues, including Michael Gorin, MD, Associate Professor, and Ashwin Ramaswamy, MD, MPP, Instuctor, continue to push the envelope, he credits his success to the supportive environment at the Icahn School of Medicine.
“Mount Sinai is among the most tech-savvy institutions. It has the infrastructure, staff, and desire in place to take us to the next level of reality,” he says. “AI will not replace urologists, but it will coexist with us, enhancing our ability to predict outcomes, personalize therapy, preserve function, and improve survival. Those of us who join the revolution can grow to greater heights than ever before.”
With Mount Sinai’s robust infrastructure, interdisciplinary collaboration, and commitment to innovation, these AI-powered advances are poised to deliver a radical shift in prostate cancer care, one that prioritizes both oncologic control and long-term quality of life.