
For 2025, it was a year of groundbreaking achievements, national recognition, and transformative research in the Department of Urology at Mount Sinai.
Together, we continue to redefine excellence in patient care, innovation, and education.
In 2025, our Department saw more than 120,000 patients, performed almost 11,000 surgeries, and reached more than 3,800 people through our mobile unit initiative. These milestones reflect the dedication of our faculty, staff, and collaborators, and underscore our unwavering commitment to delivering exceptional patient care while advancing innovation and research across the field of urology.
From community outreach and advanced robotics to AI-powered precision medicine, 2025 reflects our unified mission: to deliver compassionate, cutting-edge care and drive discovery that transforms lives.
Thanks go to our patients, faculty, collaborators, and partners for their continued trust and support, which make this work possible.
Ash Tewari, MBBS, MCh, FRCS (Hon.)
Professor and System Chair, Milton and Carroll Petrie Department of Urology
Chair of Urology, Mount Sinai Hospital
Natasha Kyprianou, MBBS, PhD
Vice Chair of Basic Science Research
Department of Urology
Icahn School of Medicine at Mount Sinai
Awards and Recognitions
Institutional Excellence
Mount Sinai Urology ranked No. 1 in New York for NIH funding by the Blue Ridge Institute for Medical Research (BRIMR) Rankings.
National Awards
Mantu Gupta, MD—Elected Member- Society of Genitourinary Surgeons
Natasha Kyprianou, PhD—Appointed Chair of American Association for Cancer Research (AACR) Clinical and Translational Cancer Research Grants Committee
Mani Menon, MD—Recipient of AUA Ramon Guiteras Award
Mani Menon, MD—Asian-American Pioneer Award
Rajvir Purohit, MD—Elected to the Board of Directors- Society of Genitourinary Surgeons
John P. Sfakianos, MD—Honored as AUA Young Urologist of the Year
Departmental Honors
Mani Menon, MD—Dr. John Barry Award (Clinical Society of Genitourinary Surgeons)
Natasha Kyprianou, PhD—Mount Sinai Steven Southwick, MD Award for Prostate Cancer Research Excellence
International Honors
Ash Tewari, MBBS, MCh, FRCS (Hon.) — Elected Honorary Member of the Royal College of Physicians and Surgeons, Glasgow, UK
Grants and Funding (2025)
Philanthropy and Program Support
The Robert F. Smith Mobile Prostate Screening Unit was launched with a $3.8 million philanthropic gift, expanding prostate screening access and outreach. The initiative is highlighted as a $4 million community investment in Mount Sinai’s Chair’s Message. The Robert F. Smith Foundation continues to spotlight the program’s progress and community impact.
Regional Expansion and Partnerships
The Mount Sinai–Emory/Winship collaboration, supported by the Arthur M. Blank Family Foundation, enhances research integration and patient access across regions.
Federal (NIH/NCI) Research Grants
Ash Tewari, Surinder Batra, Gustavo Ayala ; MPI R01 NIH/NCI Grant (CA290438): ”Artificial intelligence enabled Stroma-Weighted Automated Grading system to improve risk stratification in Black Men”
Natasha Kyprianou, Navneet Dogra, Ash Tewari, MPI R01 NCI/NIH Grant: “Profiling the Tumor Microenvironment in Prostate Cancer Progression”
John Sfakianos, R01 NCI/NIH Grant: “Targeting the Androgen Receptor to Sensitize Bladder Cancer and Urine Tumor Nucleic Acid Profiling”
Juan Arriaga: R01 NCI/NIH Grant: Role of ATAD2 in Prostate Cancer Progression and Metastasis
Prathiksha Prabhakaraalva, (Mentor: Goutam Chakraborty): Department of Defense Congressionally Directed Medical Research Programs (CDMRP), Prostate Cancer Research Program (PCRP) Early Investigator Research Award: “Investigating the Impact of Reprogrammed PIK3R1-Insulin-Glucose Metabolism Pathway in Lethal Prostate Cancer to Develop Therapeutic Strategy”
Anindita Dutta (Mentor : Juan Arriaga): Department of Defense Prostate Cancer Research Program (PCRP) Early Investigator Research Award Grant on “Tumor-intrinsic Epigenetic Mechanisms Modulating Antitumor Responses in Metastatic Prostate Cancer”
Mount Sinai participation in Prostate Cancer SPORE-linked funding featured in 2025 NCI records
Food and Drug Administration Approved Clinical Trials
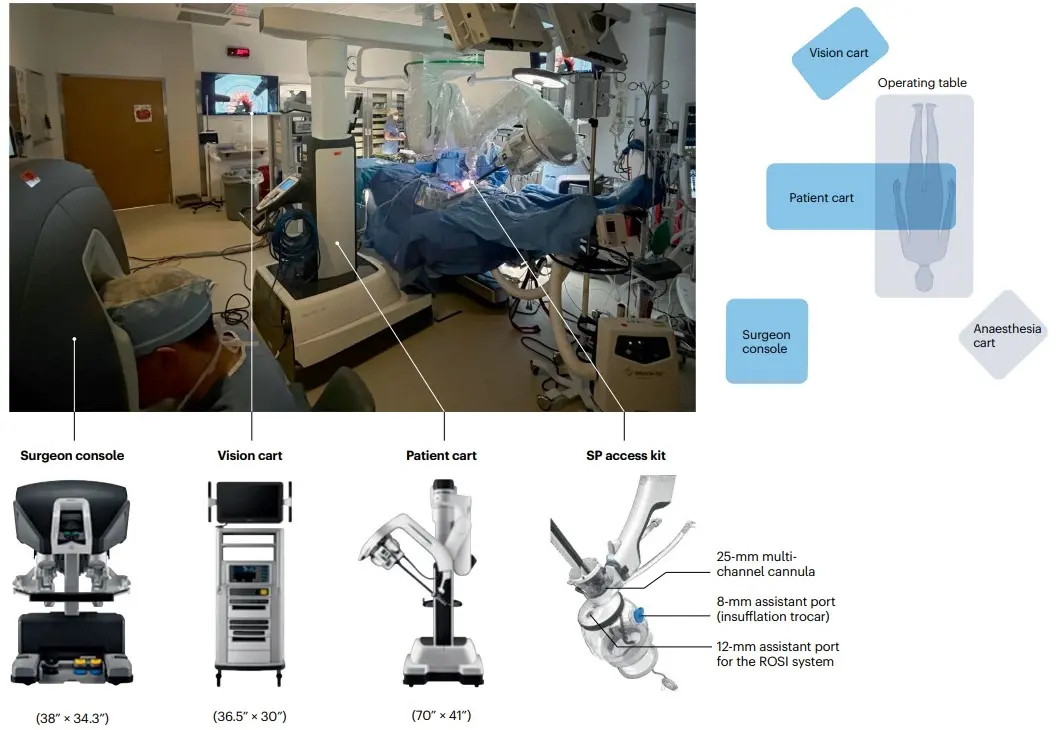
On December 5, 2025, the FDA cleared the HUGO robotic-assisted surgery system for urologic surgical procedures in the United States
Protocol title: A prospective, multi-center, single-arm study of the Medtronic Hugo™ Robotic Assisted Surgery (RAS) System in Urologic Surgery (Expand URO)
Investigators: Peter Wiklund, John Sfakianos, Reza Mehrazin
Scientific Publications (2025) (selected peer-reviewed articles out of more than 300)
Prostate Cancer, Risk Tools, AI & Molecular Mechanisms
• Tillu N, et al. Predicting side-specific extraprostatic extension in prostate cancer using an 18F-DCFPyL PSMA-PET/CT–based nomogram. Prostate Cancer and Prostatic Diseases
• Wagaskar VG, et al. Integrating genomic classifiers in predictive modelling for lymph node metastasis in localized prostate cancer. Urologic Oncology
• Mandel A, et al. Hood technique for radical prostatectomy. Journal of Endourology
• A novel machine learning–based predictive model of clinically significant prostate cancer and online risk calculator. Urology
• Yue W, et al. Circadian rhythm–related miR-6883-5p suppresses enzalutamide-resistant prostate cancer. Non-coding RNA Research
• Figiel S, et al. Exploring the transformative potential of spatial ’omics in uro-oncology. European Urology
• Kolanukuduru KP, et al. Comparative effectiveness of partial gland cryoablation versus robotic radical prostatectomy. European Urology Focus
• Kolanukuduru KP, et al. Resolving micro-ultrasound lesions in patients on active surveillance for localized prostate cancer. Journal of Urology
• Bertini A, et al. Mortality and additional treatment rates in pathologically high-risk prostate cancer. The Prostate
• Kaufmann B, et al. Diagnostic value of micro-ultrasound in identifying local recurrence after radical prostatectomy. The Prostate
• Nepali PR, et al. Effect of TGF-β–mediated phenotypic changes on prostate cancer cell anoikis response. Oncogene
• Hirani R, et al. BCL2 drives castration resistance in prostate cancer. Cell Reports
• King SA, et al. Y-chromosome alteration and its impact on cancer progression. Cellular & Molecular Biology Letters
• Sattler A, et al. Sympathetic nerve signaling rewires the tumor microenvironment. Cancer and Metastasis Reviews
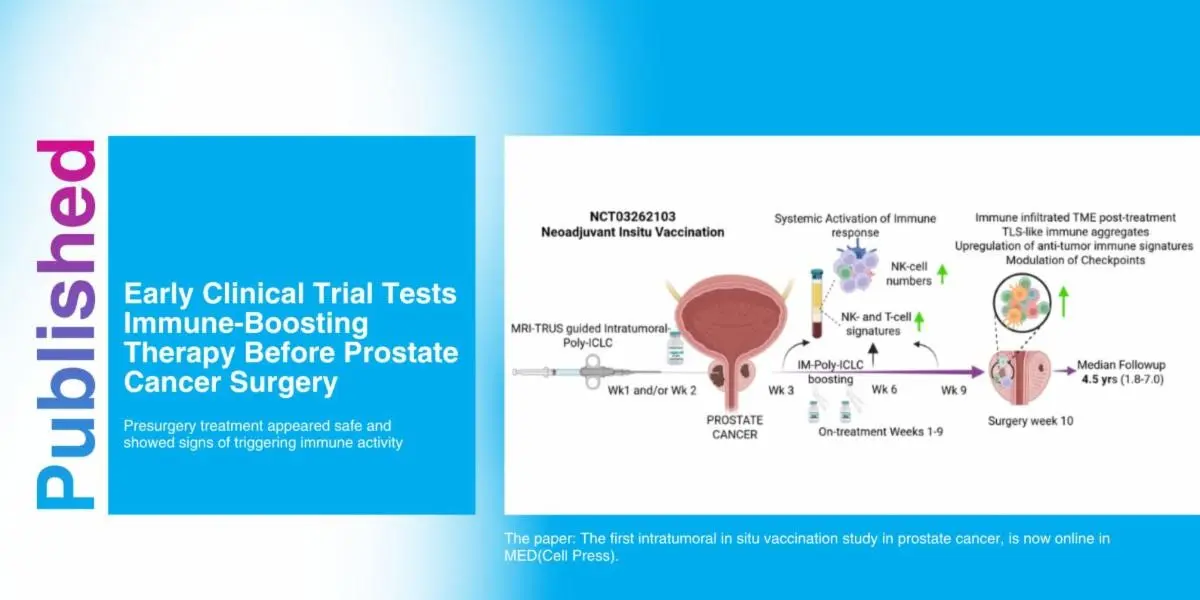
• Nair SS, et al. Prostate cancer in situ autovaccination with Poly-ICLC. Med
• Fay M, et al. Artificial intelligence-based digital histologic classifier for prostate cancer risk stratification: independent blinded validation in patients treated with radical prostatectomy. JCO Clin Cancer Inform
• Nair SS, et al. A novel artificial intelligence–powered tool for precise risk stratification of prostate cancer progression in patients with clinical intermediate risk. Eur Urol
• Okhawere KE, et al. Novel bioabsorbable, low-dose rate brachytherapy device (CivaSheet®) with radical prostatectomy and adjuvant external beam radiation for the management of prostate cancer. BJU Int
• Falagario UG, et al. Epidemiology of high-risk biochemical recurrence after primary prostate cancer treatment. Eur Urol Oncol
• Mandel A, et al. Analysis of the current surgical anatomical knowledge of radical prostatectomy: an updated review. Eur Urol
• Vathiotis I, et al. Histologic transformation in cancer: the path for clinical translation. Cancer Discov
• Pedraza AM, et al. Transperitoneal robot-assisted radical prostatectomy: Hood technique. The Comprehensive Atlas of Robotic Urologic Surgery
• Zaman N, et al. Molecular insights and biology of low-PSA high-risk prostate cancer. Cancer Res
• Liao RS, et al. AI-based digital histologic classifier for prostate cancer risk stratification: independent blinded validation in patients treated with radical prostatectomy. Journal of Urology
• Zahalka A, et al. An open-label phase 1, window-of-opportunity study of ultrasound-guided long-acting periprostatic neuraxial block with ethanol in patients with high-risk prostate cancer. Journal of Clinical Oncology
Notable authors: Tewari, Kyprianou, Menon, Chakraborty, Nair.
Kidney, Robotics
Soputro NA, et al. Single-port robotic retroperitoneal partial nephrectomy via low anterior access: a propensity-matched comparative analysis to standard transperitoneal multiport robotic surgery from the Single Port Advanced Research Consortium (SPARC). European Urology Focus
Biasatti A, et al. The current landscape of single-port robotic surgery in urology. Nature Reviews Urology
Soputro NA, et al. Development of patient-specific nomogram: single-port vs. multi-port robotic partial nephrectomy. Journal of Endourology
Connors C, et al. Trends, outcomes, and predictors of open conversion during minimally invasive radical nephroureterectomy for upper tract urothelial carcinoma: a national analysis from 2010 to 2020. Journal of Robotic Surgery
Nepali PR, et al. Molecular and therapeutic landscape of non-clear cell renal carcinoma. Nature Reviews Urology
Notable authors: Badani, Kyprianou, Mehrazin, Wiklund, Propiglia.
Endourology and Stone Disease
Gupta K, et al. Laser lithotripsy induces dose-dependent temperature elevation during retrograde intrarenal surgery. Journal of Endourology.
Serna J, Khargi R, et al. Mini-percutaneous nephrolithotomy less injurious to the kidney? Journal of Endourology.
Durbhakula V, et al. Should percutaneous nephrolithotomy be performed in patients with severe chronic kidney disease? A closer look at renal function outcomes. World Journal of Urology.
Frangopoulos E, et al. Aspiration technologies in flexible ureteroscopic urolithiasis treatment: A disruptive concept in pursuit of a stone-free future. Journal of Endourology.
Frangopoulos E, et al. Increased risk of kidney stones in transgender women and gender-diverse adults on gender-affirming hormone therapy: Insights from a large database study. Journal of Endourology.
Savin Z, et al. Evaluating blood and urinary markers for prediction of spontaneous ureteral stone passage. American Journal of Clinical and Experimental Urology.
Savin Z, et al. Randomized controlled trial of nonsteroidal anti-inflammatory drugs as a safe and effective alternative to opioids for pain relief following percutaneous nephrolithotomy. Journal of Endourology.
Gupta K, et al. Harnessing artificial intelligence to predict spontaneous stone passage: Development and testing of a machine learning–based calculator. Journal of Endourology.
Gupta M, et al. High-power lasers induce dose-dependent acute kidney injury. Journal of Endourology.
Savin Z, et al. Does having an asymptomatic renal stone increase morbidity after radical cystectomy? World Journal of Urology.
Yaghoubian AJ, et al. Patients who catastrophize pain experience increased pain after ureteroscopic laser lithotripsy with stent placement. Journal of Endourology.
Chew BH, et al. Prospective evaluation of efficacy, safety, cumulative laser energy, and stone-free rates in the SOLTIVE™ SuperPulsed laser system registry. Urolithiasis.
Gupta K, et al. Is outpatient totally tubeless standard percutaneous nephrolithotomy safe and efficacious? Journal of Endourology.
Connors C, et al. Pushing the envelope: Ambulatory percutaneous nephrolithotomy for patients with complex renal calculi. Journal of Endourology.
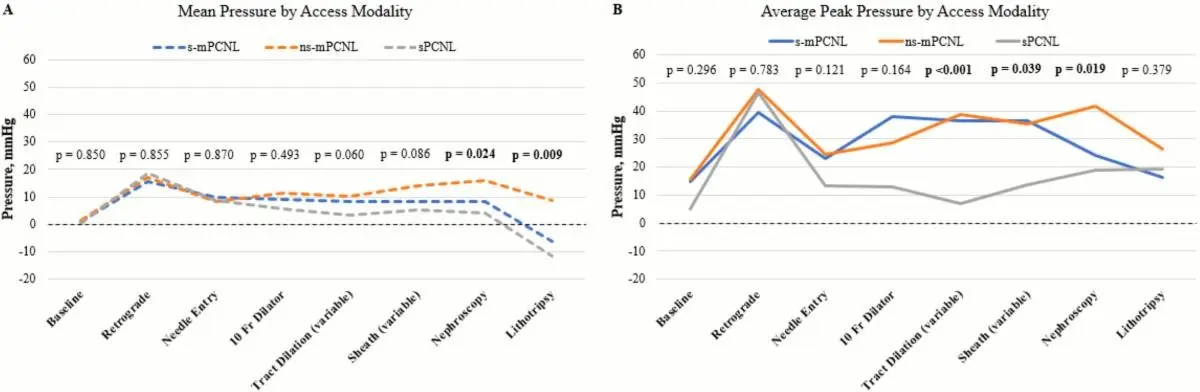
Khargi R, et al. Does mini-percutaneous nephrolithotomy increase intrarenal pressure and can this be mitigated by a suctioning sheath? Journal of Endourology.
Notable authors: Gupta, Savin, Atallah.
Bladder Cancer
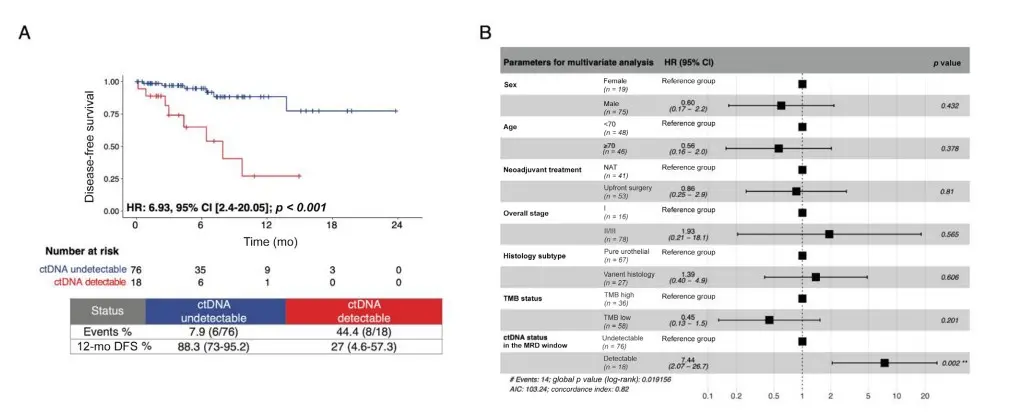
Sfakianos JP, et al. Association of tumor-informed circulating tumor DNA detectability before and after radical cystectomy with disease-free survival in patients with bladder cancer. European Urology Oncology.
Sfakianos J, et al. Impact of tumor burden or focality in recurrent low-grade intermediate-risk non–muscle-invasive bladder cancer on response to treatment with UGN-102: A substudy of the phase 3 ENVISION trial. Urologic Oncology.
Figiel S, et al. Clinical implications of basic research: Exploring the transformative potential of spatial ’omics in uro-oncology. European Urology.
Ben-David R, et al. Immunotherapy-based neoadjuvant treatment and complication rates after radical cystectomy. BJU International.
Eraky A, et al. Differential response of low- and high-grade intermediate-risk non–muscle-invasive bladder cancer to bacillus Calmette-Guérin and gemcitabine–docetaxel therapy. Urologic Oncology.
Tyson MD, et al. Economic impact model of incorporating Cxbladder Monitor in the surveillance of non–muscle-invasive bladder cancer. JU Open Plus.
Rich JM, et al. Contemporary outcomes for robotic radical cystectomy and intracorporeal neobladder urinary diversion. Urologic Oncology.
Eraky A, et al. Bladder cancer with undetectable circulating tumor DNA after radical cystectomy may be amenable to a less intense imaging surveillance protocol: A diagnostic accuracy study. European Urology Oncology.
Eraky A, et al. Bladder neck involvement in non–muscle-invasive bladder cancer: Risk implications and outcomes of BCG versus gemcitabine/docetaxel. BJU International.
Afferi L, et al. Oncological outcomes of open versus minimally invasive nephroureterectomy for locally advanced upper tract urothelial carcinoma. World Journal of Urology.
Eraky A, et al. Efficacy of bacillus Calmette-Guérin compared with sequential gemcitabine and docetaxel in Ta high-grade non–muscle-invasive bladder cancer. World Journal of Urology.
Gabriel P-E, et al. Therapeutic intensification based on immune checkpoint inhibitors in non–muscle-invasive bladder cancer: State of the art and future perspectives. Cancers.
Bertrand C, et al. A systematic review of gene-mediated therapy in BCG-unresponsive non–muscle-invasive bladder cancer: Emerging evidence and future perspectives. World Journal of Urology.
Notable authors: Sfakianos, Ben-David, Mehrazin, Wiklund.
Lifestyle and Behavioral Studies
Scharp D, et al. Unmet needs among adults with bladder cancer. Urologic Oncology.
Djordjevic S, et al. Lifestyle interventions to reduce genitourinary cancer risk. Springer Nature.
Notable authors: Mohamed and Kyprianou.
Reconstructive Urology
Ho P, Schmidt-Beuchat E, et al. Testicular implant complications after transmasculine gender-affirming surgery. International Brazilian Journal of Urology.
Selvaggi G, et al. Gender Affirming Vaginoplasty. Elsevier.
Sljivich M, et al. The use of bowel in gender-affirming vaginoplasty. In: Selvaggi G, Djordjevic ML, editors. Gender Affirming Vaginoplasty. Elsevier.
Sljivich M, et al. Feasibility and outcomes after robot-assisted sigmoid vaginoplasty for gender dysphoria. Urology.
Ho P, et al. Impact of vaginectomy technique on the safety and outcomes of transmasculine gender-affirming surgery. Journal of Sexual Medicine.
Blasdel G, et al. Outcomes following metoidioplasty and phalloplasty gender-affirming surgery with urethral lengthening: A modified Delphi consensus study. Urology.
Bizic M, et al. Neourethroplasty in masculinizing gender-affirmation surgery. International Journal of Reconstructive Urology.
Gozzi C, et al. Suprapubic transvesical adenoma resection of the prostate (STAR-P): Step-by-step technique. Canadian Journal of Urology.
Purohit RS. Introduction and guest editorial. International Journal of Reconstructive Urology.
Torres C, et al. Vaginoplasty: Maximizing aesthetic and functional outcomes of the vulva. International Journal of Reconstructive Urology.
Bucca B, et al. Hair management for transgender genital surgery: A comparative review of techniques and implications for neovaginal and urethral health. International Journal of Reconstructive Urology.
Notable authors: Djordjevic and Purohit.

International and National Collaborations
We have the privilege of engaging in creative collaborations globally, including Sweden, Finland, Germany, France, Italy, Japan, Australia, and Brazil, as well as nationally across Nebraska, California, New York, Georgia, and Maryland, in clinical and translational research.
