Robotic Kidney Surgery for Horseshoe Kidney: Navigating the Anatomical Challenges
A patient presenting with upper tract urothelial carcinoma (UTUC) involving a horseshoe kidney might seem best suited for treatment through an open surgery approach. But Mount Sinai surgeon Ketan K. Badani, MD, FRCS (Hon.), was able to achieve positive outcomes in one such case through a minimally invasive robot-assisted approach that combined the robust experience learned on elements of a partial nephrectomy, radical nephrectomy, and nephroureterectomy.
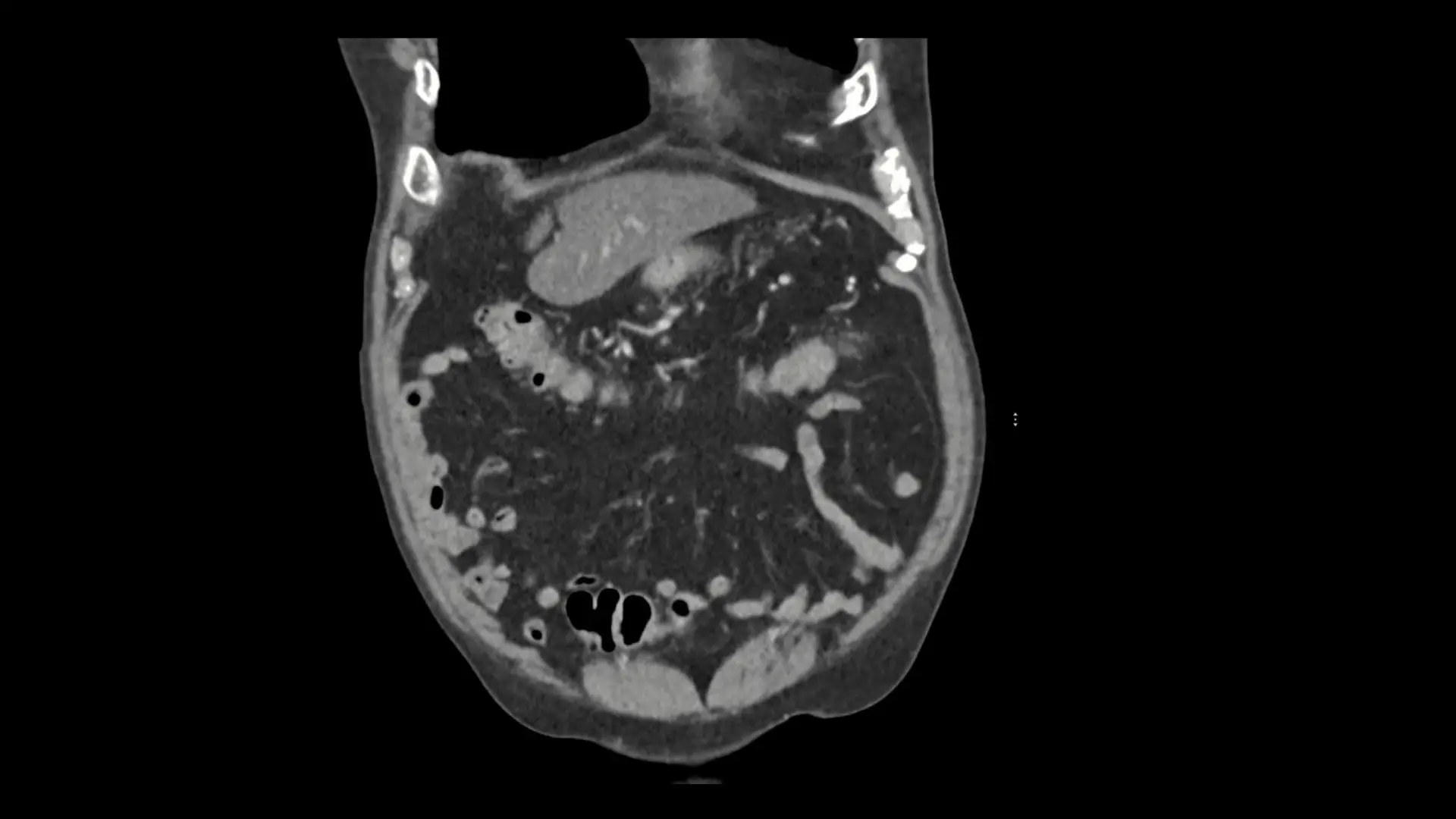
The patient, a 66-year-old male, was referred to Dr. Badani in July 2024 with a diagnosis of UTUC. Computed tomography imaging revealed the patient had a horseshoe kidney, several cysts, and small hypodense tissue that appears darker than surrounding tissue. Imaging also revealed a filling defect in the right renal collecting system. A biopsy of this lesion revealed high-grade urothelial carcinoma. The patient had a history of asthma, coronary artery disease, hypertension, hyperlipidemia, thyroid disease, and had undergone both abdominal surgery and removal of a kidney cyst in the past.
Based on the imaging and the patient history, Dr. Badani decided the best treatment approach would essentially combine a radical nephrectomy to resect the right side of the kidney moiety, followed by a partial nephrectomy to preserve the isthmus and left side of the kidney, and then complete the nephroureterectomy to resect the ureter and bladder cuff. He also decided he could achieve optimal outcomes for the patient using a robot surgical system.


“Given the complexity and patient history involved, this might seem like a case where you would opt for an open surgery approach, but it was not a consideration for me,” says Dr. Badani, Director of the Comprehensive Kidney Cancer Program, and Chief of Surgical Innovation and Strategy at the Mount Sinai Health System.
“We have extensive experience with robotic surgical systems, and we know what we are able to achieve with them. This was an opportunity to apply that knowledge for the benefit of the patient.”
Dr. Badani performed the procedure in September 2024. After placing the patient in a flank position, he used the multiport robotic surgery system to make several small incisions in the abdomen, enabling him to reflect the colon and other organs and tissue to access the retroperitoneum and horseshoe kidney.
He started by identifying several vascular structures supplying blood flow to the right moiety and to the isthmus. Immunofluorescence was utilized to identify and differentiate the right renal hilar vessels and those supplying the isthmus of the horseshoe. The renal hilar artery, and vein, was taken with endoscopic stapling as used during robotic radical nephrectomy. The vascular structures supplying the isthmus of the kidney were clamped with bulldog clamps and the left part of the isthmus was excised from the right under warm ischemia. The stump of the left isthmus was then reconstructed using the well-established partial nephrectomy technique developed by Dr. Badani–the F.A.S.T (First Assistant Sparing Technique) approach.
He then performed the ureterectomy, starting with careful isolation of the ureter, ensuring meticulous dissection along its length to preserve surrounding structures. In this procedure, he typically follows the ureter down to the bladder, mobilizing it completely to allow for a thorough removal. Finally, he excised the ureter at the bladder cuff, securing complete removal of the ureter and reducing the risk of residual tissue.
“The pathology was high-grade noninvasive papillary urothelial carcinoma with necrosis, and the ureteral, renal vein, and renal artery margins were all negative,” says Dr. Badani, who is also Professor of Urology at the Icahn School of Medicine at Mount Sinai and Vice Chair of Urology and Robotic Operations for Mount Sinai.
Dr. Badani completed the procedure in less than two hours and the patient was discharged 23 hours later. Based on follow-up consultations, he characterizes the patient’s kidney function as good and his post-surgical course as comparable to that of any standard robot-assisted partial or radical nephrectomy. Dr. Badani believes these results make a strong case for a robotic surgery approach for patients who present with complex anatomical variations, given the opportunities for enhanced surgical precision and visualization, not to mention a reduced risk profile in patients with comorbidities.
“I believe we have demonstrated that this technology minimizes the risk of complications associated with dissection and vascular management, ultimately improving the oncological outcomes we can achieve for our patients,” Dr. Badani says. “By sharing outcomes like these, we hope other surgeons will consider minimally invasive approaches in treating similar cases.”