The Mount Sinai Robert F. Smith Mobile Prostate Cancer Screening Unit was funded by a $3.8 million donation from philanthropist Robert F. Smith, right, who was honored by Ash Tewari, MBBS, MCh, and the Department at the 2023 Prostate Cancer Research Gala for his role in the initiative. This video was shown at the event.
Prostate cancer is the second most common form of cancer in American men. Black men have a 70 percent higher rate of high-risk prostate cancer, and they are more than twice as likely to die from it. Many of these deaths could be prevented by early screening.
Yet many Black men still avoid getting tested, in part because of fears and in part because of a lack of access to services. If more of these men were screened for prostate cancer, more lives would be saved.
That is the idea behind the Mount Sinai Robert F. Smith Mobile Prostate Cancer Screening Unit.
“I'm very hopeful this is going to be one of those sparks that leads to a platform of access to health care for the African American community, and saves lives.”
Robert Smith

The Mount Sinai Robert F. Smith Mobile Prostate Cancer Screening Unit visits neighborhoods across New York City, providing access to education and screening for all who visit.
In its second year, this innovative effort by the Milton and Carroll Petrie Department of Urology and Ash Tewari, MBBS, MCh, FRCS (Hon.), Professor and System Chair, to improve early detection of prostate cancer among at-risk populations in New York City, is demonstrating its ability to change the outcome of prostate cancer for the communities Mount Sinai serves, even as the Department continues to improve and expand its reach and services while defining the delivery of health care equity.
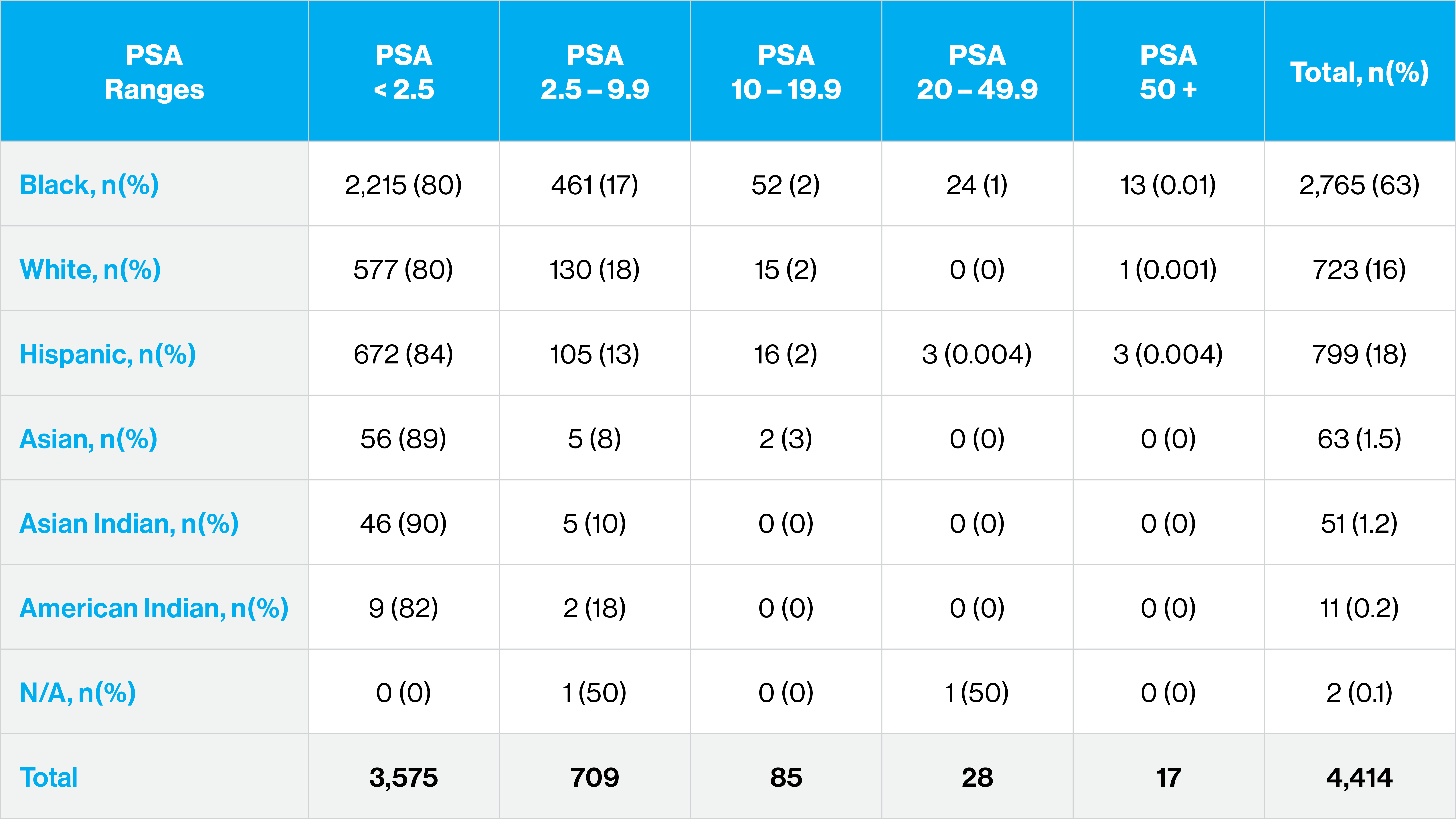
The mobile van was launched in 2022, and in its first year, more than 2,000 men were screened. Of those, 17 percent had an elevated PSA of 2.5 or above. After the second year, the total number of those screened has more than doubled to 4,400, with about 19 percent of the total showing an elevated PSA. They were referred for follow-up care with a urologist. Black men accounted for 63 percent of those screened.
Funded by a $3.8 million donation from philanthropist Robert F. Smith to support a proposal prepared by Dr. Tewari, the mobile unit is focused on educating men about the prostate while providing prostate cancer screening and referring for treatment when needed. The goal is to lower prostate cancer deaths by 25 percent among Black males in the areas immediately surrounding The Mount Sinai Hospital and Mount Sinai Queens.
“This van creates the opportunity for us to take world class physicians into all sorts of communities that may not have this access,” Mr. Smith said, as Mount Sinai and the Department honored him at the 2023 Prostate Cancer Research Gala for his role in the initiative. “I'm very hopeful this is going to be one of those sparks that leads to a platform of access to health care for the African American community, and saves lives.”

The mobile unit was envisioned and directed by Dr. Tewari, who wanted Mount Sinai clinicians to meet patients where they live.
“Our goal is that with increased education, awareness, and access to testing, we can help detect prostate cancer early, save lives, and close the gaps in high-risk diagnostic and fatality rates,” says Dr. Tewari, who is also Director of the Center of Excellence for Prostate Cancer at The Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai and Surgeon-in-Chief of the Tisch Cancer Hospital at The Mount Sinai Hospital. “The mobile van is succeeding at bringing doctors and the medical community closer to the patient.”
For example, in the last year, the Department bolstered outreach efforts by having research associates, who are members of the team, visit people at home to deliver the results of PSA tests, so they don’t need to rely on the mail or phone calls. The team is even working to provide mobile phones for those who may not have them in order to keep in touch.
Another benefit of these screenings is the team may find evidence of other medical conditions and refer people for appropriate treatment.
As part of the outreach effort, the Department’s multidisciplinary team continues to work with local churches, health centers, community groups, and attended events at local churches, street health expos, and charity events throughout New York City and beyond. The van goes to neighborhoods with high concentrated populations of Black men, providing access to education and screening for all in these areas.
Since its launch, the van has visited Harlem and parts of the Bronx, Brooklyn, Queens, and Long Island. It visits neighborhoods at least three days each week, including weekend days for the convenience of patients. At each visit, 25 to 30 men are screened.
Screening includes taking vital signs and PSA testing, and may extend to blood tests for infections, a bladder scan, EXACTVU micro ultrasound, rectal exam, and genomic testing. The mobile unit has testing equipment and a private room for physical examinations.

Screening includes taking vital signs and PSA testing, and may extend to blood tests for infections, a bladder scan, EXACTVU micro ultrasound, rectal exam, and genomic testing.
But the outreach—bringing state-of-the-art imaging equipment and specialized staff directly to the communities that need them most—is the true game-changing element of the initiative.
“We have to meet people where they are and provide them with the services they need. There are often very real barriers to taking a day off from work, finding childcare or parent care, to do health screening activities. So these kinds of programs are essential to eliminating disparities,” says Lynne Richardson, MD, Professor, Emergency Medicine, and Co-Director of Mount Sinai’s Institute for Health Equity Research.
Adds David Reich, MD, President of The Mount Sinai Hospital and Mount Sinai Queens: “We have to get out of the brick and mortar of our campus and be there for our community. Thanks to Robert Smith, we have not just the vision for that. Now we have the wherewithal, now we have the facility that brings care to the community.”
