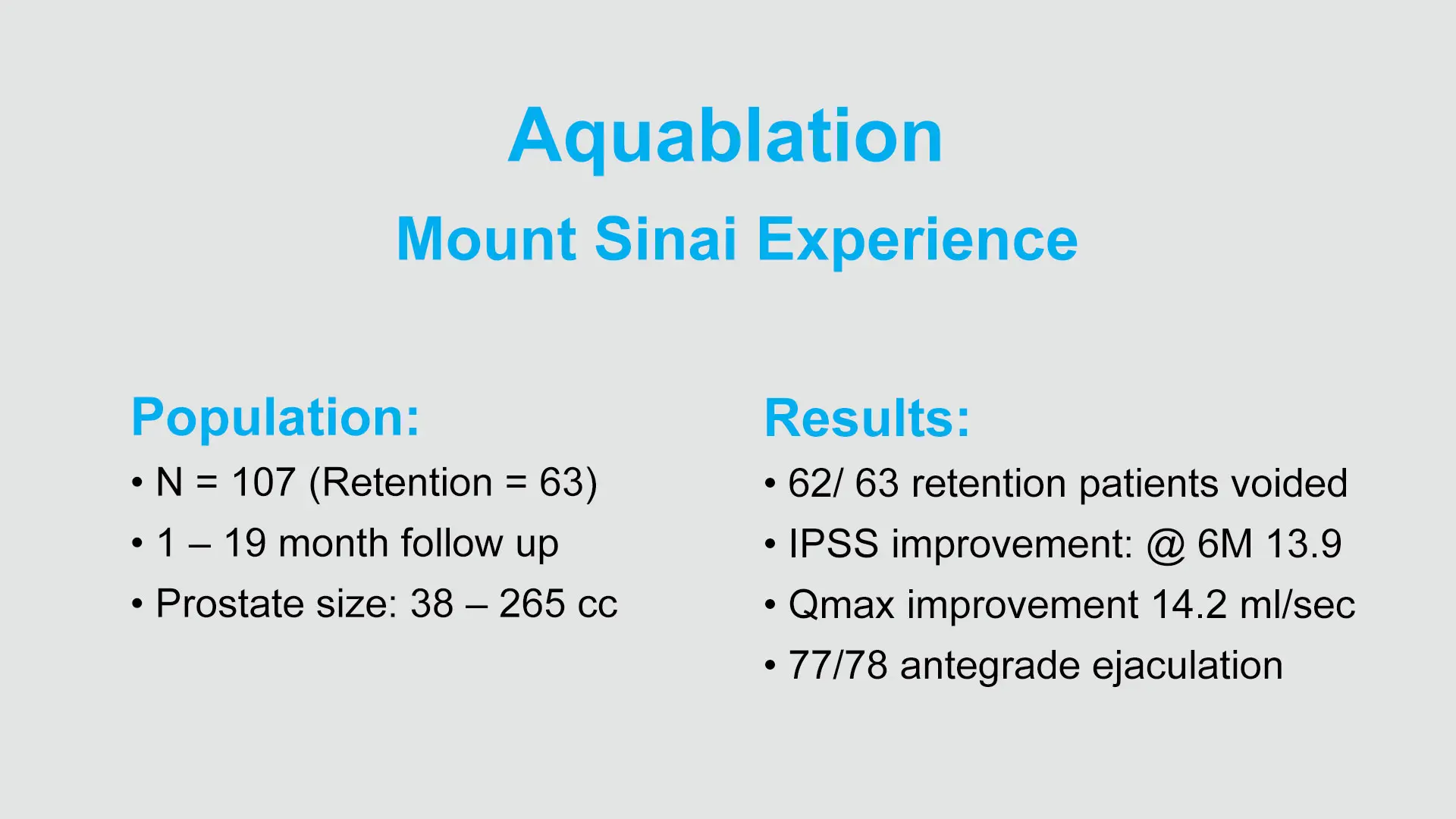
It used to take Steven A. Kaplan, MD, approximately 60 minutes to 90 minutes to treat patients presenting with benign prostatic hyperplasia (BPH) and a prostate of 80 grams or more using the transurethral resection of the prostate (TURP) procedure—the standard of care for BPH. But using Aquablation® therapy, he is able to treat patients presenting with similar size prostates in approximately eight minutes.
“The great thing about this procedure is that the size of the prostate almost doesn't matter,” says Dr. Kaplan, Professor of Urology at the Icahn School of Medicine at Mount Sinai and Director of the Men's Wellness Program, Mount Sinai Health System. “I have used it to treat prostates as large as 265 grams. I could not have done that using TURP or other transurethral methods, but this approach makes it possible.”
Steven A. Kaplan, MD, Professor of Urology at the Icahn School of Medicine at Mount Sinai and Director of the Men's Wellness Program, Mount Sinai Health System
A minimally invasive surgical procedure that combines a camera, ultrasound imaging, and a computer-controlled heat-free waterjet to enable efficient, precise removal of prostate tissue, Aquablation has proven to be a game changer in BPH treatment by enabling symptom relief with a low complication rate. Dr. Kaplan was one of the first surgeons to adopt the procedure, serving as one of the investigators in its clinical trials, and his program is the first of its kind in New York City.
“Mount Sinai was one of the first institutions to purchase the technology, but we only performed the procedure sporadically until it was covered by Medicare,” he says. “Since then, we have performed the procedure 105 times at a rate of approximately two to four aquablations each week, which is more than any other center on the East Coast.”
The Aquablation procedure involves the insertion of a waterjet handpiece into the patient’s penis and the placement of a transrectal ultrasound probe in the rectum. Once the instrumentation is set using computer software, it does not move, except for the waterjet nozzle, which means that any surgeon could potentially achieve the same results regardless of how many times they have performed the procedure. Because it is minimally invasive, it also eliminates the risk of patients experiencing retrograde ejaculation.
“Essentially, the procedure is like a three-dimensional TURP, because you can see everything inside visually and outside using the ultrasound,” Dr. Kaplan says. “That enables better targeting of the areas you want to treat, and thus enables preservation of ejaculation and sexual function among patients along with a faster healing process.”
Dr. Kaplan says there are virtually no contraindications for the procedure, which he says is essentially like power washing away the prostate. However, in the case of smaller prostate enlargements, he typically opts to perform a TURP as the advantages of Aquablation may not be needed.
Outcomes among his patients who have undergone Aquablation have been predominately positive, with only one case requiring transfusion—a rate that is consistent with available data. He adds that acceptance of the procedure among patients has also been high, with approximately 20 percent of all cases performed being the result of patients who sought him out based on online research. The biggest barrier so far has been the willingness of insurance companies to cover the procedure.
As his Aquablation program continues to grow, Dr. Kaplan has turned his attention to training others in the procedure and the development of preceptorship programs at Icahn Mount Sinai and through teaching it to colleagues nationwide. He is exploring opportunities to enhance the efficiency and durability of the instrumentation to achieve improved outcomes among patients.
Currently, two-thirds of patients who undergo the procedure are discharged the next day; his goal is to have the majority discharged the same day. Dr. Kaplan is also interested in researching whether the outcomes of the procedure are different for underrepresented populations, but he does not anticipate any disparity-related issues based on experience to date.
“This technology is agnostic,” he says. “That said, it may be that different patients may experience different outcomes related to different disease states, and we will be looking at that data to confirm whether that is the case.”