Although advances in robotic prostatectomy surgery over the past 20 years have reduced the incidence of urinary incontinence among patients from approximately 20 percent to 1 percent nationwide, the risk of erectile dysfunction remains considerably high—between 50 percent and 80 percent. Mani Menon, MD, a pioneer in the field of robotic prostate surgery who has performed more than 6,000 surgeries, decided to change that.
“The nerves that we need to preserve for maintenance of erectile function are much more complex than the nerves that we need to preserve for urinary continence,” says Dr. Menon, Chief of Strategy and Innovation in the Department of Urology for the Mount Sinai Health System. “I decided to explore the possibility of improving nerve sparing, and I realized that if we can preserve the capsule of the prostate, then we can spare patients erectile dysfunction.”
Having developed many of the techniques that helped reduce the risk of urinary incontinence in partnership with Ash Tewari, MBBS, MCh, Professor and Chair, Milton and Carroll Petrie Department of Urology, and the Kyung Hyun Kim, MD, Chair in Urology at the Icahn School of Medicine at Mount Sinai, Dr. Menon has further revolutionized the field through the development of the Menon precision prostatectomy (MPP). This novel approach to prostatectomy maximizes nerve sparing, resulting in an earlier return to urinary continence and erectile function among patients.
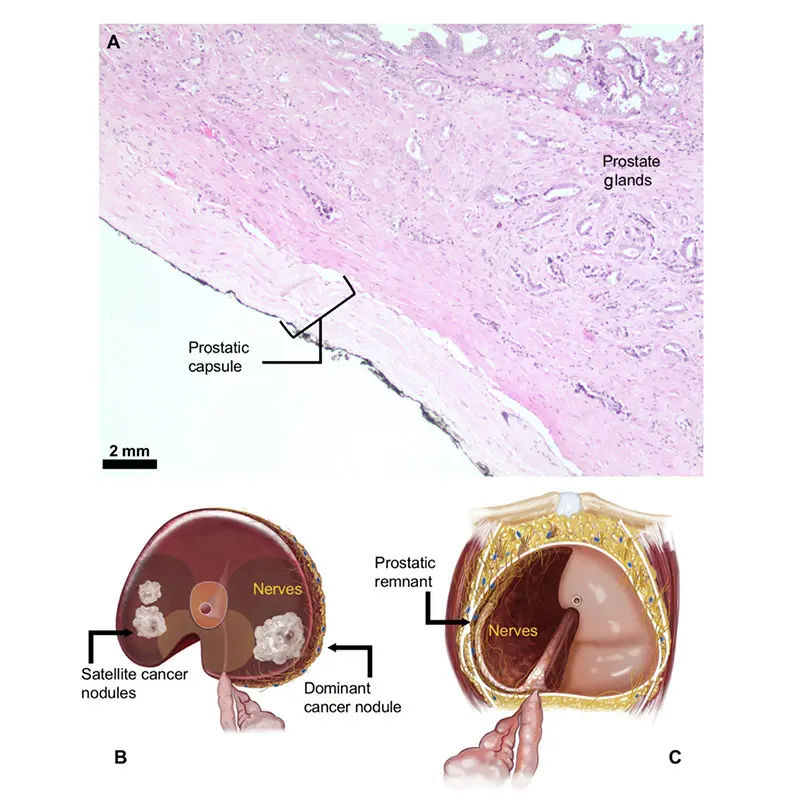
Image A shows the prostate capsule under a light microscope, the layer in which many nerves critical for erection travel; Image B shows the removed specimen during the operation; Image C shows what is left behind, the remnant with the critically important erectile nerves.
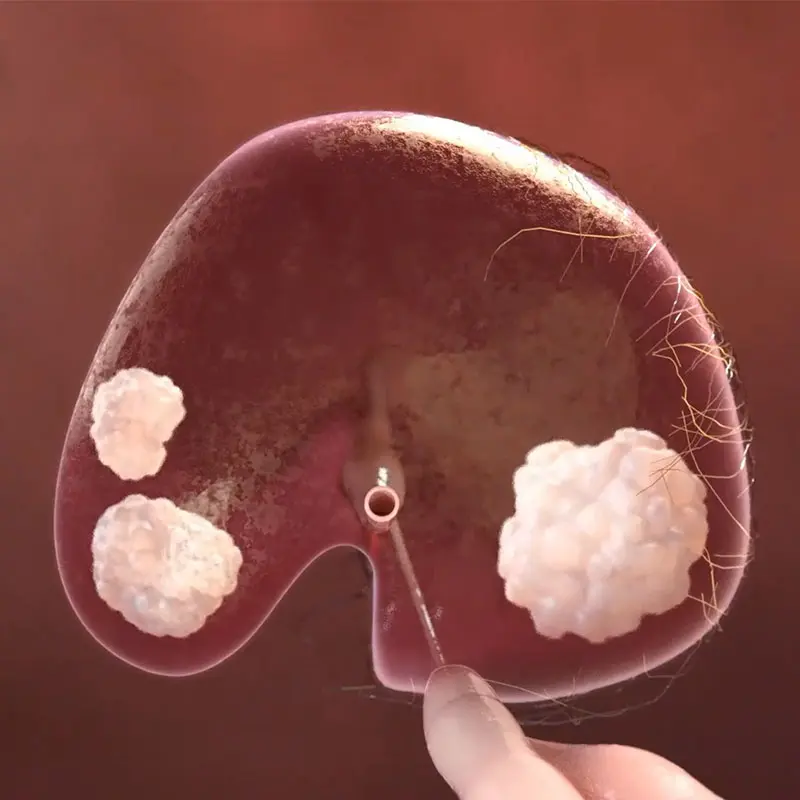
This image shows the removed specimen during the operation.
The concept for MPP is similar to that of skin-sparing surgery for breast cancer or a partial nephrectomy, in which the tumor is removed but not the entire breast or kidney. Dr. Menon performs a traditional radical prostatectomy on the side of the prostate with the visualized or dominant lesion, staying outside the prostate capsule and seminal vesicles. On the opposite side, where there is no lesion detected by an MRI and a real-time intraoperative biopsy does not detect cancer cells in the capsular tissue, he preserves a 4-to-7-millimeter rim of tissue, the seminal vesicle, the prostate capsule, and the tissue between the seminal vesicle and the prostate. It is this critical step that makes the approach a precision procedure and the spared tissue helps protect the network of thousands of microscopic nerves involved in erectile function.
Dr. Menon says eligibility for the procedure is based upon a Gleason score of 3+4 or 4+3, a prostate-specific antigen (PSA) less than 20ng/ml, and the patient’s desire to maintain erectile function, which means that approximately 80 percent of patients with prostate cancer qualify for MPP. Given that the procedure leaves behind cells that will continue to produce small amounts of PSA, patients who undergo the procedure are followed with PSA testing every three months for the first two years, then every six months from year three to year five, and once a year after that.
Data from the first 50 patients who underwent MPP between December 2016 and March 2018 show that, at 1 to 12 months, the median PSA value was below 1ng/ml (0.6), and in 50 percent of patients, the PSA was undetectable. Patients who have a PSA of 0.4 will undergo a biopsy, and if it is positive for cancer, further treatment will be recommended, such as removal of residual tissue, radiation, or tissue ablation.
Additional data from the first 50 patients who underwent MPP show that approximately 90 percent achieved erections sufficient for intercourse and 80 percent regained urinary control within one month of surgery. By the fourth month, approximately 90 percent had regained urinary control, and by the eighth month, 100 percent regained urinary control. That data, Dr. Menon says, demonstrate that MPP results in superior return of erectile function versus conventional nerve-sparing radical prostatectomy.
“I have performed the procedure 120 times and have found that it works 95 percent of the time,” says Dr. Menon, who also serves as Professor of Urology, Director of Education, and Director of the Precision Prostatectomy Program in the Department of Urology at Icahn Mount Sinai and the Center of Excellence for Prostate Cancer at The Tisch Cancer Institute. “In 5 percent of cases, the tumor was missed, and we had to retreat patients approximately one year after the first treatment. But the result for maintenance of potency is approximately 90 percent to 95 percent at one year,” he says.
Prior to joining Mount Sinai in 2021, Dr. Menon used three-dimensional (3D) software to conduct tumor biopsies. He is in the process of acquiring that software for Mount Sinai but is also exploring the potential of using micro-ultrasound to identify candidates.
“The micro-ultrasound is comparable to a 3D biopsy, which was able to achieve a 95 percent success rate in detecting clinically significant cancer,” he says. “The difference is that it would have to be done at the time of surgery. I am looking at the potential of using this technology to bring the incidence of missed cancers down to 2 percent.”
Dr. Menon will also be collaborating with Dr. Tewari to determine if molecular testing could further enhance the effort to detect patients with clinically significant cancer. For now, the main goal is to raise awareness among candidates that the procedure is available through Mount Sinai, that it can preserve urinary continence and erectile function, and that it is safe.
“When I first started doing the procedure, 60 percent of patients were uncomfortable about it,” Dr. Menon says. “By the end of four years, it was 40 percent. I think, in five years, it will be 20 percent as more patients become aware of MPP and how it can preserve both their urinary and erectile function and their quality of life.”
Featured
Mani Menon, MD
Chief of Strategy and Innovation in the Department of Urology for the Mount Sinai Health System
