A review of data from around the world by Mount Sinai researchers confirms that men face a greater risk of infection and mortality from COVID-19 and that routine screening should be conducted for the disease among prostate cancer patients.
The review, “Sex differences in SARS-CoV-2 infection rates and the potential link to prostate cancer,” was conducted to understand the epidemiological and biological evidence for gender and/or sex disparity in COVID-19, the potential association between COVID-19 and prostate cancer molecular pathogenesis, and current therapeutic options for COVID-19 patients and, in particular, COVID-19 patients with prostate cancer. It was published July 2020 in Communications Biology.
“We know that COVID-19 uses two specific receptors to enter cells and replicate—angiotensin-converting enzyme 2 (ACE2) and transmembrane protein, serine 2 (TMPRSS2),” says Ash Tewari, MBBS, MCh, Professor and Chair of the Department of Urology and Senior
Author of the study. “It is common knowledge that TMPRSS2 is highly expressed in prostate cancer. Based on that, we were interested in determining if prostate cancer patients were more susceptible to COVID-19 infection.”
The research team noted that androgens such as testosterone appear to enhance the ability of the COVID-19 virus to enter cells and replicate. “Testosterone has an immune suppressive role among males whereas women have estrogen that is considered to be immune protective,” says Sujit S. Nair, PhD, Assistant Professor of Urology and Director of Genitourinary Immunotherapy Research at the Icahn School of Medicine at Mount Sinai, and one of the authors. “Testosterone also has several other effects by which it suppresses the immune response, so the virus seems to be more active and more aggressive in men.”
Given that testosterone also drives TMPRSS2 expression, and the fact that the receptor is highly expressed in both COVID-19 and prostate cancer, the research team hypothesized that these issues may be related—more androgens could signify greater expression of TMPRSS2 and thus patients with prostate cancer are more susceptible to the virus.
“It was striking to note that TMPRSS2 was a key factor in both diseases,” says lead author
Dimple Chakravarty, PhD, Assistant Professor of Urology at the Icahn School of Medicine. “As we looked at all the different risk factors, it made us more confident that there is a connection between the two.”
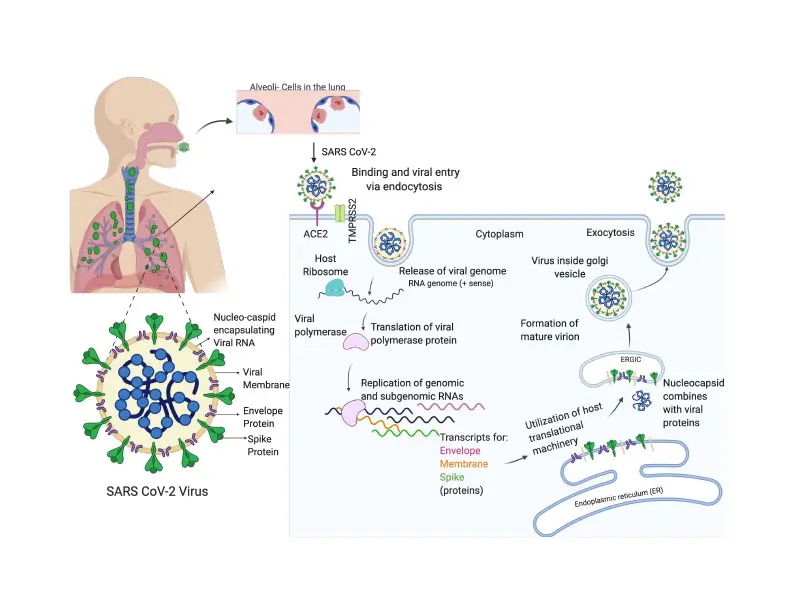
Molecular drivers of SARS-CoV-2 productive infection
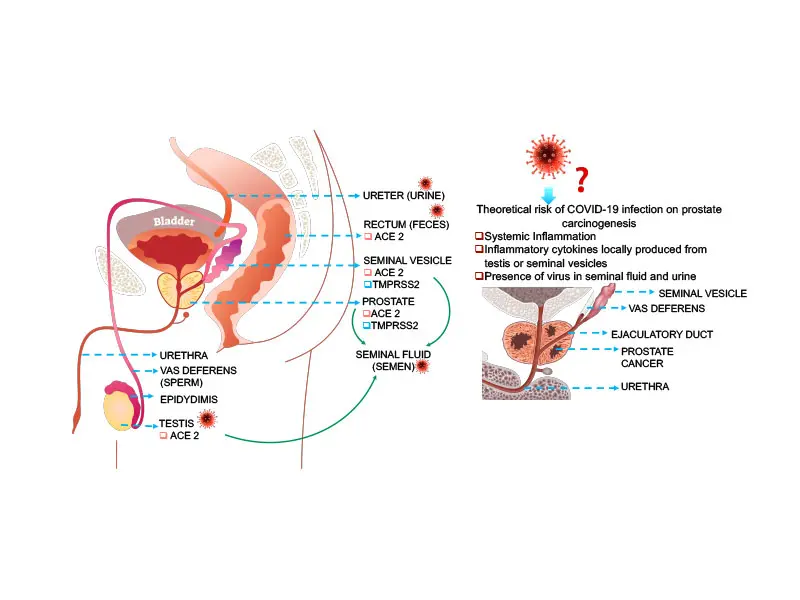
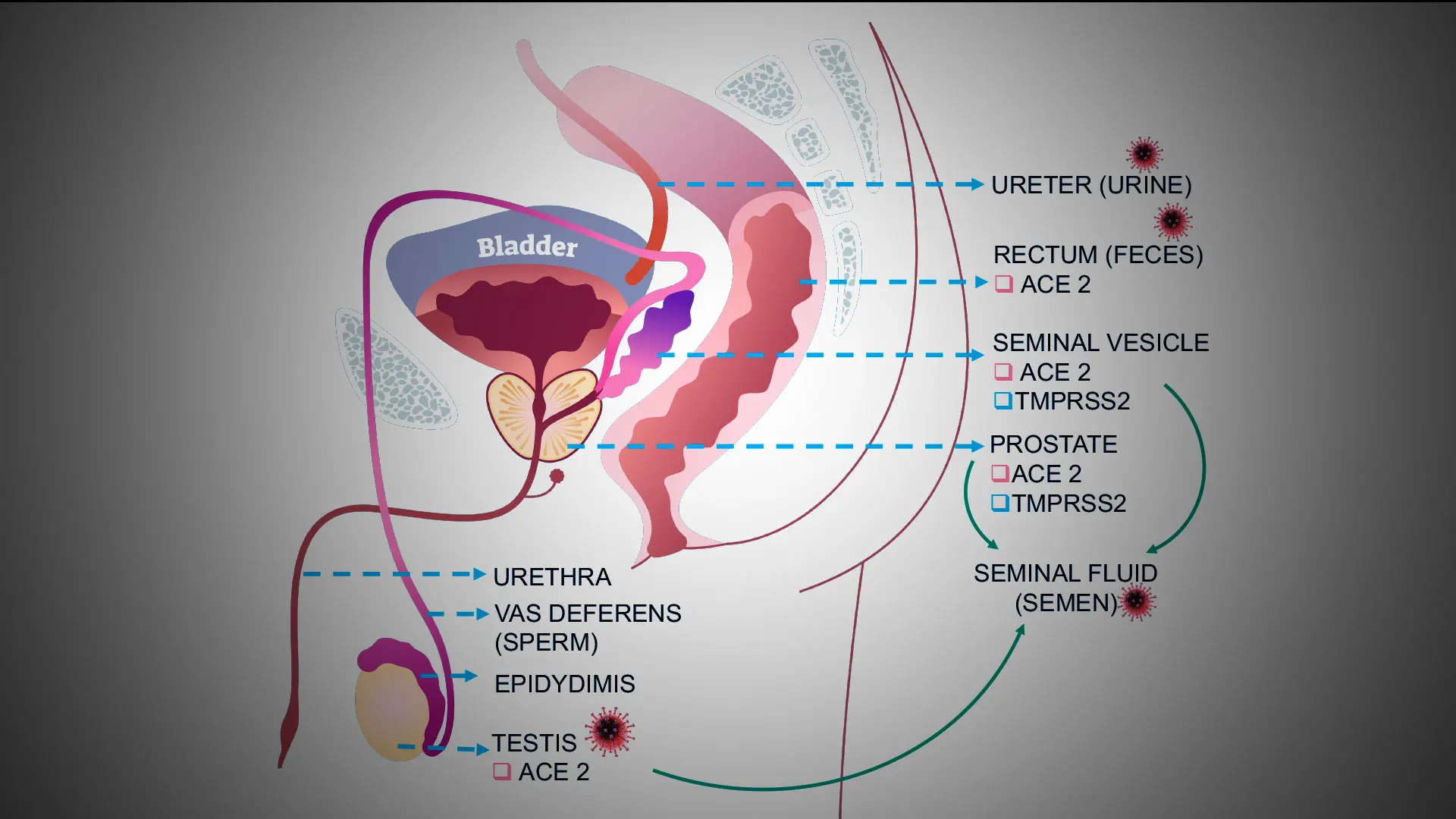
Graphical representation of the theoretical risks and potential routes of dissemination of SARS-CoV-2 to the prostate.
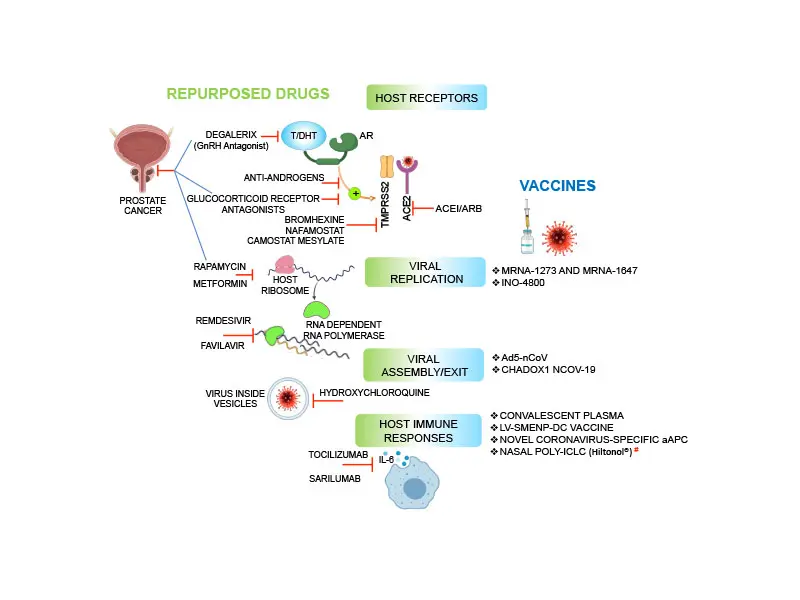
Major drugs and vaccines for COVID-19.Illustration summarizes potential drugs and vaccines for COVID-19 that target either host receptors, viral replication, virus assembly, or host immune response.
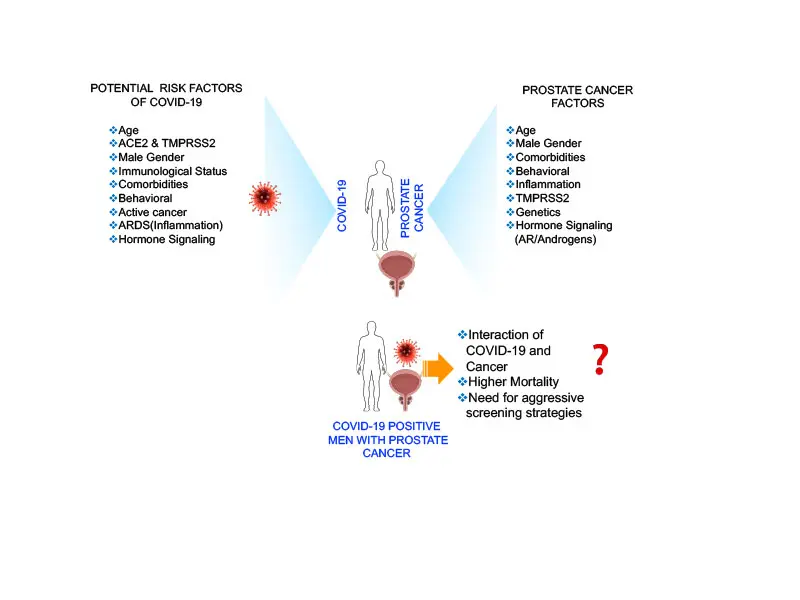
Comparison of Risk factors between COVID-19 and prostate cancer.
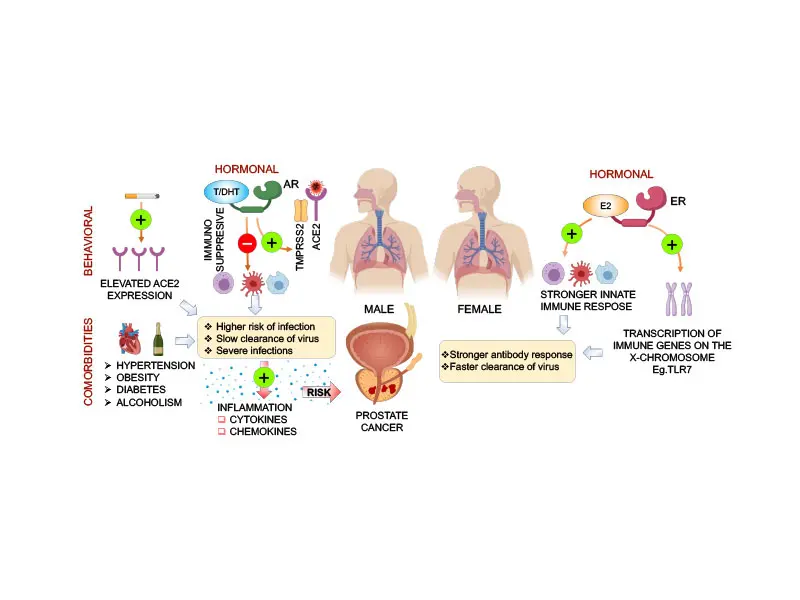
Sex differences in COVID-19. Illustration highlights potential biological (hormone signaling, immunological) and behavioral differences between males and females that contribute to sex divergence in response to SARS-CoV-2.
Among risk factors cited in the review, prostate cancer patients belong to the age group that is more susceptible to COVID-19 infection and are at higher risk of developing severe illness due to the underlying cancer weakening their immune system.
Furthermore, approximately 18 percent of prostate cancer patients have multiple comorbid conditions such as hypertension, cardiovascular disease, diabetes, and obesity, that increase the risks associated with COVID-19 infection, with males demonstrating higher rates of comorbidities than females globally. Researchers also noted there are behavioral issues that may also increase risk for males, such as greater rates of smoking.
“When you combine age, comorbidities, and testosterone as a driver of TMPRSS2 expression, that creates a very dangerous situation,” Dr. Nair says. “For these reasons, we recommend routine COVID-19 screening among patients with prostate cancer.”
Having completed this review, Drs. Chakravarty and Nair are conducting further studies to gain a better understanding as to why men with prostate cancer are at increased risk for COVID-19 infection and the clinical impact of infection on the underlying cancer.
For example, there are plans for a clinical trial to test a novel immune modulator in prostate cancer patients over age 40 who have COVID-19 and for a study collecting blood samples from all GU patients to see if those with cancer have a higher rate of infection with COVID-19.
“We have papers under review that are looking at the significance of antiandrogens among patients with COVID-19 and exploring racial disparities in COVID-19 infection,” Dr. Chakravarty says. “Interestingly, the same disparity in COVID-19 infections exists in prostate cancer, so our goal is to see whether there are common factors that inform these disparities and then identify targets to tackle them.”
The other authors of the study are: Parita Ratnani, Data Manager/Biostatistician, Urology; Yasmine Gharib, Clinical Research Coordinator, Urology; Vinayak Wagaskar, MCh, Urologic Oncology Fellow; Nihal Mohamed, PhD, Associate Professor, Urology; Dara Lundon, MD, PhD, MBA, Director, Clinical Trials and Innovation; Zachary Dovey, MBB, Director of Uro-Oncology Services, Urology; Natasha Kyprianou, MBBS, PhD, Professor of Urology, Pathology and Oncological Sciences; and Nada Hammouda, MS, Physician Researcher and Data Analyst, Department of Emergency Medicine.
Featured

Ash Tewari, MBBS, MCh, FRCS (Hon.)
Professor and System Chair, Milton and Carroll Petrie Department of Urology, Director of the Center of Excellence for Prostate Cancer at The Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai, and Surgeon-in-Chief of the Tisch Cancer Hospital at The Mount Sinai Hospital

Sujit S. Nair, PhD
Assistant Professor of Urology and Director of Genitourinary Immunotherapy Research

Dimple Chakravarty, PhD
Assistant Professor of Urology