A review of COVID-19 literature by Mount Sinai researchers has identified an overlap between the biomarkers of the virus and renal cell carcinoma (RCC), and that could enable effective simultaneous treatment of both diseases.
Published in September 2020 in European Urology Focus, the review, “COVID-19 and Kidney Disease: Molecular Determinants and Clinical Implications in Renal Cancer,” explores whether the high presence of angiotensin-converting enzyme 2 (ACE2) in the kidney contributes to COVID-19 infection among patients with kidney disease.
“Structural spike proteins drive entry of the virus into target host cells by engaging ACE2,” says Natasha Kyprianou, MBBS, PhD, Professor of Urology, and Oncological Sciences and Vice Chair of Basic Science Research, Urology, at the Icahn School of Medicine at Mount Sinai, the senior author. “Given that ACE2 is expressed on podocytes and the border of the proximal tubule cells of the kidney, there is an easy route of infection for the viral particles at this site. Our goal was to analyze the impact of COVID-19 on the kidney and RCC and assess potential therapeutic targeting for RCC patients with COVID-19.”
The researchers observed that 74.8 percent of COVID-19 patients who were hospitalized with an underlying condition had chronic renal disease, but these patients accounted for 3 percent of all COVID-19 cases.
Moreover, a notable percentage of patients hospitalized with COVID-19 had proteinuria (43.9 percent), hematuria (26.7 percent), and elevated serum creatinine, elevated blood urea nitrogen, and estimated glomerular filtration rate under 60 ml/min (13-14 percent). The incidence of acute kidney injury was significantly higher among patients with elevated baseline serum creatinine, and the in-hospital mortality rate among these patients was 33.7 percent, which was significantly higher than that among patients with normal creatinine levels.
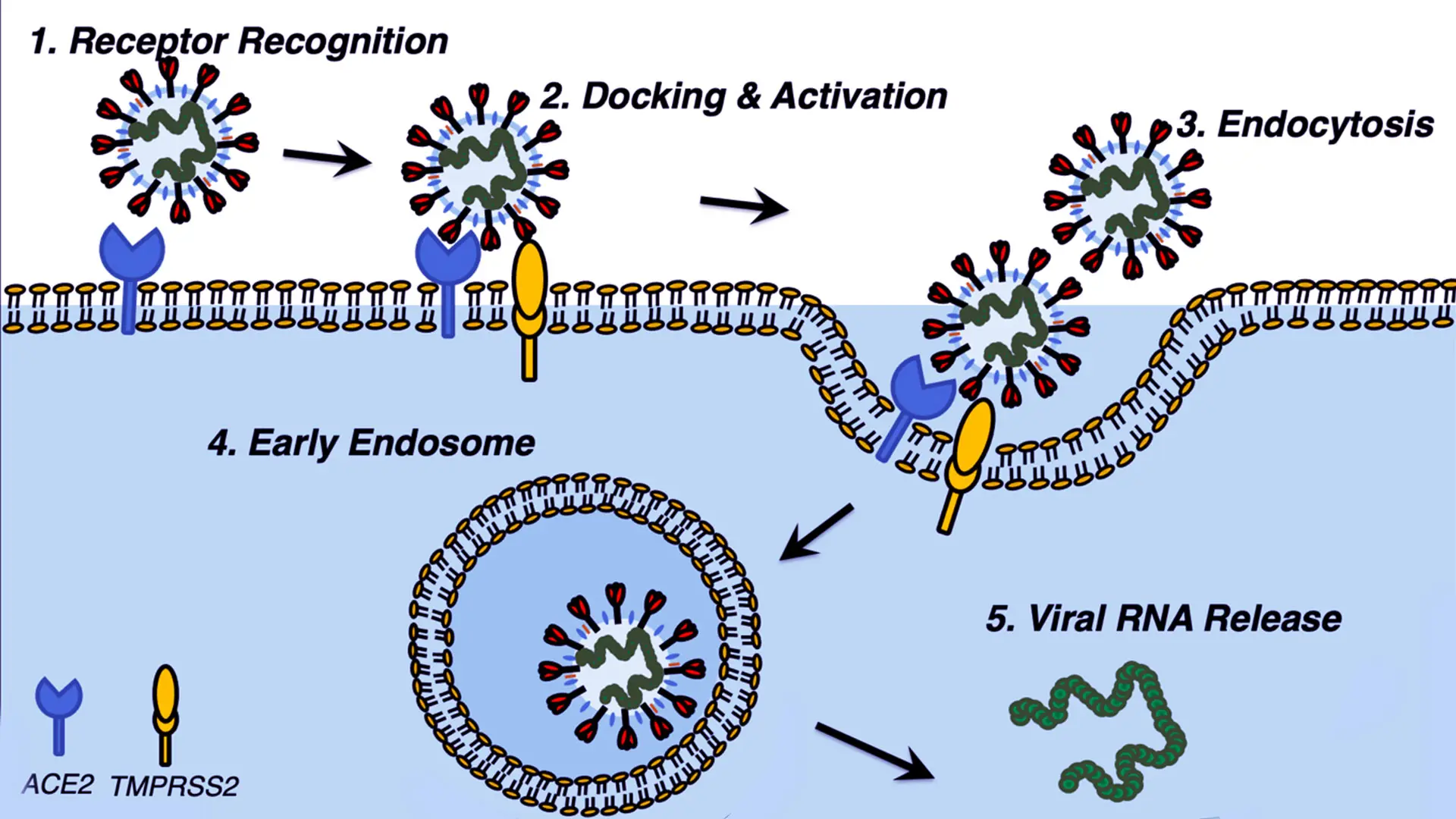
Molecular pathway of SARS-CoV-2 activation in host cells. Illustration credit: Navneet Dogra, PhD
However, the researchers also noted that patients with COVID-19 who were being administered maintenance hemodialysis had less lymphopenia, lower serum levels of inflammatory cytokines, and milder clinical disease compared to other COVID-19 patients. As a result, they recommend that dialysis patients who have been infected with COVID-19 should continue their current therapeutic regime and do so at their current center to reduce risk of exposure for other patients and health care workers.
Reviewing liquid biopsies of blood from patients with COVID-19, the researchers noted the presence of viral exosome RNA in the blood, which could be correlated in the subset of patients who also had renal cancer. They also observed the elevated presence of RNA biomarkers that are specifically associated with cancer—carbonic anhydrase IX (CAIX) and ceruloplasmin.
“Not only were these renal cancer-associated markers elevated among patients with COVID-19, they were also associated with higher mortality, which suggests they are a mechanism of severe kidney disease in COVID-19-infected patients,” Dr. Kyprianou says. The researchers are the first to identify this association.
This association, Dr. Kyprianou hypothesizes, could be the result of inflammation caused by ACE2. “We know there is a strong pathological link between inflammation in various organs and cancer development,” Dr. Kyprianou says. “Thus, if we understand the mechanisms of inflammation, we can identify markers for detection and therapeutic targets.”
In assessing therapeutic management of renal cell carcinoma and COVID-19, the researchers noted that kidney cancer patients who are being administered immune checkpoint inhibitors demonstrated better COVID-19-related outcomes than patients who are immunosuppressed from chemotherapy.
At the same time, potential pneumological toxicity from anti-PD-1/PD-LI ICI agents may worsen interstitial pneumonia. There are promising indicators that tocilizumab, a monoclonal antibody against the interleukin-6 receptor, may serve as a neutralizing antibody against the COVID-19 spike protein.
The researchers also noted that ACE inhibitors cause an increase in ACE2 receptors and less competitive inhibition for SARS-CoV-2 binding, and that endothelin receptor antagonists may be better suited for those with hypertension as the therapy does not enhance the viral binding capability of SARS-CoV-2. Glucocorticoids, which improved outcomes for patients with Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), also appear to have promise, but only when administered in low dosages.
“That is exciting because it means there are FDA-approved therapeutic management options available now that we can administer to patients with kidney disease who are infected with COVID-19 and potentially target and eradicate both diseases,” Dr. Kyprianou says.
Further studies are necessary, but Dr. Kyprianou believes that ACE2 expression in the kidney, particularly in cases involving renal cell carcinoma, will result in new targets for therapeutic treatment. She also anticipates that continued study of extracellular vesicles, circulating tumor cells, biomarkers, and the genomic landscape of renal cell carcinoma and COVID-19 will result in further insights into the impact of viral damage on kidney function and RCC.
“The future exploration will rely on whole-blood, whole-urine genomics to define the intertwined genomic landscape among RCC and COVID-19-positive patients and the downstream effect of viral damage on renal function,” she says. “Liquid biopsy could be the most effective tool for early identification, intervention, and improved prognosis among RCC patients harboring SARS-CoV-2 infection.”
The other authors of the study from Mount Sinai are: Meredith Mihalopoulos, medical student, Icahn School of Medicine at Mount Sinai; Navneet Dogra, PhD, Assistant Professor, Genetics and Genomic Sciences, and Pathology, Molecular and Cell Based Medicine; Nihal Mohamed, PhD, Associate Professor, Urology; and Ketan Badani, MD, Professor, Urology, and Vice Chair of Urology and Robotic Operations for the Mount Sinai Health System.
Featured

Natasha Kyprianou, MBBS, PhD
Professor of Urology, and Oncological Sciences and Vice Chair of Basic Science Research, Urology