Traditionally, the approach toward patients who present with staghorn calculi has started and ended with surgery.
Mount Sinai has developed a more comprehensive, patient-centered approach to care that is focused on understanding the root causes of the disease by pioneering new treatments and developing customized postoperative regimens that reduce the risk of redevelopment, resulting in improved outcomes.
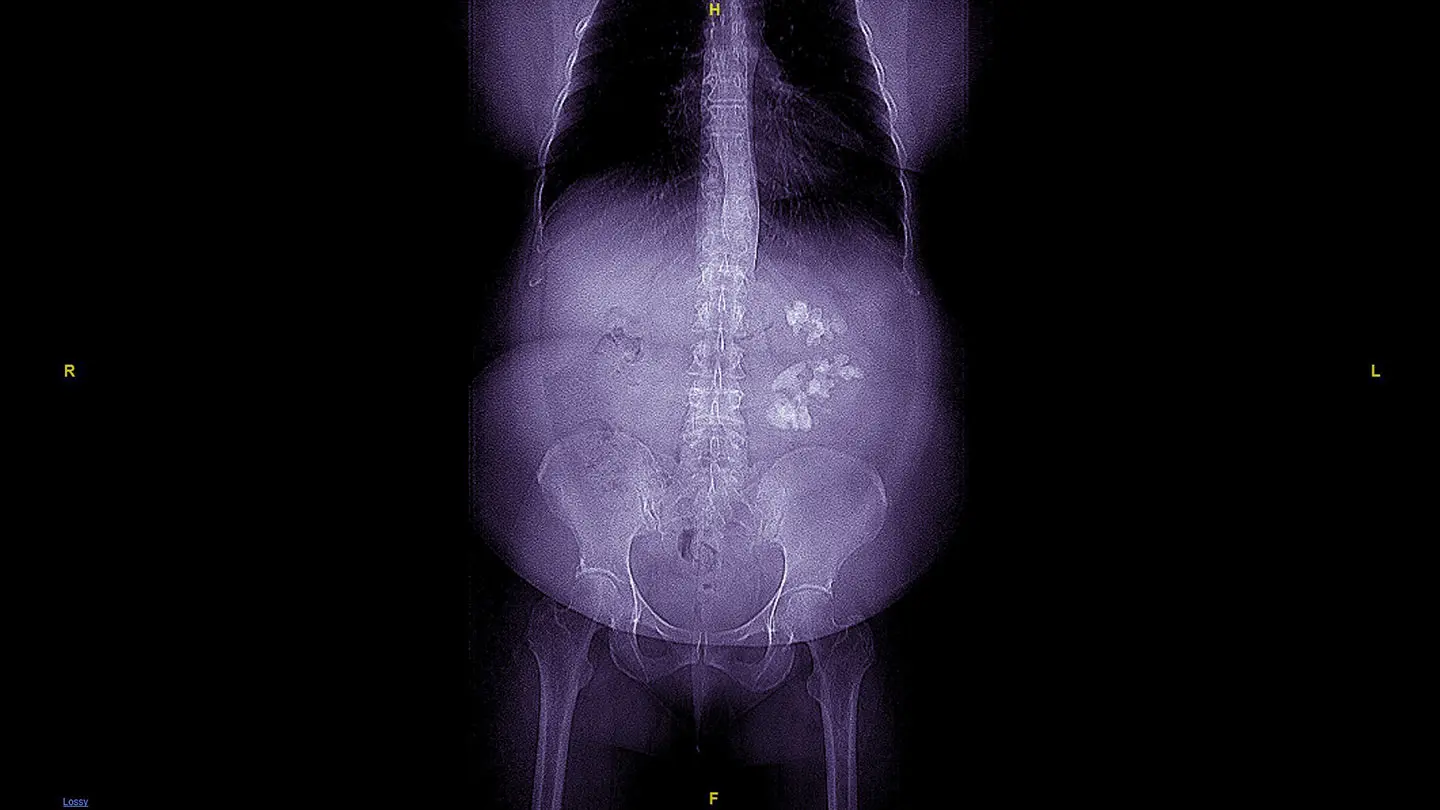
Patients who present with staghorn calculi first undergo a full imaging workup with a computed tomography (CT) scan to determine the position of the kidney relative to their major organs and ribs and thus mitigate the risk of complications such as a fistula or pneumothorax, according to Mantu Gupta, MD, Professor of Urology at the Icahn School of Medicine at Mount Sinai. The CT scan also facilitates three-dimensional (3D) reconstructed imaging of the kidney, enabling Dr. Gupta to ascertain the shape of the staghorn calculi and plan the best surgical approach.
Once done, Dr. Gupta performs percutaneous nephrolithotomy (PCNL) using ultrasound, a modality he pioneered, which enables real-time 3D imaging of the kidney and surrounding organs. The result is a more precise needle trajectory than possible using fluoroscopy, which enables him to perform the procedure without the use of nephrostomy tubes.
“This minimally invasive modality does not traverse blood vessels, so it eliminates the requirement for a nephrostomy tube to drain the kidney and tamponade bleeding,” says Dr. Gupta, who is also Site Chair of Urology at Mount Sinai West and Mount Sinai Morningside. “Instead, we use a catheter or a stent from below, which means patients experience significantly less pain.”
"By looking at the root causes for staghorn calculi development in each patient, we are able to develop customized interventions that reduce their risk for redevelopment."
-Mantu Gupta, MD
The ultrasound modality has also enabled Dr. Gupta to perform PCNL with one track dilated to 24 French in complex cases, but in less complex cases, he is able to remove the staghorn calculi using a mini PCNL approach with 16 French dilation.
“Traditionally 30 French was used because it created more room for irrigation, enabling the removal of larger pieces of stone,” Dr. Gupta says. “Now that we have specialized high-power lasers, we can get the job done effectively using a smaller track, which is beneficial for patients because the incision is small enough that it can be sealed with glue instead of sutures.”
These surgical innovations have resulted in enhanced recovery times for patients who present with staghorn calculi at Mount Sinai. Approximately 95 percent of patients are discharged within 23 hours of surgery, which compares favorably with the national average of two days. In addition, the prevalence of postoperative complications such as pseudoaneurysm is 0.5 percent versus the national average of 2 percent.
Surgical innovations resulted in enhanced recovery times for patients
95 percent of patients discharged within 23 hours of surgery
As for long-term outcomes, patients undergo an X-ray or ultrasound following the procedure to ensure there are no residual staghorn calculi, issues with kidney function, or swelling of the kidney. Samples are also extracted from their staghorn calculi for further analysis to determine if the etiology was infection or metabolic.
In cases involving an infection etiology, patients are administered a low-dose regimen of antibiotics lasting several months. In cases involving a metabolic etiology, Dr. Gupta conducts a 24-hour urine analysis to assess pH volume and the presence of minerals such as calcium, phosphorus, and oxalate. Based on his findings, Dr. Gupta develops a customized treatment regimen that could include changes in lifestyle or referral to a nephrologist.
“There is a significant risk for redevelopment of staghorn among patients who have undergone PCNL,” Dr. Gupta says. “That is why we go beyond getting patients back to their lives as quickly as possible. By looking at the root causes for staghorn calculi development in each patient, we are able to develop customized interventions that reduce their risk for redevelopment. We then follow up every three months with consultations for the first year or two, monitoring their urine tests for any sign of staghorn calculi redevelopment. It is this long-term approach that sets us apart when it comes to achieving positive patient outcomes.”
In addition to surgical and therapeutic innovation, Mount Sinai is also making progress in researching the factors that cause staghorn calculi, an effort that has been facilitated by the development of a comprehensive patient database.
One study, published in 2019, looked at 24-hour urine analyses to see if there were any discernable differences between patients who developed staghorn calculi and those who developed regular kidney stones.
“We found no difference between the two cohorts,” Dr. Gupta says. “Based on those findings, we are now performing biopsies of the papilla from staghorn and non-staghorn patients to see if there are differences in the protein profile or enzyme profile that might explain this branching phenomenon and thus offer a target for treatment, such as an antibody or an inhibitor.”
In the meantime, Dr. Gupta continues to advance surgical modalities for the benefit of patients. He is pioneering a supine approach to PCNL that will eliminate the need for intubation, which will mean less stress to the patient’s lungs and improved recovery times.
“Through all these efforts and advances, we are getting better, not just in terms of the treatment we are able to offer patients but also in our efforts to uncover the root causes of staghorn calculi,” he says. “For that reason, I believe the future is very bright both for our patients at Mount Sinai and for all patients with staghorn calculi.”

A cut measuring less than one centimeter in the back is made on the side of the affected kidney, and a protective sheath is inserted.
Featured

Mantu Gupta, MD
Professor of Urology, the Icahn School of Medicine at Mount Sinai