The human immune system is theorized to provide protective functions against cancer, but clinical evidence of that is lacking. A breakthrough study led by researchers from the Icahn School of Medicine at Mount Sinai sheds valuable light on the debate of the role of genetics in cancer-risk assessment and causation, specifically in lung cancer.
The team’s findings suggest that genetic variation in immunosurveillance is a key cancer risk factor. Specifically, human leukocyte antigen-II (HLA-II) heterozygosity is associated with reduced risk of developing lung cancer, with particular benefits to smokers. The implications of this research, published in Science, extend beyond lung cancer as researchers seek to develop more effective detection and prevention strategies to combat various forms of cancer.
“We’re helping to advance the field’s traditional understanding of cancer risk as the product of random somatic mutations arising during DNA replication, inherited genetic variability, and environmental factors,” says senior co-author Diego Chowell, PhD, Assistant Professor of Artificial Intelligence and Human Health, and Oncological Sciences, at the Icahn School. “Our findings offer a fresh perspective on the role of the host immune system in cancer risk and will hopefully inspire the inclusion of immunogenetics into lung cancer screening programs.”

Diego Chowell, PhD, Assistant Professor of Artificial Intelligence and Human Health, and Oncological Sciences (left), and Robert Samstein, MD, PhD, Assistant Professor of Radiation Oncology (right), have found that human leukocyte antigen (HLA) polymorphisms can reduce the risk of lung cancer. Their findings add evidence to the theory that the host immune system plays a role in preventing cancer, and can potentially be extrapolated to other cancer types as well.
By focusing on human leukocyte antigens, the research team brought to center stage the most diverse genes in the human body that are at the core of immune recognition. The role of these molecules is to present foreign antigens on the cell surface and thus assist the immune system in identifying and eliminating threats, such as malignancies and pathogens. The HLA heterozygote “advantage” theory in cancer immunosurveillance proposed by investigators is based on the fact that individuals with heterozygosity have different versions of HLA genes, and that HLA-II genes (but not HLA-I) help smokers by presenting to the immune system a more diverse antigenic peptide repertoire, resulting in superior immune system control of cancerous cells.
The research team comprises Mount Sinai; the University of Helsinki; Boston institutions Massachusetts General Hospital and the Broad Institute of MIT and Harvard; the Vall d’Hebron Institute of Oncology in Barcelona; and the Hartwig Medical Foundation in Amsterdam. They analyzed two large population-level datasets, one from the UK Biobank and the other from Finland’s FinnGen.

Drs. Chowell and Samstein tested the hypothesis that two different HLA allomorphs will present more neoplastic antigens than will a single HLA allomorph, thus increasing the likelihood of a cytotoxic reaction against mutated neoplastic cells. They performed clinical, genetic, environmental, and longitudinal analyses on two large-scale population cohorts: the UK Biobank and FinnGen, totaling more than 570,000 individuals.

In the findings, current and former smokers who had heterozygous HLA-II loci saw a significant reduction in lung cancer risk compared to those with homozygous loci. There was no significant difference in lung cancer risk for those who had never smoked, regardless of heterozygosity. This suggests a possible interaction between HLA-II heterozygosity and smoking in driving lung cancer risk.
What these scientists found from their genetic epidemiology and multimodal genomic analysis was that heterozygosity at the HLA-II level was linked to reduced risk of lung cancer over more than a decade of participant follow-up. Interestingly, that protective effect was observed in both current and former smokers, but not in those who had never smoked, suggesting that smoking-derived antigens may augment the immune response in early-stage disease.
“Furthermore, we learned that adding to our analysis polygenic risk scores—which are a measure of genetic predisposition based on multiple genes—increased the lifetime risk of lung cancer, specifically in smokers who had identical versions of the HLA-II alleles,” explains Dr. Chowell, whose lab works at the intersection of cancer genomics, immunology, and computational biology.
According to senior co-author Robert Samstein, MD, PhD, Assistant Professor of Radiation Oncology at the Icahn School, the net effect of the team’s findings is to highlight a previously overlooked aspect of cancer-risk assessment. “Our study marks a major step toward understanding the intricate interplay between the immune system and cancer risk,” he elaborates. “We hope that by identifying individuals with increased susceptibility based on their immune genetics, we can implement more targeted screening, prevention, and treatment strategies.”
The next step for researchers is to unravel the mechanisms underlying HLA heterozygosity’s unique protective effects, moving the research for the first time to preclinical disease models. Additionally, they plan to explore the role of CD4 T cells and HLA class II in cancer biology, potentially opening the door to novel strategies in the mitigation and treatment of cancer.
Featured

Diego Chowell, PhD
Assistant Professor of Artificial Intelligence and Human Health, and Oncological Sciences
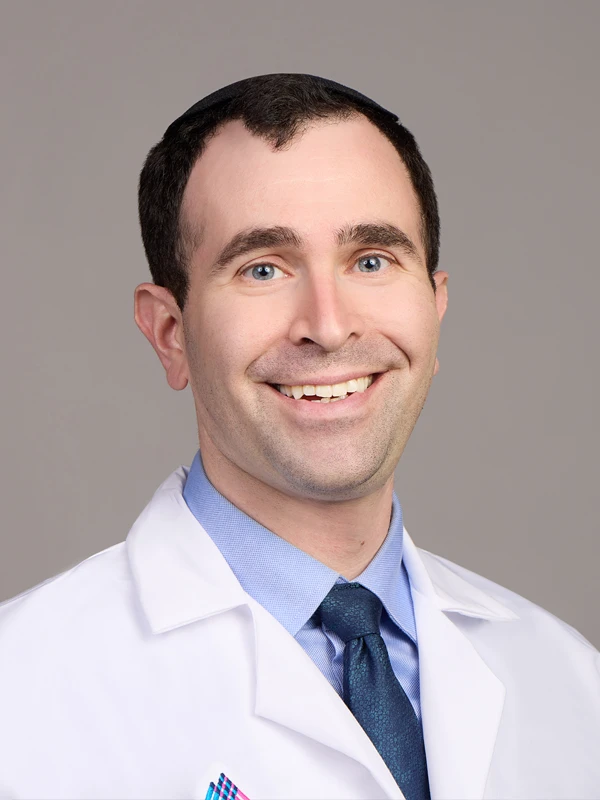
Robert Samstein, MD, PhD
Assistant Professor of Radiation Oncology