New research funded by the National Cancer Institute (NCI) is targeting lethal prostate cancer, exploring the role of BRCA2 and other so-called “DNA damage repair genes” in an effort to create new therapeutic paradigms.
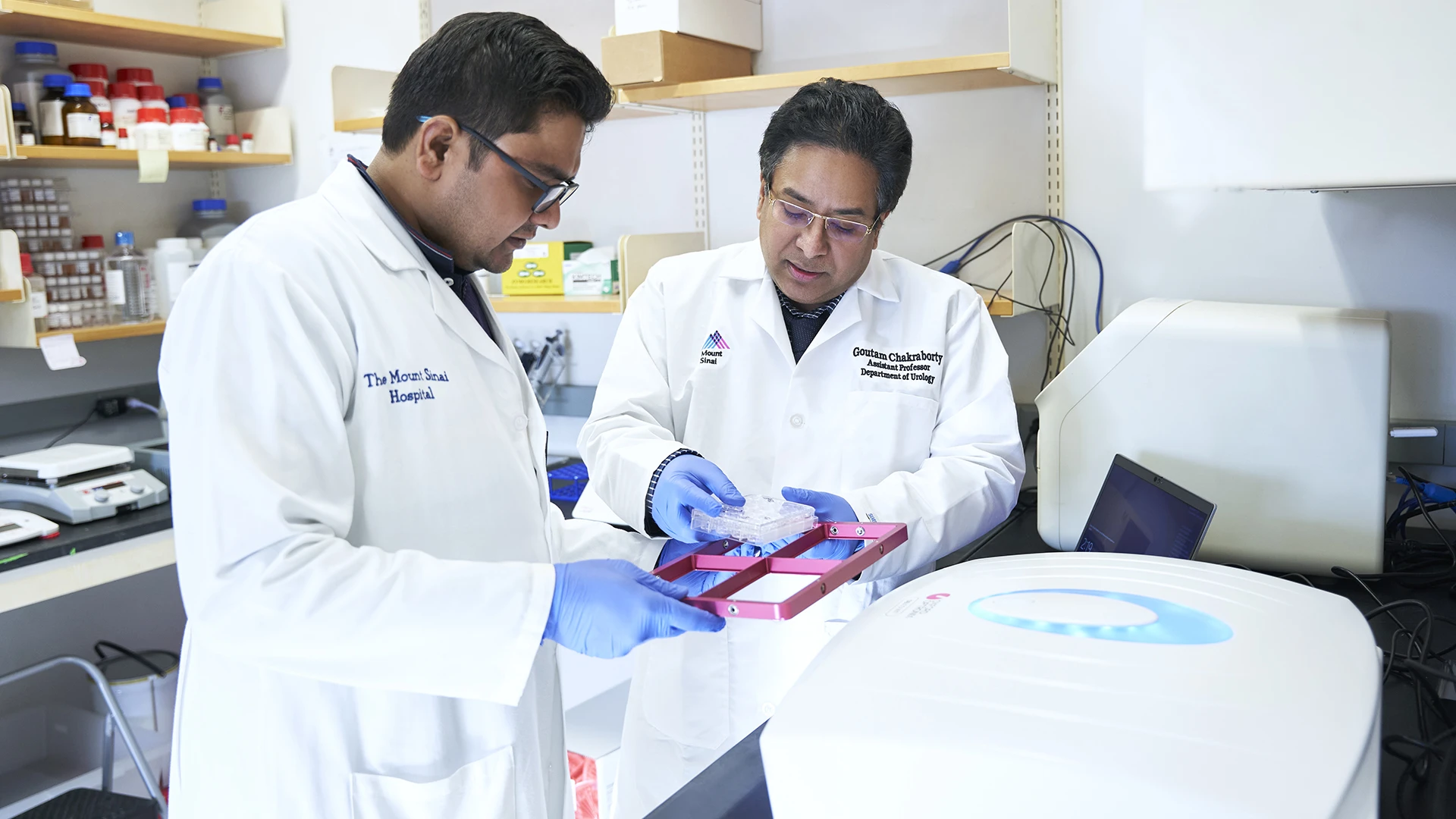
Leading the study is Goutam Chakraborty, PhD, Assistant Professor of Urology, and Oncological Sciences at the Icahn School of Medicine at Mount Sinai and member of the NCI-designated The Tisch Cancer Institute. Dr. Chakraborty launched the study in April 2023 with an R01 grant from the NCI. The funding provides $729,450 in 2023-2024, with an estimated total of $4.3 million over the five-year grant period. His research suggests that mutations in DNA damage repair genes such as BRCA2 may drive the transformation of prostate cancer from a slow-growing, localized tumor to an aggressive, treatment-resistant metastatic disease. By characterizing the molecular mechanisms behind that process, he hopes to develop new treatments to target the deadliest cases of prostate cancer.

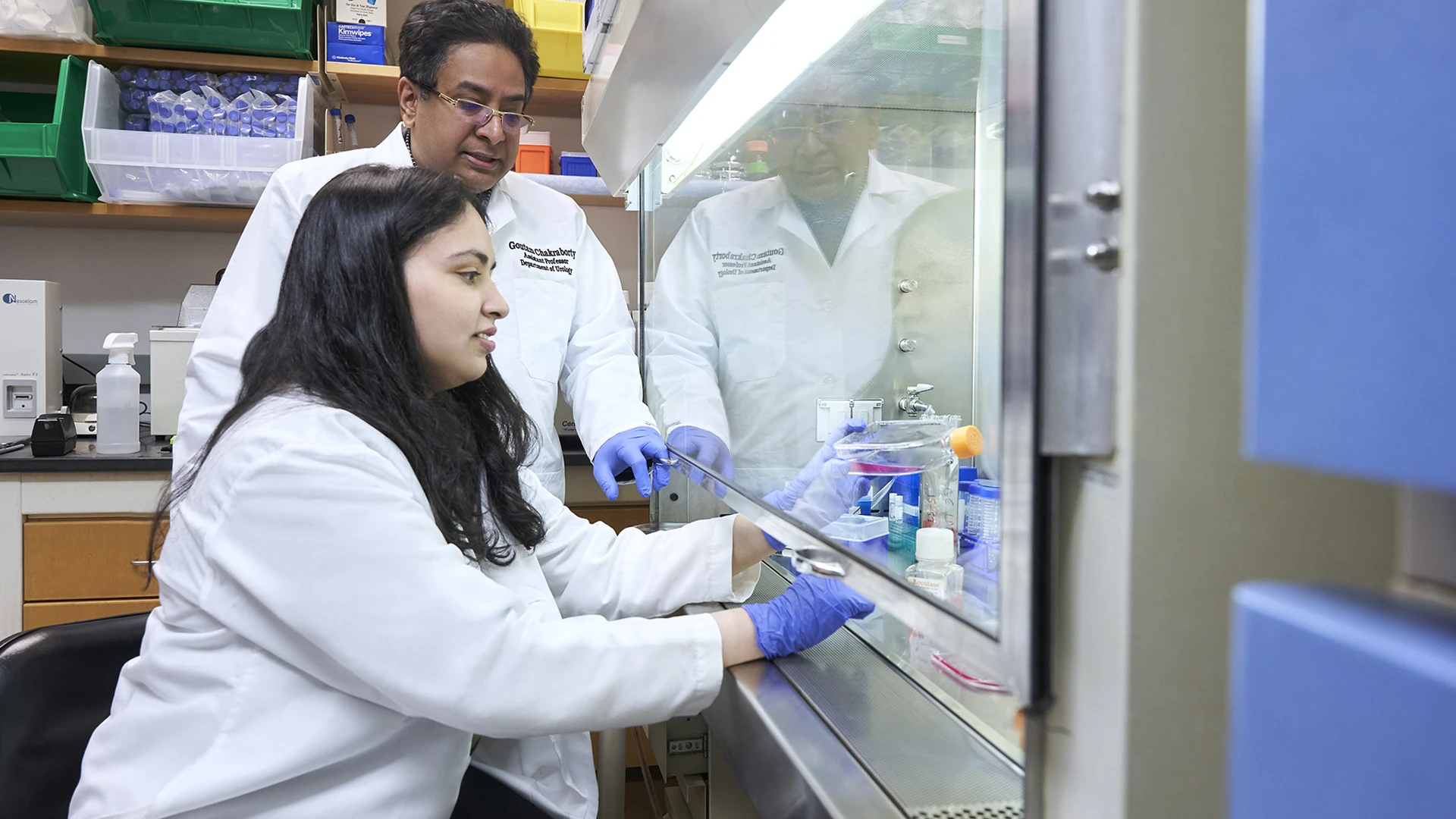
Goutam Chakraborty, PhD (left), works with lab member Prathiksha Prabhakaraalva , PhD (right), to explore how deletions and mutations of genes implicated in DNA damage repair, such as BRCA2, could turn prostate cancer into an aggressive and treatment-resistant disease.
Prostate cancer is the second leading cause of cancer death among men in the United States. Much of that burden is due to metastatic castration-resistant prostate cancer (mCRPC), an advanced form of the disease that is resistant to antiandrogen therapy. The five-year survival rate in men with metastatic disease is just 30 percent. To better understand why some prostate cancer cells become resistant to antiandrogen therapy, Dr. Chakraborty zeroed in on mutations in DNA damage repair genes—in particular, BRCA2.
BRCA2, RB1, and Prostate Cancer
While BRCA2 mutations are common in breast and ovarian cancers, Dr. Chakraborty’s research suggests that deletions of the BRCA2 gene are specifically associated with lethal prostate cancer.
“We analyzed mutational frequencies—including hereditary and somatic mutations and deletions—among people with nonlethal versus lethal prostate cancer. And we found a four- to fivefold increase of BRCA2 mutations in lethal cancers,” he says. “The first part of this study is to understand the molecular biology of why prostate cancer cells that harbor BRCA2 mutations don’t respond to antiandrogen therapy. Then we can develop novel therapies to treat lethal prostate cancer.”
Radiopharmaceutical and Immunotherapy Target for Prostate Cancer
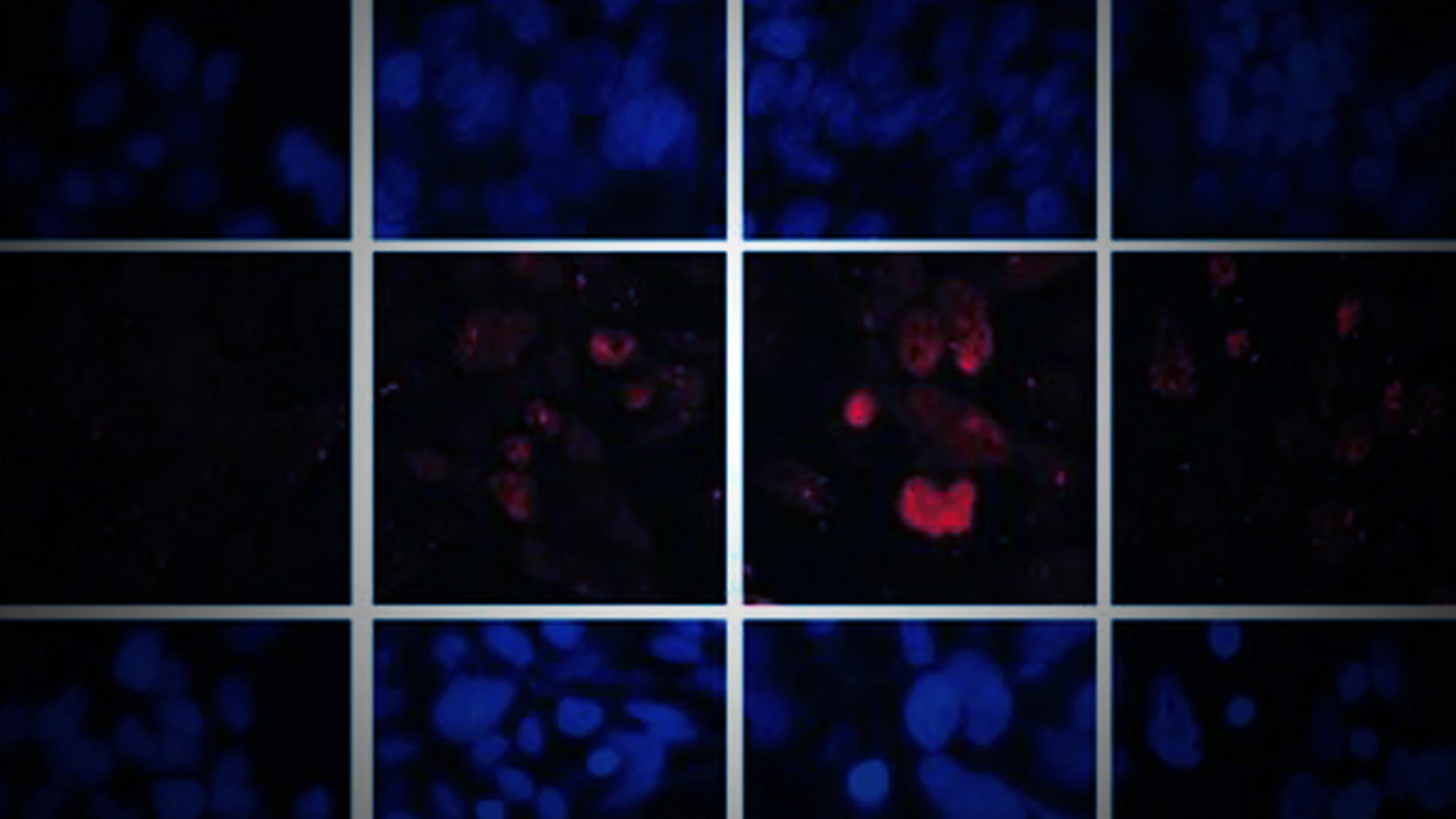
Dr. Chakraborty’s work has led him to investigate prostate-specific membrane antigen (PSMA) as a prime target for radiopharmaceutical therapy, as well as immunotherapy. He has shown that the loss of BRCA2 leads to high levels of PSMA expression. “In general, prostate cancer doesn’t respond well to immune therapy,” he explains. However, since BRCA2-mutant cells have higher genomic instability, they may be more likely than other prostate cancer subtypes to respond to immunotherapies.

Members of Dr. Chakraborty’s lab, from left to right: Goutam Chakraborty, PhD; Nabila Zaman, Sarah Ann S. King, PhD; Prathiksha Prabhakaraalva, PhD; and Atar Singh Kushwah, PhD.
This line of research has spurred collaborations with immunology experts to develop CAR T-cell therapy targeting PSMA. Dr. Chakraborty is also collaborating with radiochemistry experts to target PSMA with radiopharmaceutical therapy. This approach has recently been approved by the U.S. Food and Drug Administration (FDA) for treating patients with PSMA-positive mCRPC. He plans to test those therapies in conjunction with poly (ADP-ribose) polymerase (PARP) inhibitors—another promising drug candidate group he identified in previous work. His 2020 Clinical Cancer Research paper also showed that PARP inhibitors reduced cell growth in prostate cancer cell lines missing copies of BRCA2 and RB1. Using mouse models implanted with tumors from his CRISPR-derived human cell lines, he will study the combination of PARP inhibitors with the newly developed CAR T-cell therapy and PSMA-targeted radiopharmaceutical therapy. “I’m hopeful that combining these therapies will lead to a better response and increase survival of patients. If our preclinical studies are successful, we are prepared to move into clinical trials immediately,” he says.
“We have strong preliminary data. Now we have to connect the dots,” Dr. Chakraborty adds. “Ultimately, I think we have a high potential to translate this research into new classes of treatments.”
Featured

Goutam Chakraborty, PhD
Assistant Professor of Urology, and Oncological Sciences