Women who believe they’ve fully recovered from breast cancer sometimes get devastating news years later: their tumor has resurfaced in distant bone. With the help of a $450,000 grant from the Breast Cancer Research Foundation (BCRF) and the American Association of Cancer Research (AACR), a Mount Sinai scientist is starting to unravel this phenomenon and the potential role of fibroblast growth factor 2 (FGF2), part of a large family of growth factors known to enrich and, at times, dysregulate the bone microenvironment. From this important work could emerge not just a clearer understanding of cancer cell survival, but potential therapeutic strategies to reduce the risk of breast cancer relapses in the bone.

Igor Bado, PhD (right), and his lab members Rahat Alam, BS (left), and Chau Duong, BS (center). Dr. Bado has secured a grant to explore the role of fibroblast growth factor 2 in the bone microenvironment, which has an impact on breast cancer metastasis.
“Determining how breast cancer cells can remain dormant for 20 years or more apart from the primary tumor site in patients thought to be cancer-free is a clinical and research mystery we hope to shed light on,” says Igor Bado, PhD, Assistant Professor of Oncological Sciences at the Icahn School of Medicine at Mount Sinai, and recipient of the three-year BCRF/AACR Next Gen Grant for Transformative Cancer Research. “What we know is that FGF2 plays an important role in cell survival, maintenance, and proliferation and helps create a unique ecosystem that may be favorable to bone metastasis. All these properties make FGF2 an intriguing candidate for further exploration.”
FGF2 belongs to a family of 22 fibroblast growth factors that permeate bone and bind to four receptors that activate signaling pathways involved in such normal functions as tissue regeneration, wound repair, embryonic development, and hematopoiesis. Dysregulation of these pathways, however, may trigger aggressive cancer phenotypes, resistance to chemotherapy, and generally poor clinical outcomes. Indeed, bone is known to be a frequent site of breast cancer relapse, with several studies suggesting that FGF2 may play an important role in promoting a number of solid and hematological tumors. At the same time, the bone microenvironment has been associated with long-term dormancy of cancer cells, especially in patients who develop tumors classified as hormone receptor positive (HR+).

Dr. Bado (right) with lab member Duong (left) at the fume hood, working on cancer cultures. By delving into the basic mechanisms of how cancer cells enter into dormancy, findings can shed light on how these cells later reemerge as metastatic.
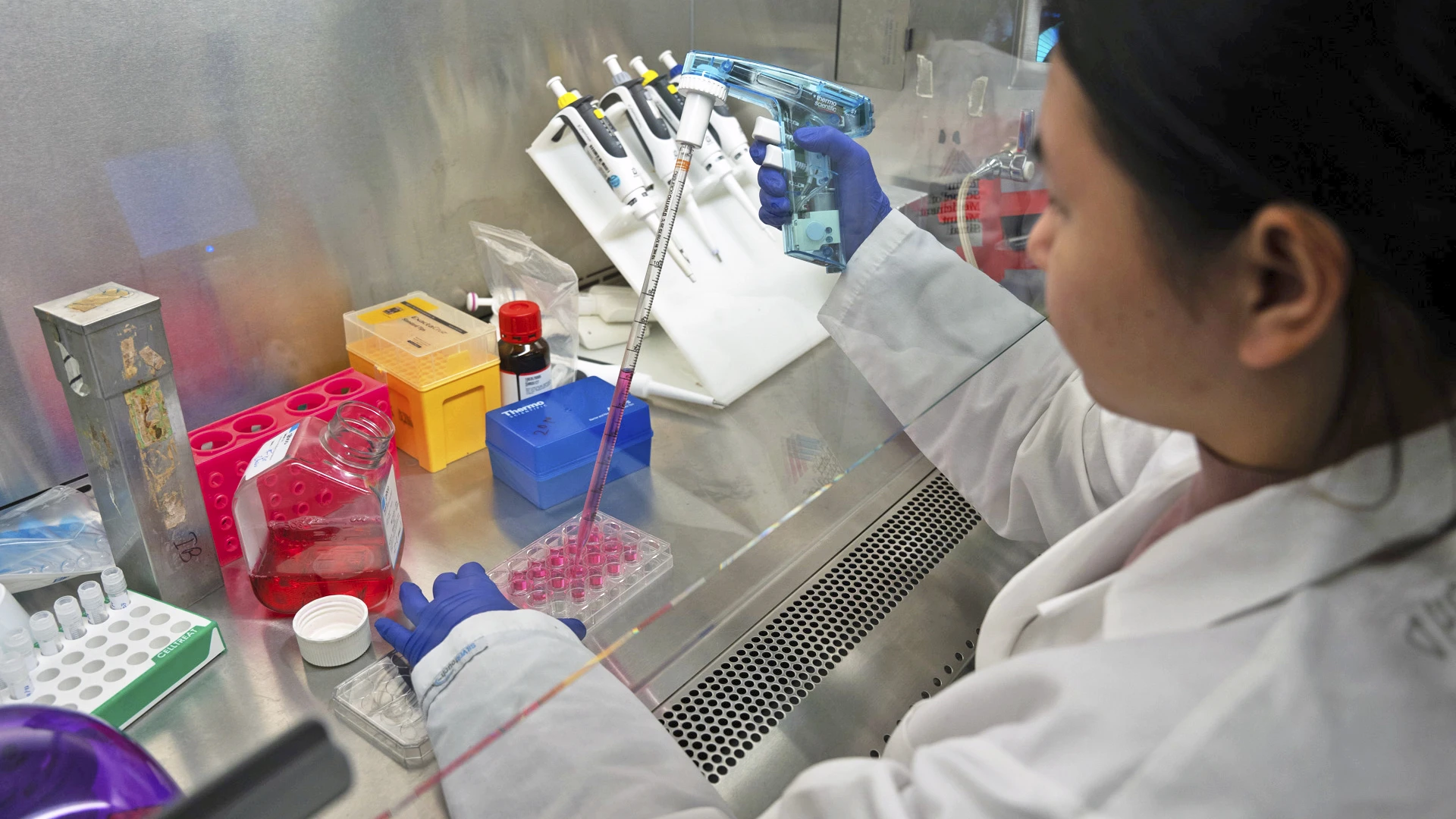
The research on FGF2 that Duong and members of Dr. Bado’s lab are working on has implications not just on breast cancer, but many other solid and hematological tumors as well.
“We plan to investigate through our mouse models whether bone-mediated secretion of FGF2 is essential for the survival of disseminated breast cancer cells in the bone and if it allows them to actually escape cell death,” notes Dr. Bado. “Very little is currently known about how these cells manage to survive for so long, or how they recur in bone three, five, or even 20 years later.”
One theory is that cancer cells that disseminate to bone can undergo a “senescence-like” process in which they remain protected by bone building cells that render them more resistant to treatment, such as chemotherapy and endocrine. Dr. Bado plans to explore in his research how and why FGF2 tends to cluster in proximity of osteoblast-enriched areas of the bone, as high expression of FGF2 is believed to signal impaired outcomes and shorter survival for patients with relapsed and refractory cancers.

Imaging is an important component of Dr. Bado's (right) and lab member Alam's (left) work. At the imaging station, the team scans thousands of samples regarding receptor activity of FGF2, tying links to tissue function.

Dr. Bado (right) and Alam (left) pore through samples at the microscope, working on basic science of tumor senescence, but those findings will have great impact down the road on informing treatment strategies.
An equally intriguing part of Dr. Bado’s unfolding research is its potential pathway to pharmacologic solutions and as a predictive biomarker for bone metastasis that starts as breast cancer. “Once we’re able to biologically link FGF2 to breast cancer cell survival, we can start thinking about inhibiting the signaling between this protein and its receptors,” says Dr. Bado. “Some inhibitors have already shown promise, but the real challenge—and our ultimate goal—is making them specific to FGF2 signaling in cancer cells so we can eliminate the threat of breast cancer recurrence for patients over the longer term.”
Featured

Igor Bado, PhD
Assistant Professor of Oncological Sciences