More than 70 years ago, the immunologists Lewis Thomas, MD, and F. Macfarlane Burnet, MD, PhD, advanced the notion that the immune system constantly surveils the body for cancer cells, killing off foreign invaders before they become clinically detectable. While this theory and the broader one of immunoediting have since been proven in mice, whether they apply to human cancers has been a topic of considerable scientific debate over the years.
An important new chapter is being written by Marta Luksza, PhD, Assistant Professor of Oncological Sciences, and Genetics and Genomic Sciences, at the Icahn School of Medicine at Mount Sinai. She and her research team reported on a study, published in Nature in June 2022, of 70 pancreatic cancer patients over 10 years, which found that spontaneous immunoediting did indeed occur in human cancers, resulting in the immune system detecting immunogenic antigens (neoantigens) in primary tumors. That detection, in turn, induced the antigen to be eliminated in recurrent tumors, and long-term survivors of the disease had more robust immune systems with strong T cell activity in primary tumors compared to the general study population.
“Most intriguing is our finding that well-developed immune systems in the rare survivors of pancreatic cancer had the unique ability to ‘see’ high-quality neoantigens and mark them to be killed,” says lead author Dr. Luksza, whose computer science background informs her research for The Tisch Cancer Institute at the intersection of evolutionary biology and immunology.

The work from the laboratory of Marta Luksza, PhD, is contributing evidence that immunoediting occurs in tumors, which has implications for long-term survival of patients.
Using the dynamic of how the immune system marks neoantigens, Dr. Luksza’s team has created a model that captures the selective pressures by T cells on tumor clones. “We believe this clearer understanding of the mechanisms involved in the evolution of tumors could have tremendous implications for the future design of therapeutics for pancreatic as well as other types of cancer,” she states.

Immunoediting historically had the hallmarks of surveillance and elimination of tumor cells, but over the years it has evolved to include two other phases that involve equilibrium and escape. More specifically, the rare cancer cells that are not destroyed in surveillance and elimination phase enter the equilibrium phase, where they are maintained in a state of immune system-mediated growth dormancy. In the final escape phase, tumors further adapt to evade immune recognition, including hijacking the immune system’s own pathways to escape T cell control and grow unconstrained in the host.
The tumor cell “fitness” model created by the Mount Sinai-led researchers is in sync with the three evolutionary phases of immunoediting. It predicts how immune system pressure prompts cancer cell populations to evolve over time, and the statistical evidence the team has gathered suggests that patients who survive the longest develop genetically less heterogenous recurrent tumors with fewer immunogenic mutations, or neoantigens, Dr. Luksza explains.

Dr. Luksza's findings are being advanced in a variety of translational settings, including a personalized vaccine study.
“As we look ahead, these findings provide a rationale to use neoantigen-based therapies to activate immunity in pancreatic and similarly low-mutated cancers.”
Marta Luksza, PhD
The fitness model is now being evaluated in a therapeutic context of personalized vaccines for pancreatic cancer as part of a clinical trial in collaboration with Memorial Sloan Kettering Cancer Center, BioNTech, and Genentech.
“We believe our model will lead us to the design of an effective vaccine that can optimally stimulate the immune system by targeting the right combination of high-quality neoantigens,” says Dr. Luksza. “And that excites me the most about the work we do: using mathematical approaches to create novel treatments such as personalized vaccines with the potential to make a difference in the lives of people with cancer.”
Featured
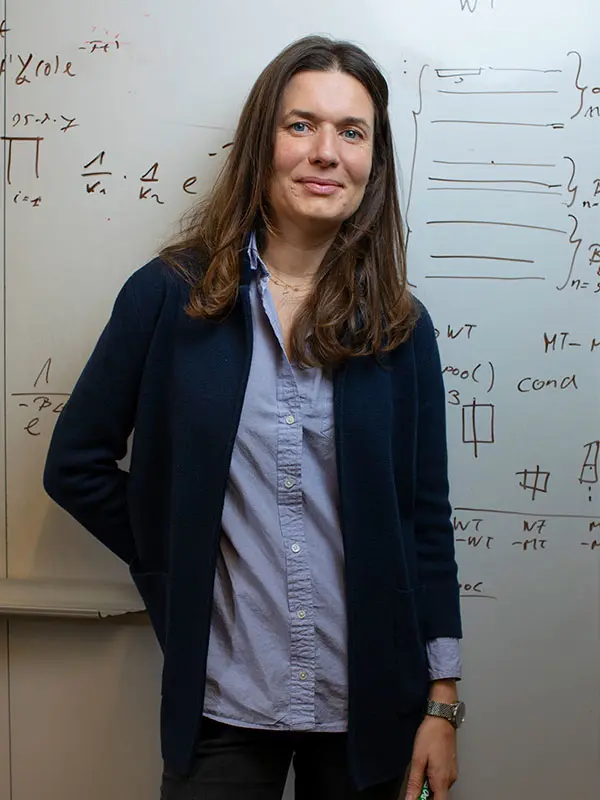
Marta Luksza, PhD
Assistant Professor of Oncological Sciences, and Genetics and Genomic Sciences
