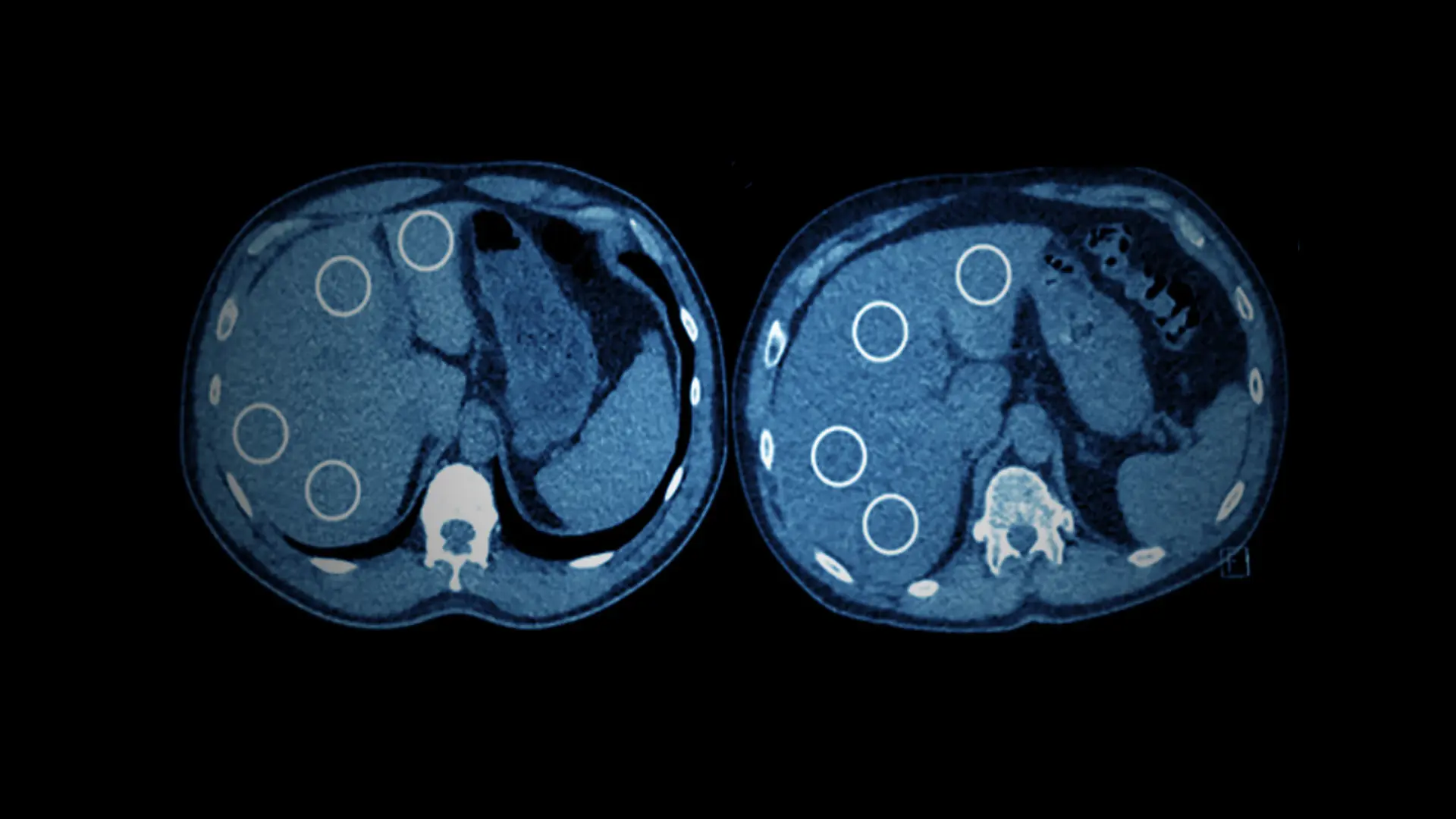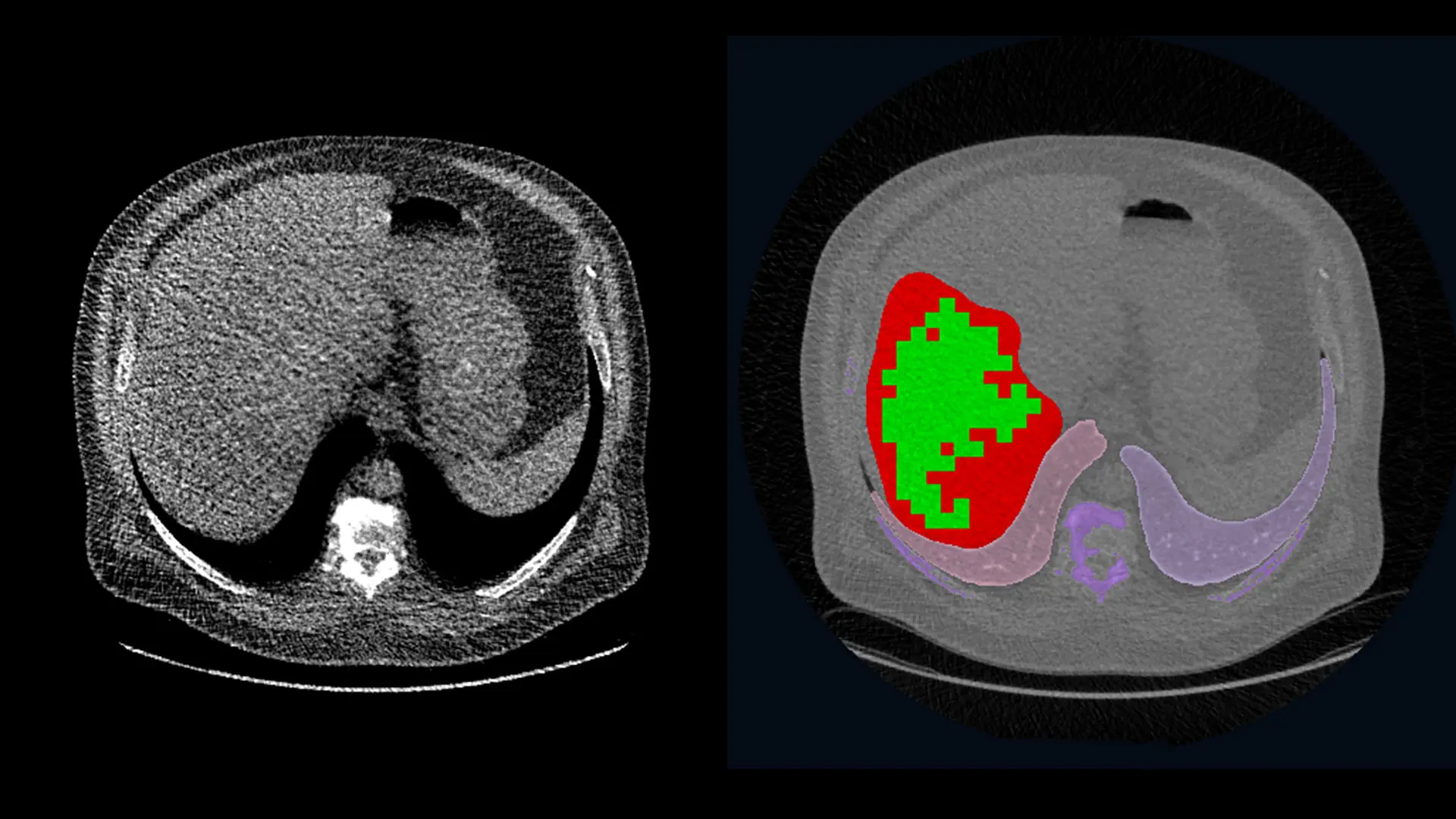
Left: A single slice of the CT scan for a participant in the WTC study with a liver density indicative of moderate-to-severe steatosis. Right: The same CT scan shows the region of the liver to be analyzed in red, the sampled areas in green, and other organs in purple (the lungs and vertebrae).
A known connection between liver disease and exposure to chemical toxins, such as benzene and glass fibers, prompted researchers at the Mount Sinai Health System in 2020 to investigate the incidence of hepatic steatosis—high levels of fat in the liver—in World Trade Center (WTC) first responders. Using low-dose CT (computed tomography) lung screening, the researchers found that the WTC cohort—composed of 154 individuals—was three times more likely to have moderate-to-severe steatosis than those who were not WTC first responders. Their findings, published April 2020, in Clinical Imaging, established this condition in WTC responders for the first time. Steatosis can lead to fatty liver disease, scarring, and liver cancer.
“We were not surprised to find evidence of steatosis in this population given the known association between toxic chemicals and liver disease. But the number of liver issues we observed was much higher than anticipated,” says the study’s senior author, Claudia Henschke, MD, PhD, Clinical Professor of Diagnostic, Molecular and Interventional Radiology, at the Icahn School of Medicine at Mount Sinai.
Dr. Henschke and her team followed up with an epidemiological study, which analyzed 1,788 lung scans that had been performed on WTC first responders between 2001 and 2018, as part of Mount Sinai’s WTC Health Program. The results of this study, published July 2021 in the American Journal of Industrial Medicine, showed that more than 14 percent of the WTC cohort had signs of hepatic steatosis. They also found that responders who arrived at Ground Zero within the first two weeks after the September 11 attacks, were significantly more likely to have steatosis than those who worked in the rescue and recovery efforts afterward.
“Given the prevalence of hepatic steatosis in first responders, we need to have enhanced monitoring for liver disease. From the same single image, we can see indicators of disease in other organs with no additional exposure to radiation.”
Artit Jirapatnakul, PhD
“Given the prevalence of hepatic steatosis in first responders, we need to have enhanced monitoring for liver disease,” says the study’s first author, Artit Jirapatnakul, PhD, Assistant Professor of Diagnostic, Molecular and Interventional Radiology. “From the same single image, we can see indicators of disease in other organs with no additional exposure to radiation and no additional scans.” Dr. Henschke favors recommending low-dose CT scans for hepatic steatosis with referrals to a specialist if there is an indication of liver damage.
Over the last 30 years, Dr. Henschke has been instrumental in the development and approval of national and international guidelines for low-dose CT (LDCT) screening for the early detection of lung cancer in high-risk populations. She has also collaborated with Dr. Jirapatnakul, additional colleagues in radiology, and subspecialists across multiple areas to design and test methods for the early detection of diseases in other organs as a part of routine lung cancer screening.
“LDCT for lung cancer provides images of the entire chest and upper abdomen,” says Dr. Henschke. “This is a low-radiation dose scan that requires only a few seconds to obtain. With our collaborators, we have demonstrated its utility for detecting asymptomatic coronary artery disease, COPD (chronic obstructive pulmonary disease), and thyroid disease, among other conditions. LDCT is essentially an overall ‘health check.’”
Meanwhile, additional research into liver disease is continuing at Mount Sinai under the leadership of Andrea Branch, PhD, Professor in the Division of Liver Diseases, and co-author on the WTC studies. Dr. Branch directs a National Institute for Occupational Safety and Health-funded project that investigates evidence of toxicant-associated liver disease in WTC responders. She is also exploring the relationship between fatty liver disease and fibrosis, the scarring that leads to liver failure, and how toxicity contributes to disease.
Featured

Raja M. Flores, MD
Chair of Thoracic Surgery; Steven and Ann Ames Professor in Thoracic Surgery

Emanuela Taioli, MD, PhD
Professor of Population Health Science and Policy; Director, Institute for Translational Epidemiology; Associate Director for Population Science, The Tisch Cancer Institute

Claudia Henschke, PhD, MD
Clinical Professor of Diagnostic, Molecular, and Interventional Radiology