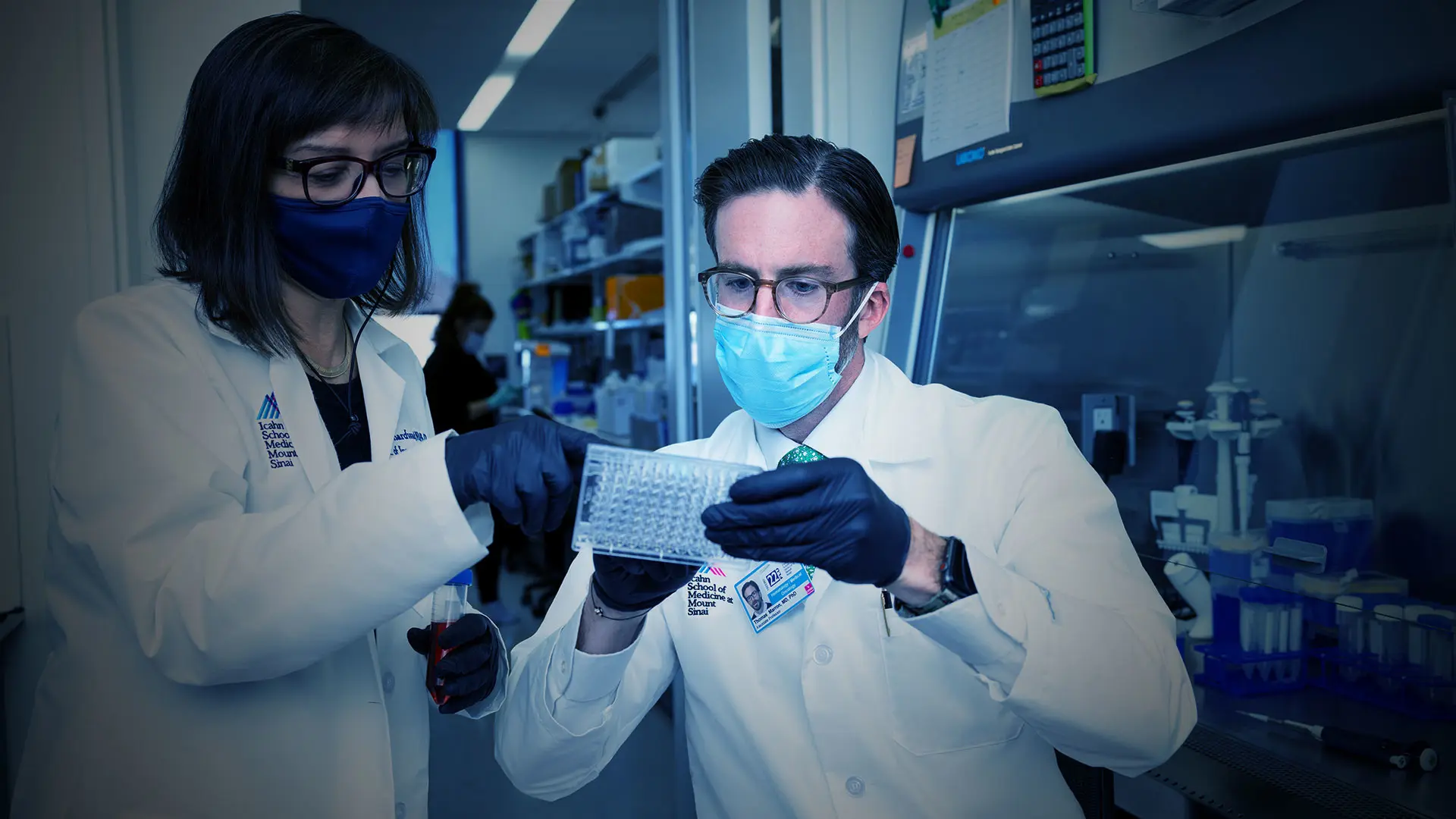
Nina Bhardwaj, MD, PhD, and Thomas Marron, MD, PhD
Tumors accumulate DNA mutations at a high rate, and some of these mutations result in the translation of mutated proteins, termed neoantigens. These novel and patient-specific proteins can be immunogenic and represent promising targets for the development of personalized cancer vaccines.
At the Annual Meeting of the American Association for Cancer Research in April 2021, researchers led by Nina Bhardwaj, MD, PhD—Ward-Coleman Chair in Cancer Research and Director of Immunotherapy at The Tisch Cancer Institute (TCI)—reported promising results in a unique and personalized vaccine trial. They showed that a personalized genomic vaccine—specific to the neoantigens created in individual patients—was, in fact, safe and potentially beneficial.
Mount Sinai’s trial was the first to test a personalized vaccine in multiple types of cancer in the adjuvant setting. The patients were at high risk for disease recurrence following curative-intent therapy—either surgery for solid tumors or stem-cell transplant for multiple myeloma.
The vaccines were developed at Mount Sinai’s Vaccine and Cell Therapy Laboratory using TCI’s proprietary computational platform, OpenVax. The tumor’s DNA and RNA and the patient’s germline DNA were sequenced to identify mutations unique to the tumor. OpenVax identified at least 10 neoantigens likely to initiate an immune response in 13 of the 15 patients in the trial. Patients
were each administered seven-to-ten doses of a personalized vaccine, along with the immuno-stimulant poly-ICLC to boost the immune response.
“We have demonstrated that OpenVax is a feasible platform for the development of a safe personalized vaccine, and we are gaining a deep understanding of response. This will inform new approaches to vaccines, as well as to other immunotherapies.”
- Thomas Marron, MD, PhD
The patients were followed for a median of 925 days, and the study’s primary outcome was achieved: The vaccine proved to be safe and well tolerated. Four patients—nearly one-third of study participants—had no recurrence of disease, including patients with lung, breast or bladder cancers, and multiple myeloma.
While the study has far-reaching implications, “super-personalized” vaccines such as these are not necessarily practical for large-scale use due to the expensive and time-consuming nature of their development.
“We have demonstrated that OpenVax is a feasible platform for the development of a safe personalized vaccine, and we are gaining a deep understanding of response,” says Thomas Marron, MD, PhD, Associate Professor of Medicine (Hematology and Medical Oncology) and Director of TCI’s Early Phase Trials Unit. “What we have learned will inform new approaches to vaccines, as well as to other immunotherapies.”
The Mount Sinai team recently launched one of the new approaches—a shared neoantigen vaccine that will be administered to patients with common cancer cell mutations. By identifying cancers in which tumors develop the same mutations across many patients, the vaccine peptides can be developed in bulk rather than patient-by-patient.
The phase I trial of a shared neoantigen vaccine is set to begin.
Dr. Bhardwaj and her collaborators have found a number of such conditions with “shared neoantigens” across multiple patients, including a group of blood disorders known as myeloproliferative neoplasms in which cancer cells in approximately one-third of patients have a mutation in the CALR (calreticulin) gene. No curative treatments currently exist for MPN patients, making it imperative to identify new therapies.
When the researchers determined that the neoantigen peptide was effective in a small subset of patients they also discovered that many patients had high levels of checkpoint receptors, which had, essentially, shut off any T-cell response. Combining the peptide with checkpoint inhibitors (anti PD-1 and CTLRA-4) restored T cells in vitro and elicited a dramatic response in
vivo.
The research team recently initiated a phase I trial to test the safety of the shared neoantigen vaccine in MPN patients and will begin enrolling patients soon. In subsequent studies, they expect to combine the vaccine with checkpoint therapies to ensure a robust and durable response. “With this approach we can reach the patients who will have the greatest likelihood of responding,” says Dr. Bhardwaj.