Patient survival of some of the most aggressive forms of uveal melanoma—the most common primary intraocular malignant tumor—can be particularly dismal and lead to death in less than six months. Anne Bowcock, PhD, Professor of Oncological Sciences, Genetics and Genomic Sciences, and Dermatology, Icahn School of Medicine at Mount Sinai, has made significant strides in understanding the progression of the disease and developing effective new therapeutic targets.
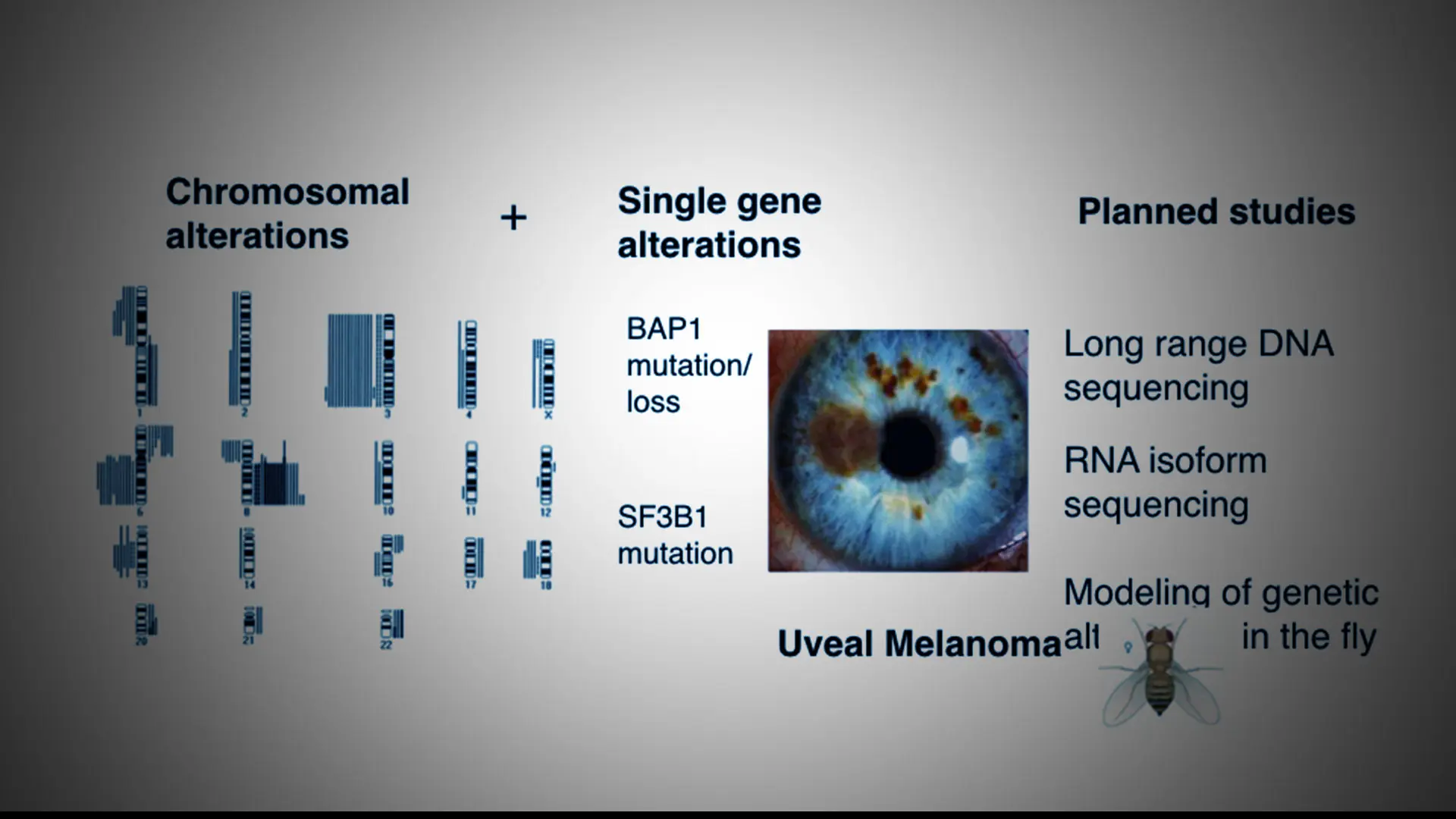
A leading investigator of the genomics and chromosomal alterations that play a role in uveal melanoma pathogenesis, Dr. Bowcock and her team eight years ago were the first to identify two genes—BAP1 and SF3B1—that together, are mutated in the majority of uveal melanomas that metastasize. The discovery of BAP1, a protein that acts as a tumor suppressor, led to the development of a diagnostic marker that is widely used today for determining treatment and
prognosis of uveal melanoma.
Dr. Bowcock continues to model mutations through a variety of novel systems, including the fruit fly, which shares many common genes with humans. On this, she collaborates with co-investigator Cathie Pfleger, PhD, Associate Professor of Oncological Sciences at Icahn School of Medicine at Mount Sinai. In a 2019 study, Dr. Bowcock described new candidate genes involved in tumorigenesis, including a potential tumor suppressor role for PHF10/BAF45a.
With renewed funding from the National Institutes of Health, Dr. Bowcock is exploring chromosomal changes in uveal melanoma using long-read sequencing. The technology can generate sequences of DNA molecules up to hundreds of kilobases in length. This allows her to examine the large-scale rearrangements that arise in tumors, which have been poorly understood, until now.
“Chromosomes are inherently unstable, either losing or gaining pieces of DNA, which correspond to characteristic changes we see in uveal melanoma,” Dr. Bowcock explains. “Understanding these changes will give us a better window on genetic alterations in uveal melanoma and their downstream consequences. This will hopefully lead to new long-term treatments for uveal melanoma.”
The development of uveal melanoma is accompanied by large-scale chromosomal changes and smaller mutations, including single base-pair changes in genetic drivers such as BAP1 and SF3B1. Long-range sequencing, modeled in the fruit fly, will permit an in-depth analysis of the DNA alterations that occur.
Featured

Anne Bowcock, PhD
Professor of Oncological Sciences, Genetics and Genomic Sciences, and Dermatology