Clinical neuropsychologist Kristen Dams-O'Connor, PhD, Director of the Brain Injury Research Center at the Icahn School of Medicine at Mount Sinai, and her team study a grim phenomenon that has been virtually unexamined despite its vast prevalence: brain damage suffered by individuals with a history of intimate partner violence (IPV).
An estimated one-third of all women worldwide experience physical and/or sexual IPV during their lifetimes. Of those, the majority suffer multiple traumatic brain injuries (TBI). Yet, until now, while there are papers on the clinical sequelae of IPV, there are none on the neuropathology of IPV other than a couple of case reports, says Dr. Dams-O’Connor.
“There is so little research in this space, it’s mind-blowing. How is it possible that in this day and age, after the billions of dollars devoted to brain health research, that we know so little about the medical and neurological consequences of intimate partner violence? This is what happens when there are topics that are buried in secrecy and shame and that are hard to study,” says Dr. Dams-O’Connor, Professor of Rehabilitation Medicine and Neurology at Icahn Mount Sinai.

Despite the prevalence of traumatic brain injury in intimate partner violence (IPV) cases, there is a lack of published research on its neuropathology. Kristen Dams-O'Connor, PhD is working with the New York City’s Office of the Chief Medical Examiner to shed light on the neuropathology of people who have a history of IPV.
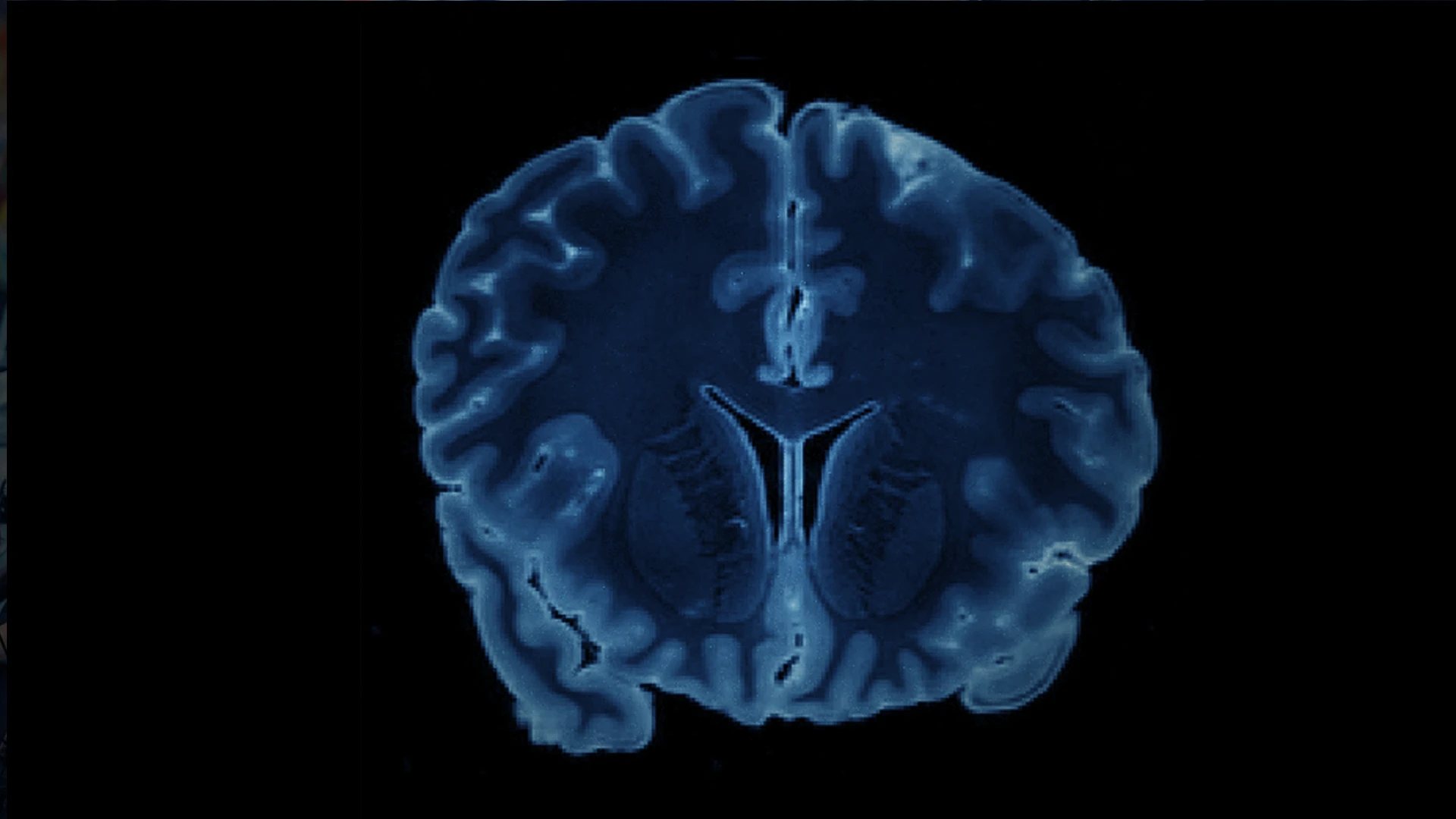
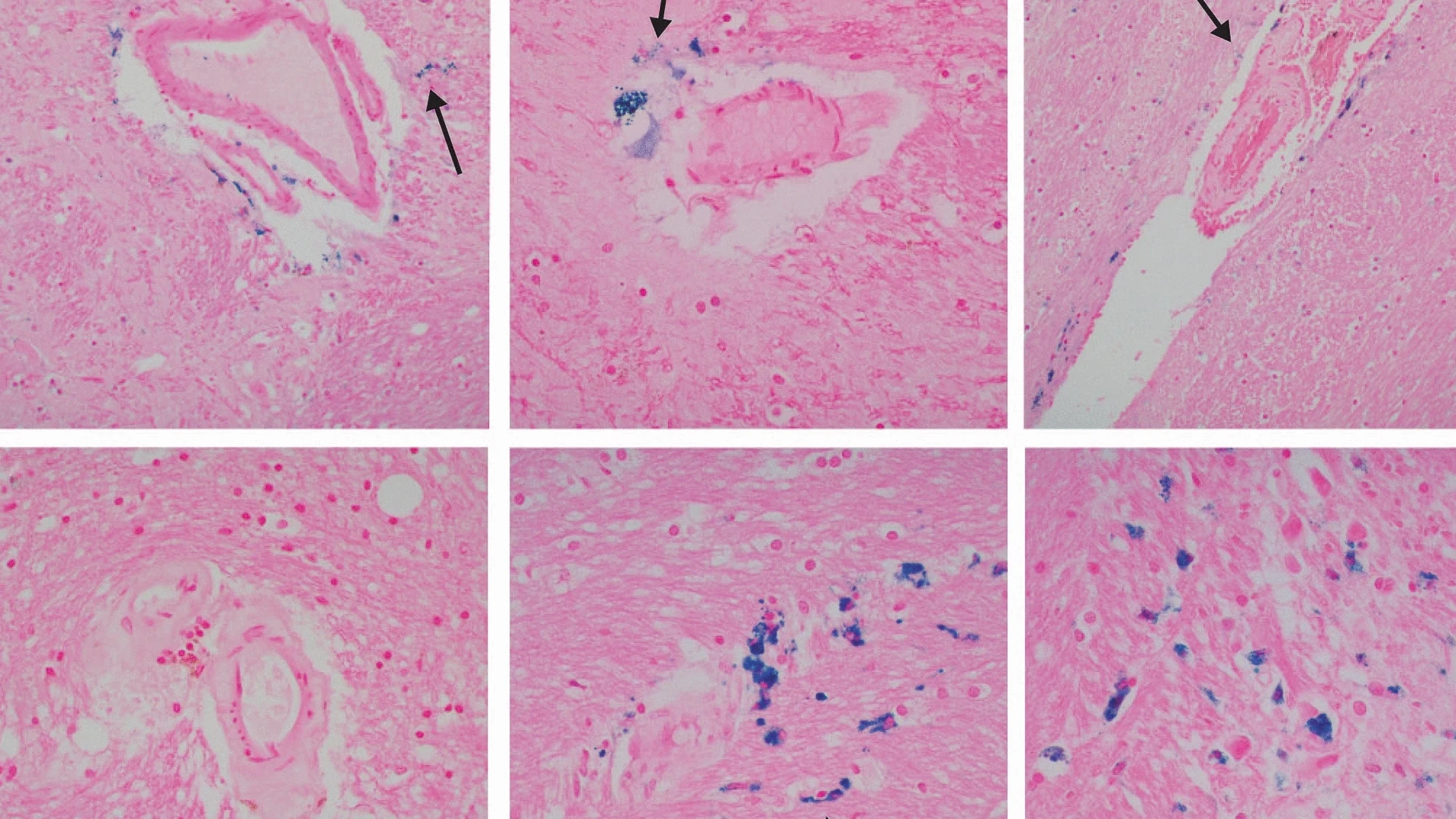
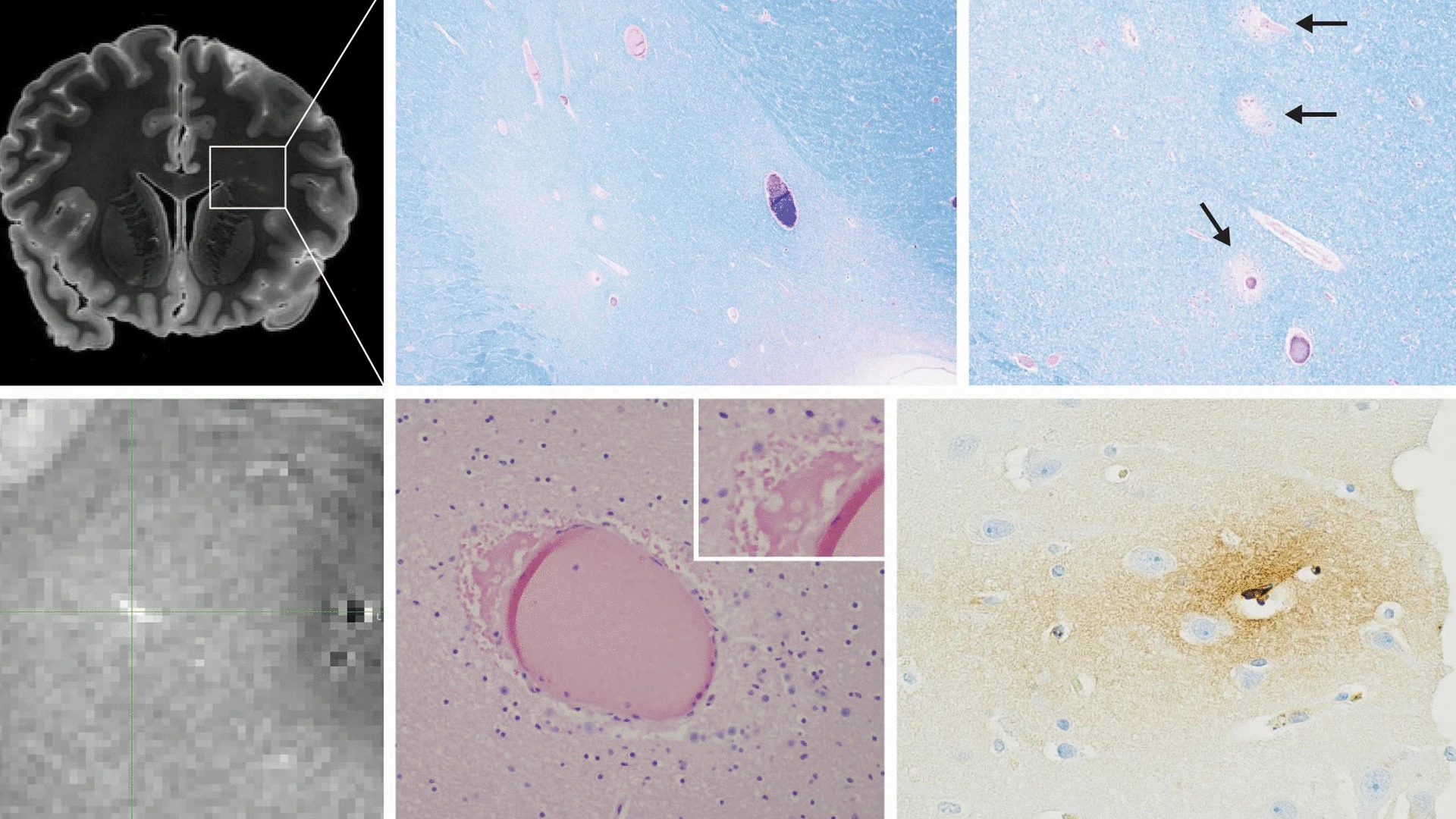
Her team is studying it, using state-of-the-art brain imaging and pathology techniques in the brains of decedents who had experienced IPV, in collaboration with New York City’s Office of the Chief Medical Examiner and scientists from other centers in the U.S., Canada, and the U.K.. In a new paper published in Acta Neuropathologica in October 2023, they report results from a total of 84 women decedents who had documented IPV during their lifetimes.
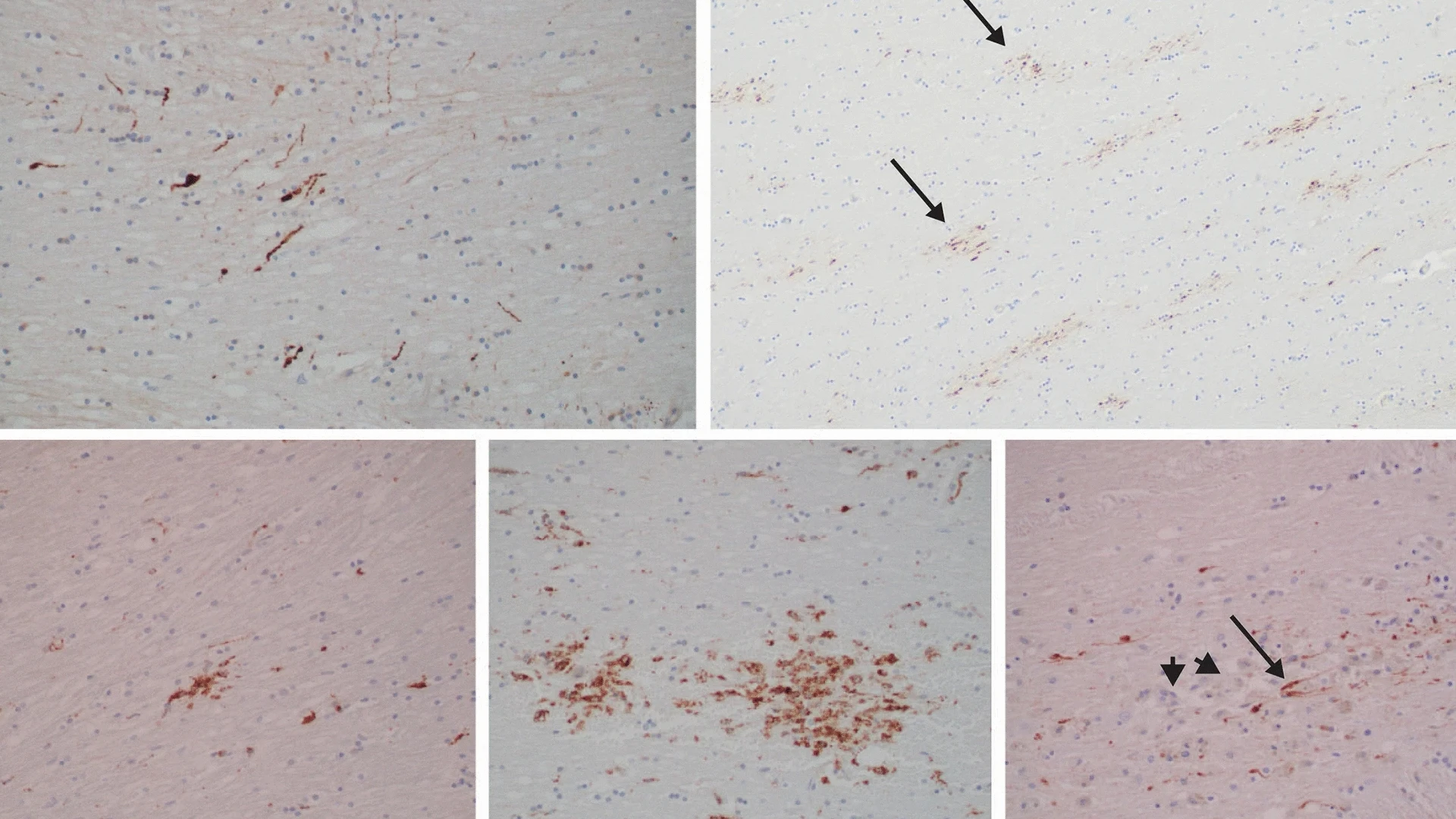
All the decedents had signs of TBI, often with newer injuries layered over old. Many had substantial white matter and vascular pathology. Findings suggested both mechanical injury and hypoxic-ischemic—caused by a lack of blood flow and oxygen—injury that can arise from nonfatal strangulation (NFS). There were also higher-than-expected rates of substance abuse, psychiatric conditions, and HIV infection, along with epilepsy, diabetes, and cardiovascular disease.
One-third
of women worldwide have experienced intimate partner violence in their lifetimes
“The burden of comorbid medical conditions is astounding in this series, especially given that this is a relatively young group of women,” Dr. Dams-O’Connor says.
Some of the decedents may have chronic conditions preceding the abuse—although causation could not be established from autopsy data—given that people living with disabilities more likely tend to be victimized by violence. Regardless, it’s clear these women are living with an enormous burden of comorbid disease, she says.
The study results were also noteworthy for another finding: none of the cases met criteria for chronic traumatic encephalopathy neuropathic change (CTE-NC), the widely described condition linked to repeated head injury in male former contact sports athletes.
The long-held belief that IPV is the “female equivalent of football” arose partly from two autopsy case reports in the literature. One, published in 1990, describes a “punch-drunk wife” with dementia. The other, from 2021, was a young woman with CTE who was both an IPV victim and a contact sports athlete.
Given the lack of further research, people have assumed that CTE must happen in IPV survivors, says Dr. Dams-O’Connor. “But in fact, the patterns of injury differ considerably—they can include isolated TBI, repetitive head impacts, and nonfatal strangulation/suffocation injuries,” she adds.
Moreover, she points out, as awareness has been raised about TBI in contact sports such as football, injured athletes are removed from play and medically supervised. “Obviously, that’s totally absent in the context of IPV. These women may not even have the option to receive care. There’s no medically supervised break from a violent relationship.”
The Mount Sinai research is ongoing. Carrie Esopenko, PhD, Associate Professor of Rehabilitation Medicine and Human Performance, is currently leading a study funded by the National Institute of Neurological Disorders and Stroke examining the psychological, cognitive, and neural signatures of IPV-related head trauma in women.
Dr. Esopenko also leads the Enhancing NeuroImaging Genetics through Meta-Analysis (ENIGMA) Consortium Intimate Partner Violence Working Group, a global collaboration examining the effects of IPV-related brain injury. Meanwhile, Dr. Dams-O’Connor is continuing the partnership with the medical examiner’s office, and another planned study will follow a prospective cohort of living IPV survivors, as part of the Late Effects of TBI (LETBI) brain donor program.
“We know so little about this population that we need to study them while they’re living and follow them longitudinally. We want to understand biomarkers that link clinical symptoms and underlying pathobiology. That’s how we can get toward in vivo diagnostics,” Dr. Dams-O’Connor says.
The research offers hope. “If we can identify vascular contributors to cognitive impairment and functional decline, some of them might be treatable. The entire goal is to be able to treat this during life.”
Featured

Kristen Dams-O'Connor, PhD
Director of the Brain Injury Research Center