Traumatic brain injury (TBI) research has entered a “golden age” over the past two decades, as more attention is paid to brain concussions sustained by football players and severe head injuries by military personnel in combat. However, there remains a pressing problem for the field: TBI lacks a validated consensus definition that can be easily used by epidemiological researchers, says neuroepidemiologist Raj Kumar, PhD, MPH, Assistant Professor of Rehabilitation and Human Performance at the Icahn School of Medicine at Mount Sinai.
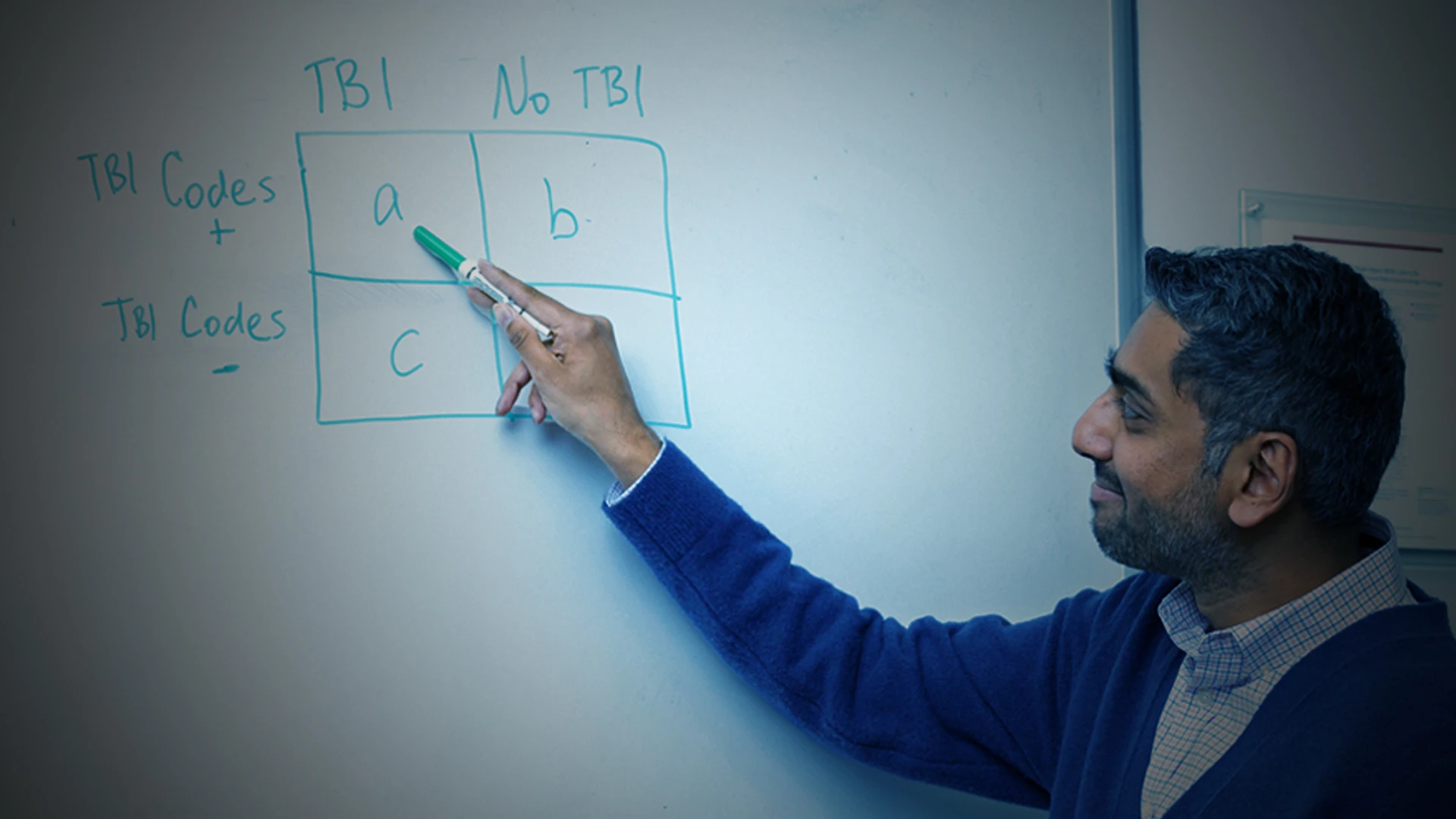
One solution is to use International Statistical Classification of Diseases and Related Health Problems (ICD) codes, used by hospitals for billing purposes. These codes may be used by epidemiologic researchers retrospectively to define cases that appear to fit under the medical rubric of traumatic brain injury. However, with more than 68,000 unique ICD codes, selection of ones that seem most germane to researchers’ cases becomes a rather subjective and imprecise science that may include some individuals who don’t clinically have TBI, while excluding others who do.

Traumatic brain injury (TBI) lacks consistency in its case definition, which makes comparisons between studies hard, says Raj Kumar, PhD, MPH, Assistant Professor of Rehabilitation and Human Performance at the Icahn School of Medicine at Mount Sinai. His study is validating hospital administrative TBI codes to fill that gap.
Dr. Kumar is addressing this conundrum, and has received a combined K99/R00 grant of more than $1 million over five years from the National Center for Medical Rehabilitation Research (NCMRR) as part of National Institutes of Health’s (NIH) Eunice Kennedy Shriver National Institute of Child Health and Human Development to validate administrative case definitions for TBI exposure, severity, and mechanism of injury as an optimal methodology for case identification. Critical to the $747,000 R00 portion of the grant now underway is using electronic medical records residing in the massive Mount Sinai Data Warehouse that aggregates clinical data across the Health System in New York City.
The goal is to first do a scoping review to identify each unique definition of TBI that’s appeared in literature over the past 10 years, explains Dr. Kumar, a faculty member of the Brain Injury Research Center of Mount Sinai. His team will then validate the different case definitions against a secondary source—the electronic medical record data from the Data Warehouse to see how the definitions compare. This same validation process has been done in other neurological diseases, such as epilepsy. An external validation will then occur using the Traumatic Brain Injury Model Systems (TBIMS) National Database, a prospective TBI cohort study involving data collected at 21 acute rehabilitation centers over the past 25 years.
“My job is to present empirical data on sensitivity, specificity, and related statistics for ICD-based case definitions of TBI that exist in the literature,” says Dr. Kumar. Validated TBI case definitions would allow researchers to use the plethora of big health care data that’s out there in a consistent manner, and could even open the door to investigating novel questions using data from studies not specifically designed to study TBI, but contain other phenotypic data of great interest, he adds.

Dr. Kumar (second from left) with his research team, from left to right, clinical research coordinator Sydney McCage; program manager Amanda Watsula; and project manager Brittany Engelman. They are leveraging the Mount Sinai Data Warehouse that aggregates clinical data across the Health System.
The lack of validated TBI case codes has impeded scientific progress in addressing some of the most important issues in the field of TBI today when interpreting meta-analyses, such as establishing the link between TBI and dementia, or TBI and depression and cognitive impairment, says Dr. Kumar. “Empirical data on case definition validity is critically needed to move our field forward, toward greater rigor and reproducibility as we seek to answer the most basic study design question of all: how do you define a TBI?” The question seems obvious, but is often an overlooked detail, and there is currently a complete lack of consensus in the literature for such an administrative definition, unlike other neurological and psychological diseases such as multiple sclerosis, epilepsy, and depression, he adds.
As an example, he cites a recent meta-analysis that evaluated literature over a 30-year span to focus on a highly topical research question regarding TBI and the link to dementia. The review encompassed 10 administrative studies that defined TBI using ICD codes. “The combination of ICD codes was remarkably inconsistent across the 10 studies as evidenced by the six different case definitions that emerged,” notes Dr. Kumar. “We are not looking at an apples-to-apples definition of TBI when we compare results between these types of studies. This inconsistency of TBI exposure definitions suggests they are not well-defined exposures, thus lacking the required level of rigor to infer causality.”

Validation of TBI using Dr. Kumar's method would benefit not just his own research, but other ongoing TBI research at other institutions.
The current study Dr. Kumar has initiated will also benefit other efforts to study TBI, including the National Study of Caregiving (NSOC) and the National Health and Aging Trends Study (NHATS)—ideally suited to address high-priority questions around TBI outcomes and care utilization. “Since there’s currently no data in NHATS or NSOC on TBI exposure, my current study is needed to conduct future work using these types of data sources in a thorough manner,” he acknowledges. “By establishing an empirically validated TBI definition, I’ll hopefully advance the science for not just myself, but for many others in the field whose studies will benefit from enhanced rigor and reproducibility.”
Featured

Raj Kumar, PhD, MPH
Assistant Professor of Rehabilitation and Human Performance