To better understand how Mount Sinai teams can better serve their patient populations, the Office of Patient Experience relies on vital data from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). This data is derived from patient responses to surveys measuring their experience with the Mount Sinai Health System. The Patient Experience scores can help providers understand the barriers faced by both patients and staff and develop solutions to resolve those barriers. In early 2021, health care systems across the nation saw units with traditionally high patient experience scores demonstrate a decline that lasted for several months. The staff attributed this decline to several barriers such as not having enough time with their patients, unfamiliar floating staff adjusting to the unit culture, and unexpected high admission rates.
Mount Sinai Morningside’s surgical unit, 8 East, was not immune to this decline and sought to return to its high ranking within the hospital and Health System. Arthur A. Gianelli, FACHE, President of Mount Sinai Morningside, assembled an interdisciplinary team consisting of clinicians, hospital leaders, and LEAN experts to address the issues the hospital units were facing. This resulted in Patient Survey score improvement after only a few months. This group continues to meet to adjust the approach as needed and to celebrate the work that the unit has accomplished.
8 East, a 39-bed medical/surgical unit, is a large driver of Press Ganey patient survey responses at Mount Sinai Morningside. Recovering from wave 2 of COVID-19 was a challenge for the unit, as identified in their Quarter 1 Hospital Rating scores. A combination of strong leadership, continuous improvement initiatives, and patient experience coaching returned the unit to its pre-COVID-19 hospital rating. Currently, the performance of 8 East is in the top 10 percent, both within the Health System and in the nation.
The strategy that led to this comeback for 8 East was headed by Art Gianelli and Maxine Legall, MBA, MSW, CPXP, Director of Patient Experience and Cultural Transformation.
The first step in stabilizing the unit was focusing on staffing and eliminating the practice of floating staff from 8 East to other units to maximize staff ratios and consistent care delivery. A sheet was created to track measures such as staffing to patient census, nurse floating, and PCA floating. With an emphasis on weekly ratios, staff satisfaction quickly improved.
With a focus on key behaviors to improve Care Checks and Responsiveness, 8 East Nurse Manager Susan Ignacio, RN, partnered with Patient Experience Coach Mindy Morris. Through this partnership, Mindy was able to gain insights and work with Susan to facilitate listening sessions for staff, coordinate Care-Checks role playing, and observe staff interactions with patients during rounding sessions. These observations led to further narration-of-care development and allowed Mindy’s coaching to address issues in real time.
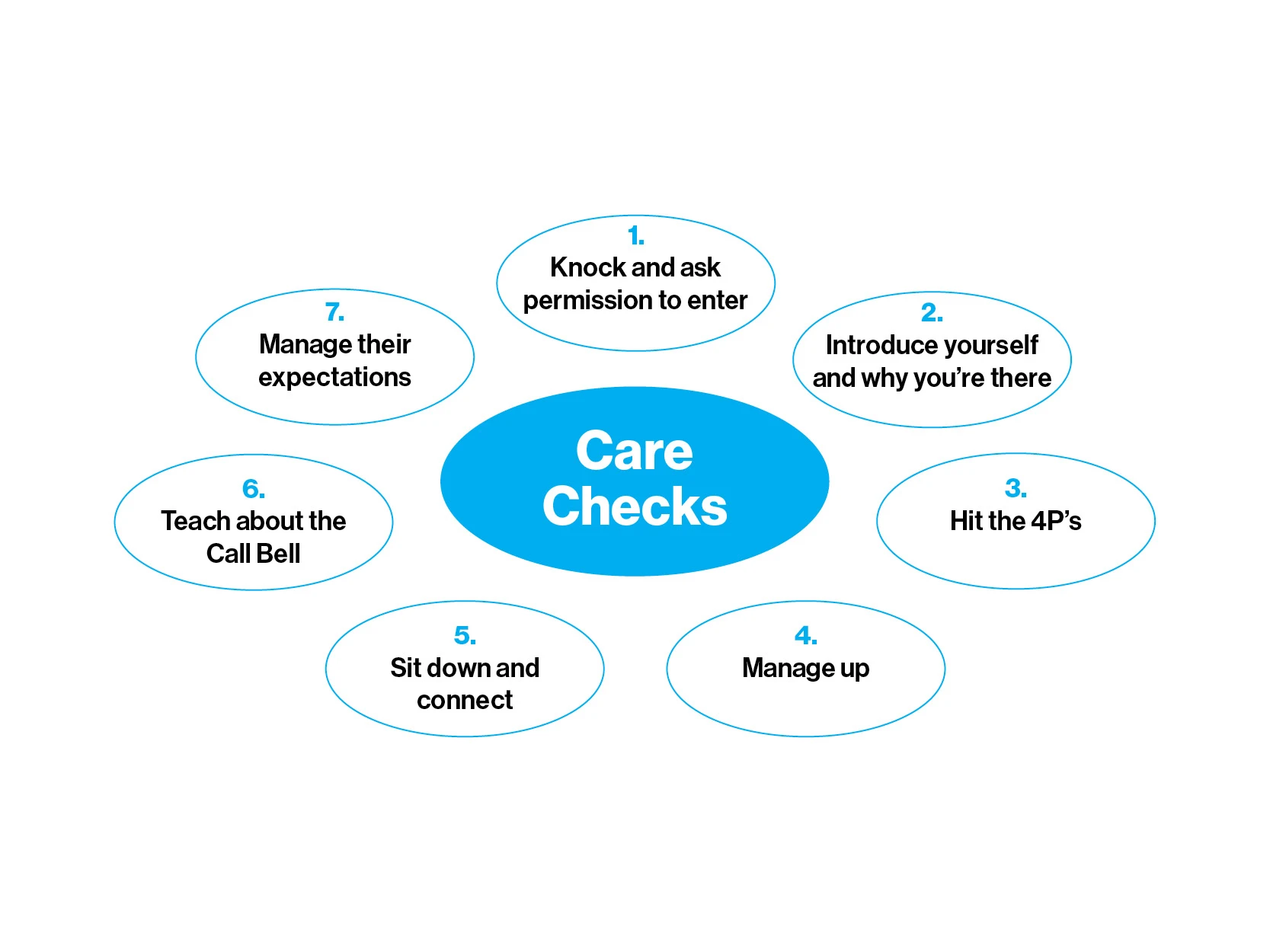
A “Narration of Care” Tip Sheet included Care Checks best practices for the bedside.
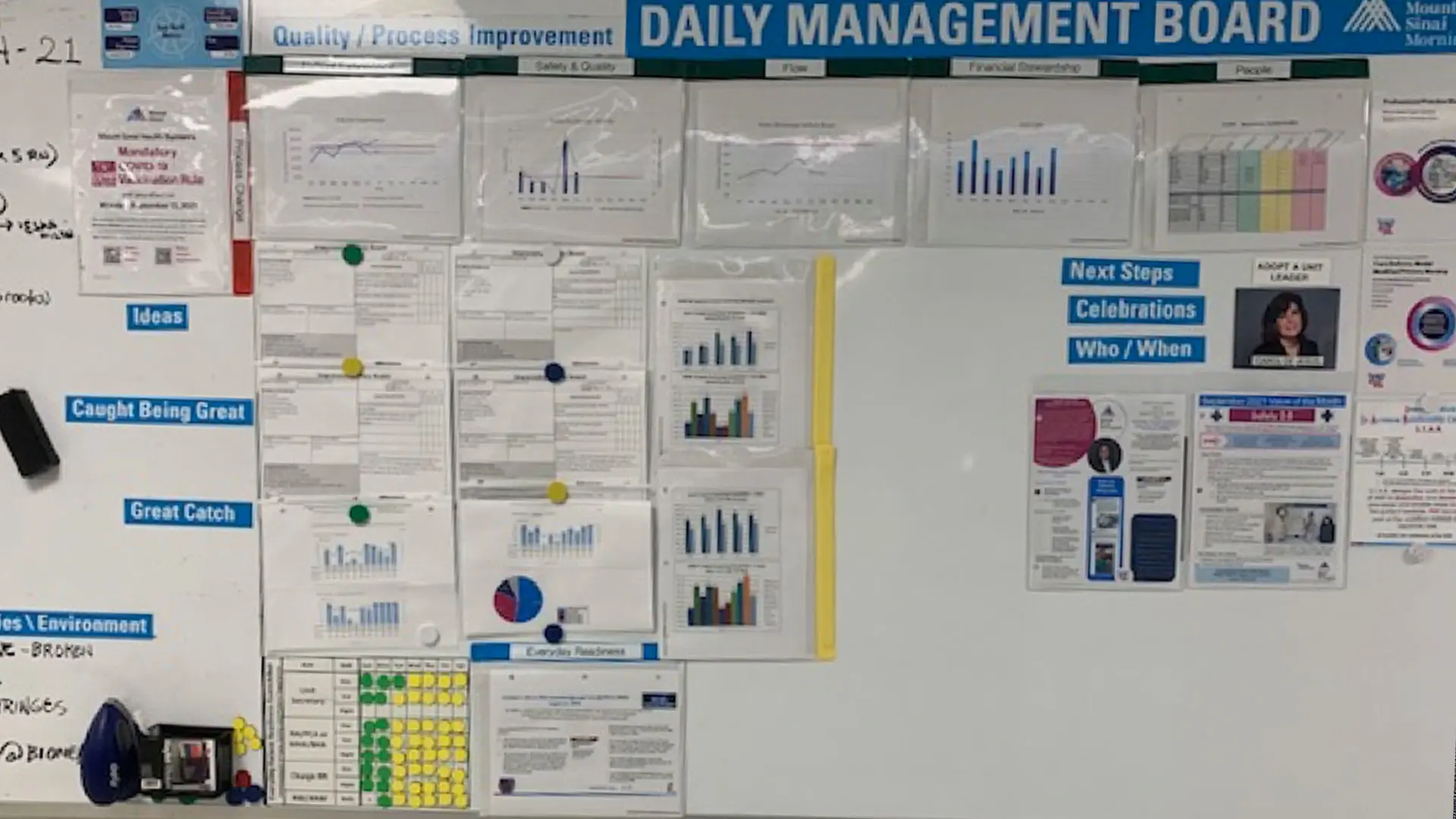
A Patient Experience Storyboard gathered key metrics and employee celebrations to track and enhance performance on 8 East.
A “Narration of Care” Tip Sheet was used during these observations as a resource for all staff. Additionally, weekly patient experience meetings led by Maxine were conducted to review unit performance, discuss interventions, identify blind spots, and prepare for biweekly meetings with the larger group.
To further monitor and drive success, key components of Continuous Improvement were implemented. The 8 East Daily Management Board was used to track interventions and improvements. Additionally, Patient Experience Storyboards were used to identify key process metrics to enhance performance. Susan met weekly with her LEAN coach, Shelcy Kamrud, to review progress.
To address the decrease in responsiveness, 8 East eliminated floating staff from the unit, staffed nursing based on patient census, and increased the call bell volume to level 7 as per the manufacturer guidelines. Nurses also completed Care Checks logs and were supported by Mindy during rounds. The impact of these changes can be seen in the graphs below.
This improvement work would not have been successful without the support of the dyad formed by Nurse Manager Susan Ignacio and Physician Lead John Harvey, MD. Bringing together all members of this team—including nursing, physicians, Continuous Improvement and Patient Experience coaches, Environmental Services, and the site Patient Experience team—garnered success for this unit. “The journey of 8 East proves, yet again, that we are all the patient experience,” Art Gianelli says.
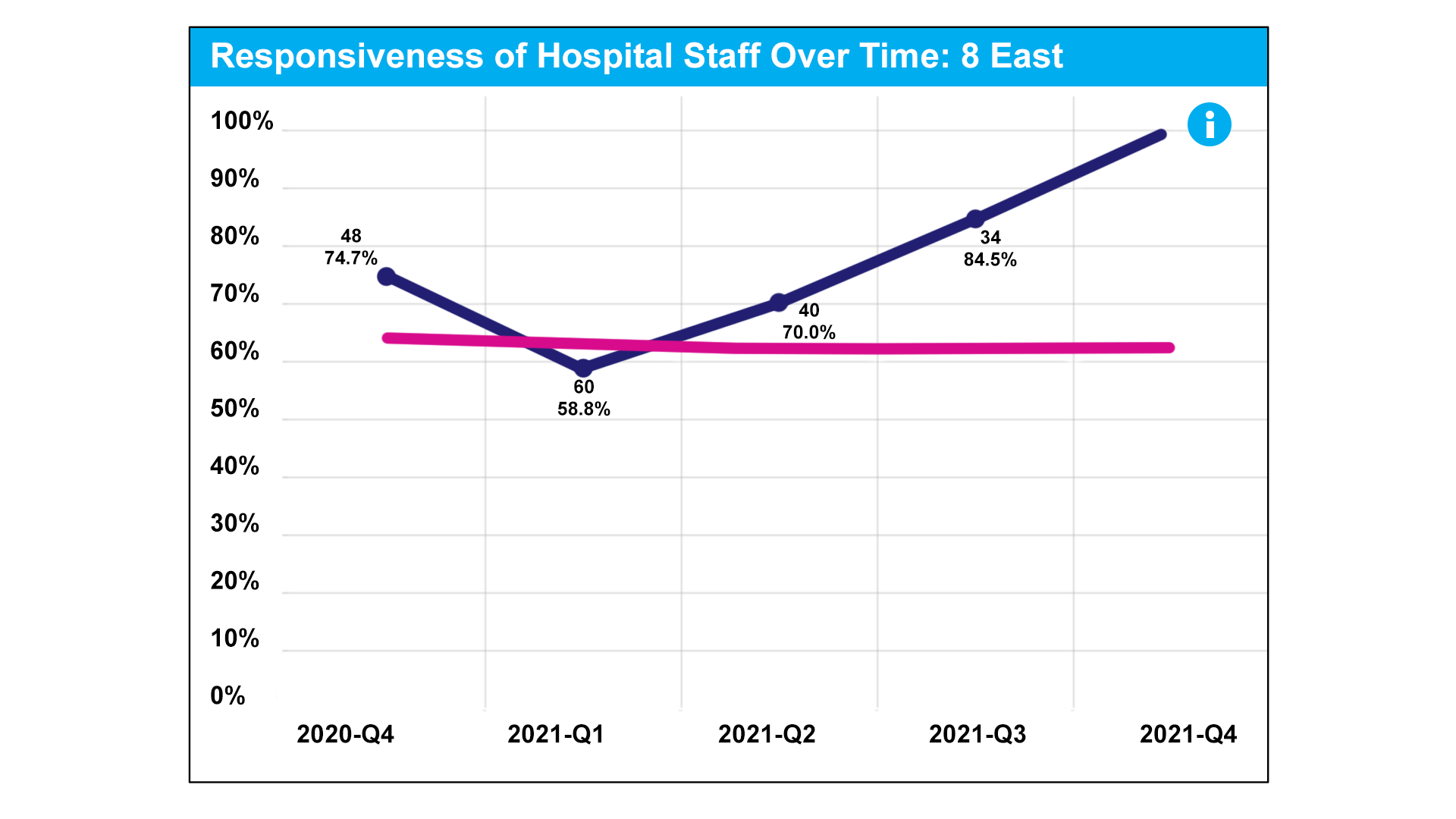
The rating for responsiveness rose significantly by the fourth quarter of 2021.
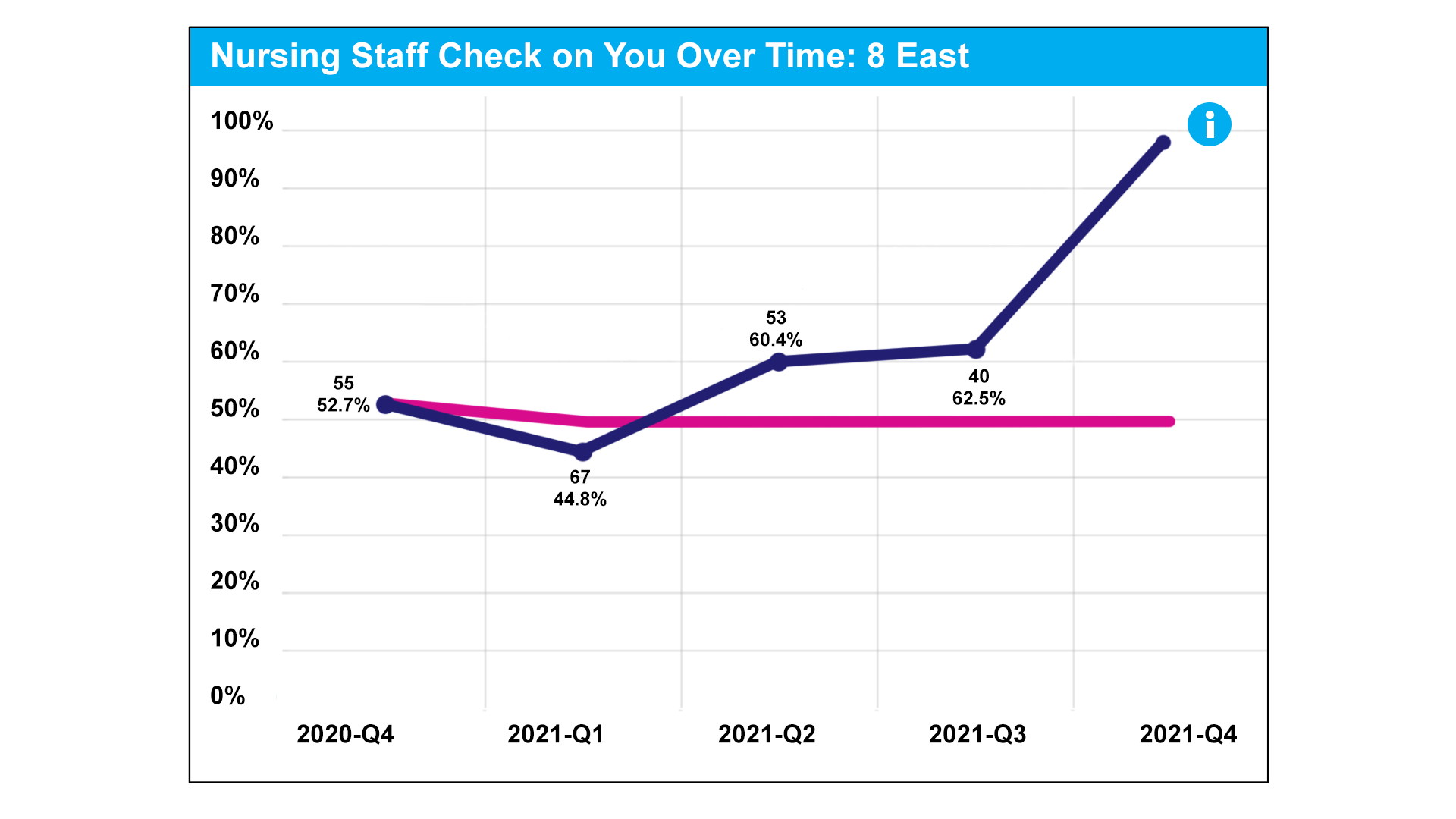
"Nursing staff check on you," a crucial measure of excellence, returned to a high level.
