The year 2020 posed more challenges than any could have ever anticipated. While cities shut down, neighborhoods turned inward, and the world seemed to come to a stop, the Mount Sinai Health System revved up to meet the needs of the community. To combat the spread of COVID-19, the Health System developed a wide range of practices and policies to keep staff and patients safe. However, these interventions—such as limiting visitors and staff visits to patient rooms—created barriers to compassionate care and a positive patient experience.
Human connection and interaction, especially with family and care team, significantly affect the patient’s recovery, and the absence of those interactions can be a detriment to the patient’s health. The staff at each site created practices to combat those barriers.
“Even in the face of COVID-19 and all that came with it, the staff kept compassionate care as a focal point,” says Vicki LoPachin, MD, MBA, Senior Vice President and Chief Medical Officer, Mount Sinai Health System. “Through this very difficult and trying time, the staff have shown that we truly are better together.”
Here are some of the creative and compassionate steps taken at sites throughout the Health System:
The Mount Sinai Hospital

Mount Sinai West
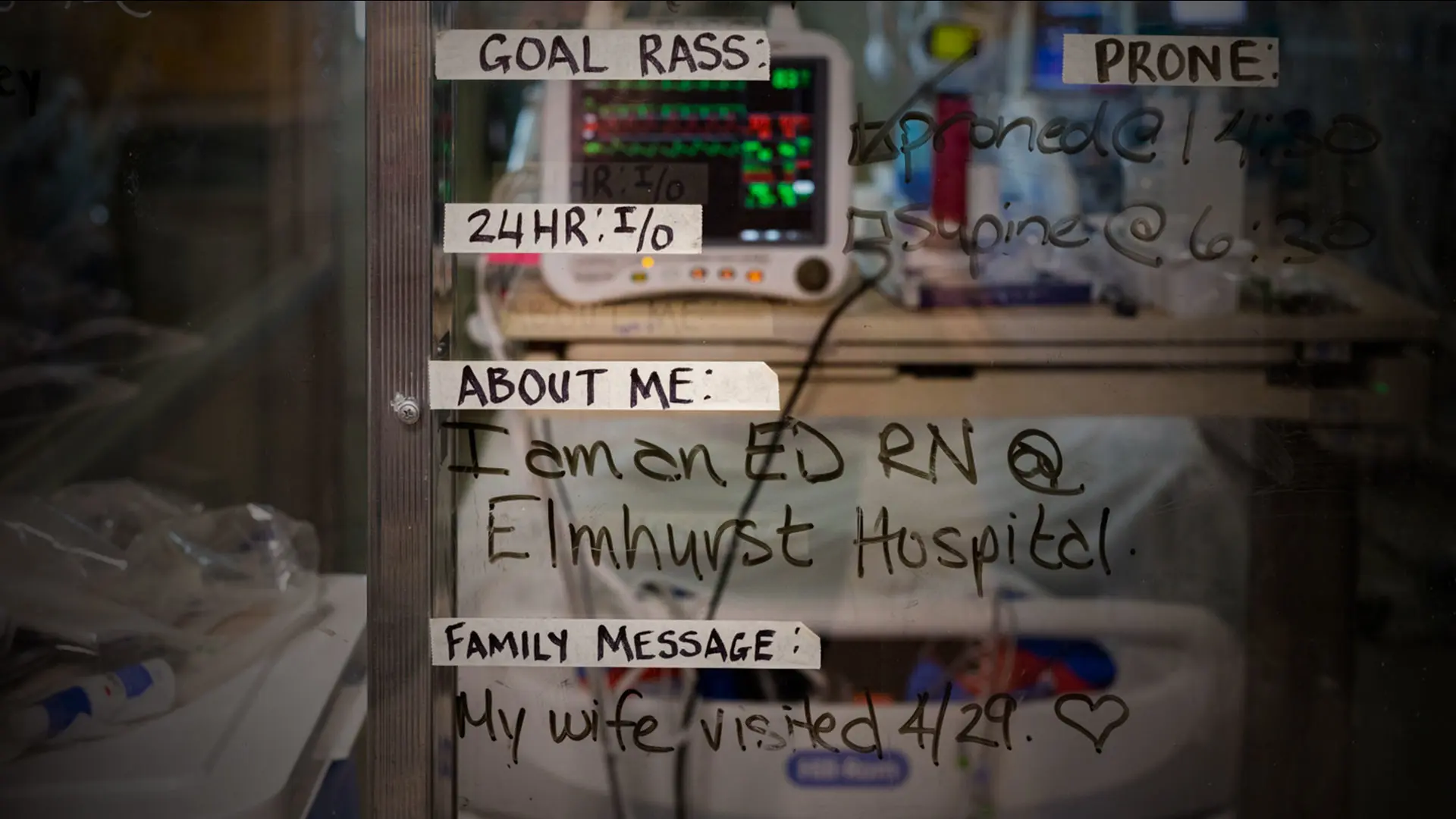
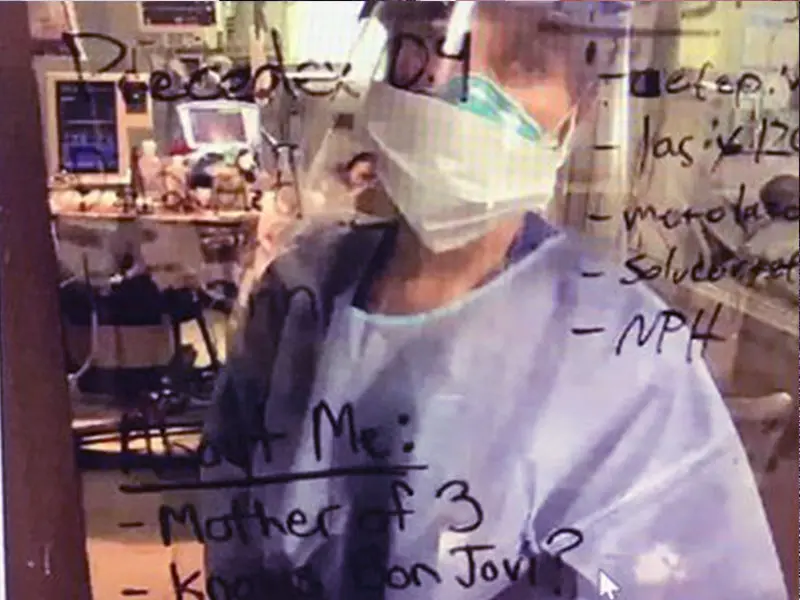
At The Mount Sinai Hospital, as at all sites, the social distancing that kept staff and patients safe made it harder to give compassionate care. Facing this barrier, staff decided to use the new glass walls on the patient rooms to write messages about the patient in the room. This simple act showed the patient that the staff caring for them were not only seeing a number, or a patient with COVID-19, but a mother of two kids who loves her job. Bringing the act of seeing the patient for the person they are, and not their diagnosis, to a whole new level. — Emily Jweid, MBA, CPXP, Administrative Manager
At Mount Sinai West, the limits on visitors that protected patients and their families also meant that some patients neared the end of their lives while separated from their loved ones—and many were afraid and lonely. In a compassionate response, a multidisciplinary group of physician assistants, physical therapists and occupational therapists became End of Life Champions. Members of the team would enter the patient’s room, hold their hand, play the patient’s favorite music, say a prayer and connect family members using Zoom for their last moments, and most important—stayed with them so they weren’t alone. — Andres Moreira, Senior Director, Patient Experience and Patient Relations

A Recharge Room
Across the Health System, safe spaces to retreat to became necessary during the pandemic, and so, with the generous help of the Joseph F. Cullman Institute, Recharge Rooms were assembled. The spaces, which offered sound, scent, visuals, and snacks, were dedicated to supporting the physical and mental well-being of front-line workers. They were created in partnership with Studio Elsewhere, a New York-based design studio specializing in resilient health care environments, and the Abilities Research Center, a part of the Department of Rehabilitation and Human Performance at the Icahn School of Medicine at Mount Sinai.

Mount Sinai Beth Israel

Mount Sinai Health Network
At Mount Sinai Beth Israel, staff used monitors in patients’ rooms for both conversation and observation. Many rooms did not have windows, and patients were in isolation, making it even more vital for nurses to talk to patients while charting and make connections with them. During the PPE shortage, the resident team noticed the emotional toll it was taking on nurses to not see their patients more regularly, and they stepped up to provide baby monitors to nurses so that they could still connect with their patients. — Nicole Porto, Associate Director, Patient Experience and Engagement
Within the Mount Sinai Health Network, many patients were afraid to come in and see their doctors, which could have been detrimental to their health. So the staff organized several practices to help the patients visiting their physicians feel comfortable and safe. Patient greeters stood at entrances, using a white board to communicate wait times to patients, and medical assistants were in the lobby to answer questions. The staff not only welcomed the patients back the office, but remained in communication with them for their entire visit. This enabled patients to see their physicians and, more importantly, made them feel safe to return. — Rebecca Asmussen, Project Manager II
Mount Sinai Queens
Mount Sinai Brooklyn
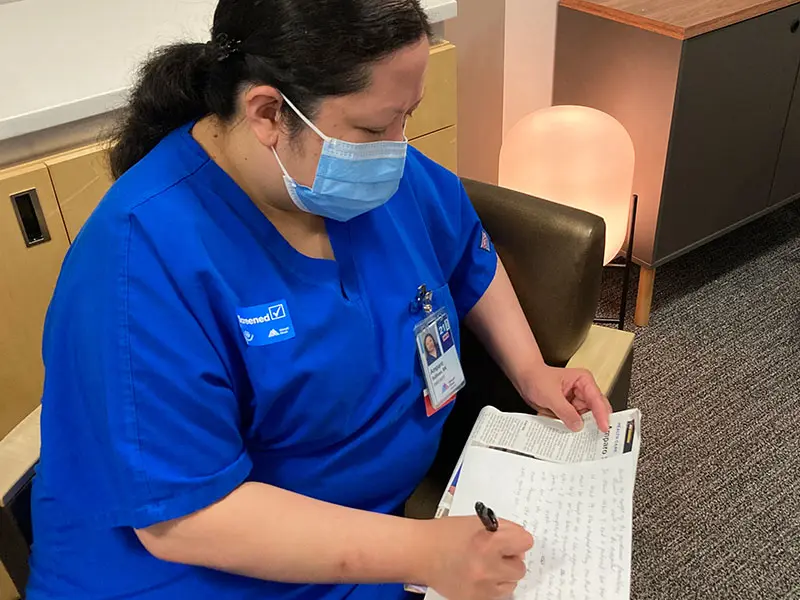
At Mount Sinai Queens, nurses have been writing letters to the loved ones of patients who passed away, in a program that arose from their determination to console the families and their own need to remember the patients they worked so hard to save. “Our nurses were caring for people as they died, and I was praying for people as they died, and no family was present. And it’s heartbreaking,” says the Rev. Dr. Rachelle Zazzu, MA, DDS, Staff Chaplain for Mount Sinai Queens. “So we have been writing letters to the families, fundamentally saying, ‘Your mother was not just patient No. 1234. We cared for her, and we saw beauty in her, and we want you to know that when she died, she was taken care of with a lot of care.’” — Ana Rodriguez, LCSW, Director, Community Affairs and Volunteer Services
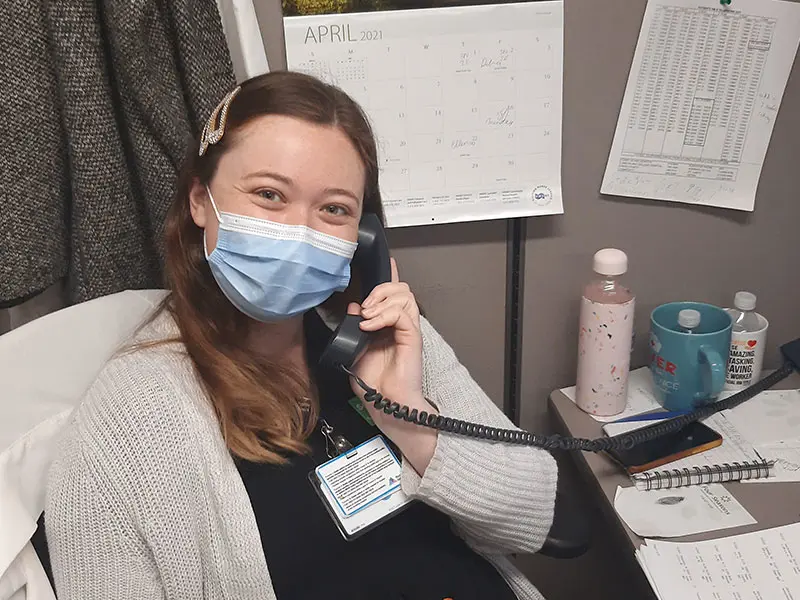
At Mount Sinai Brooklyn, the staff valued face-to-face interactions and connecting with patients. They would also call the patients in their rooms to check on them, or just to chat. This allowed staff to become the visitors patients couldn't have, and helped them build relationships, even though they weren't in the same room. — Emilie Shore, MSc, Patient Representative

Mount Sinai South Nassau
New York Eye and Ear Infirmary of Mount Sinai
Mount Sinai South Nassau anticipated that many members of the community, including seniors and those with mobility issues, may not be able to travel to the hospital to get their vaccination. Using CARES Act funding, the site partnered with Town of Hempstead to purchase and deploy the region’s first Mobile Vaccination Unit, known as the “Vaxmobile,” to bring the vaccine directly to dozens of local communities. So far, more than 1,000 residents have been reached, including many working people who said they simply didn’t have the time to take off work but were appreciative of this convenience. The Vaxmobile has won high praise from elected and civic leaders across the South Shore of Long Island as has the dedicated Vaxmobile staff. — Stephen Rosner, Organizational Behaviorist and Service Excellence
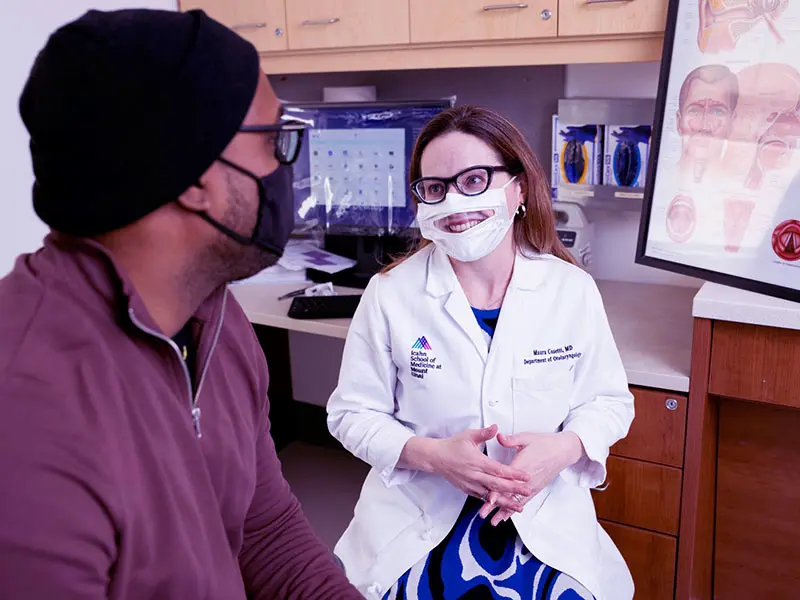
At New York Eye and Ear Infirmary of Mount Sinai, patients with difficulties hearing were negatively affected by the PPE that was needed to protect both patients and staff. The masks provided safety, but presented a barrier to patient communication. In response, the staff used masks that had a transparent feature, allowing patients to see their mouths. This enabled patients to read lips, aiding in communication and making the patients feel more comfortable. This not only helped improve the patient experience, but also helped the staff to connect with the patients they care for. — Shelly Ozdamar, AuD, CCC-A, Audiologist

Mount Sinai Morningside
At Mount Sinai Morningside, staff saw the toll that the pandemic has taken, and wanted to celebrate both the COVID-19 survivors and the teams that helped them heal. To address this, the site created Pause and Applause. Whenever a COVID-19 patient was discharged, many staff went to the lobby to cheer them on as they left. This not only showed compassion for patients, but also engaged teamwork throughout the staff. — Maxine Legall, MBA, LMSW, Director of Patient Experience and Cultural Transformation
Sites across the Mount Sinai Health System showed compassion and made connections during the COVID-19 pandemic.
Our patients, in their own words
“In this difficult time—and considering the staff’s own safety is at risk during the COVID pandemic—everyone I encountered, from the lobby staff checking us in (the screener was on his first day, and
he was so welcoming and professional) to the clinic receptionist, the courtesy and positive mood everyone expressed illustrates leadership that is creating a culture of integrity and compassion.
This does not happen by accident, and the people in charge should take credit for the
extraordinary care I received.”
– Office Visit, Mount Sinai Union Square Center for Post-COVID Care
Featured

The Patient Experience
COVID-19 Response