Ensuring that all patients receive consistent, equitable, and high-quality care requires key performance data that can easily be accessed, analyzed, and acted on. Mount Sinai Health System’s Division of Pulmonary, Critical Care and Sleep Medicine is working to make such data more readily available through the launch of inpatient and outpatient pulmonary dashboards.
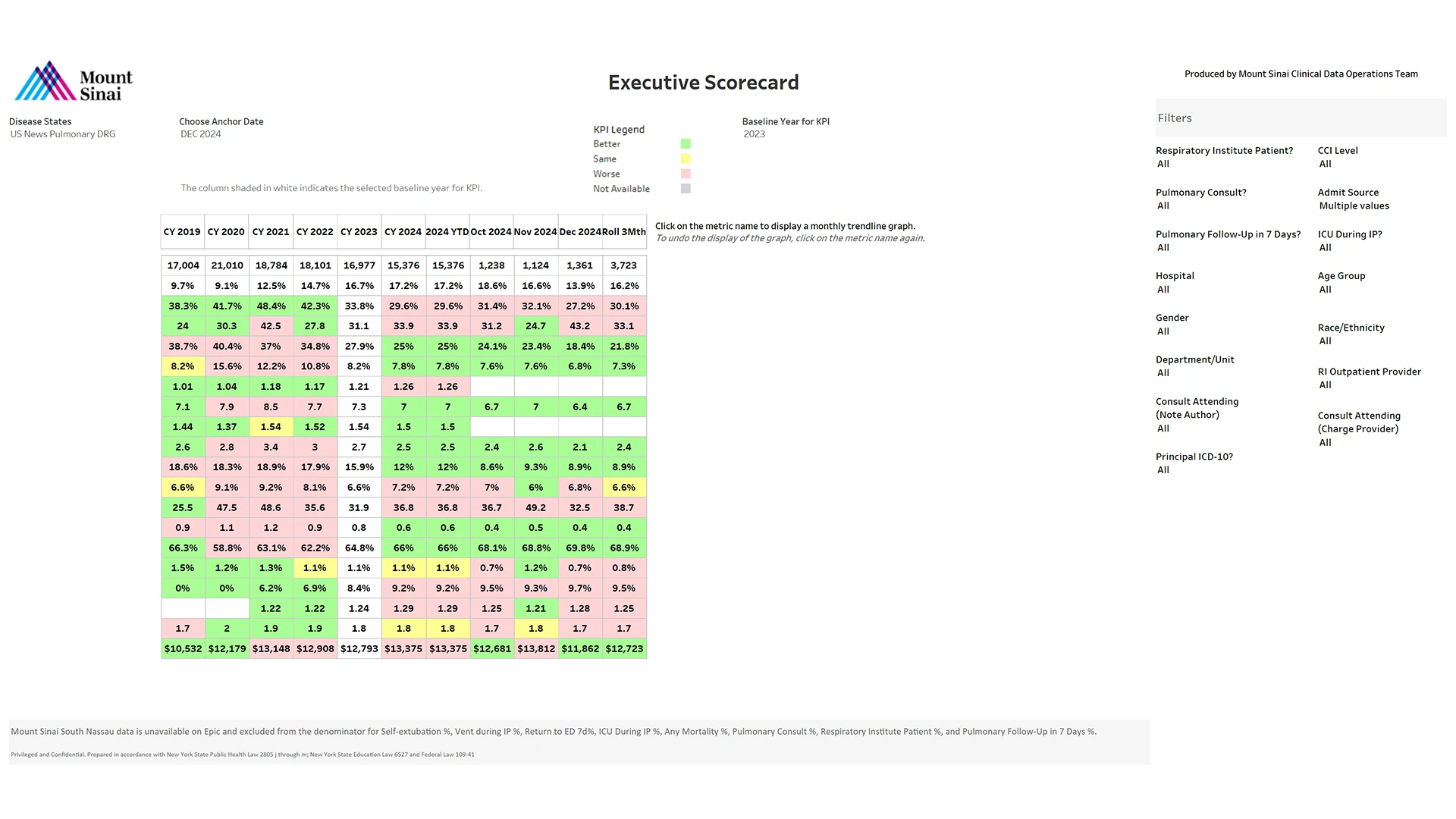
Created in collaboration with Mount Sinai pulmonary leadership, clinicians, the clinical data operations team, data analysts, and health care administrators, the dashboards provide centralized, user-friendly access to key performance indicator data from across the Health System. The data include length of stay, 30-day readmissions, Emergency Department (ED) visits and avoidable utilization, referrals to pulmonary rehab, and discharge disposition.
“We recognized there was a gap in our ability to easily visualize and act on data we were generating across our system,” says Neomi Shah, MD, MPH, MSc, Associate Dean, Faculty Career Advancement, for the Icahn School of Medicine at Mount Sinai, System Vice Chair for Faculty Affairs in the Department of Medicine, and Director of Clinical Strategy and Oversight for the Mount Sinai Respiratory Institute.
“Our dashboards bridge that gap, helping us standardize care and supporting quality improvements among our different patient populations that were not possible with static reports or partial data sources.”
The data are drawn from Mount Sinai’s Epic electronic health record and other systems, providing insights on clinical, operational, and research priorities. They are aggregated at different levels—system, site, provider, and disease cohort—and presented through intuitive visualizations, making it easy to investigate factors such as disease state and patient outcomes.
Although the available data are retrospective, Samira Khan, MPH, Assistant Director of Research and Clinical Initiatives at the Mount Sinai Respiratory Institute, says that is advantageous.
“By analyzing monthly and quarterly trends at the population level, we’re able to assess performance systemwide and compare benchmarks across sites,” Ms. Khan says. “We are also able to identify patterns or variations in care across providers and locations and evaluate the impact of quality improvement efforts. Moreover, we can prioritize areas for intervention with a clear understanding of historical trends.”

Charles A. Powell, MD, MBA, above left, and Dr. Shah are among the Mount Sinai physicians using pulmonary dashboards, like the one below, to improve care quality and use of resources, reduce unnecessary costs, and offer tailored interventions to patients.
Using the dashboards, the Division is identifying variances and gaps in care that are informing targeted interventions to improve care quality and use of resources while reducing unnecessary costs. For example, Dr. Shah and her colleagues conducted an investigation of the relationship between Mount Sinai pulmonary patient hospital experience and readmission rates using Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey scores from the dashboard. They found that patients who indicated they had a good understanding of managing their health had a lower risk for both a 7-day ED readmission and a 30-day hospital readmission. A good understanding of taking medications was also associated with a lower risk for 30-day hospital readmission. These findings were shared in an abstract, “HCAHPS Scores and Their Impact: Pulmonary Patient Readmission Trends at Mount Sinai Health System,” at the 2024 American Thoracic Society International Conference.
“Our early findings underscore the significance of patients’ overall understanding of managing their health as a potential indicator of readmission risk,” says Dr. Shah, who is also Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine) at the Icahn School of Medicine at Mount Sinai. “Based on that, we are looking at tactics such as tailored interventions and leveraging our dashboards to promote patient-centered care and ultimately reduce readmissions.”
Dr. Shah and her colleagues have also conducted investigations of data from different pulmonary cohorts to identify opportunities for improvements. One involving patients with interstitial lung disease (ILD) found that the observed-to-expected mortality ratio was higher among individuals who did not receive a pulmonary consult (1.4 for 308 patients between 2019 and 2023) during their hospital admission compared to those who did (0.9 for 397 patients during the same timeframe). These findings were also shared in an abstract, “Leveraging Tableau Dashboards for Enhanced Inpatient Pulmonary Care: A Data-Driven Approach at the Mount Sinai Health System,” at the 2024 American Thoracic Society International Conference.
“We subsequently discussed how high-risk ILD patients can be evaluated by our pulmonary consult service during their hospitalization,” Dr. Shah says. “As a result, our ILD disease lead, Maria Padilla, MD, along with her ILD fellow, now reviews the daily list of hospitalized ILD patients to identify those who may benefit from a timely consult.”
The dashboards have also enabled the introduction of several new initiatives that are contributing to enhanced patient care. They include “numbers day,” in which physicians develop data-driven presentations highlighting achievements and areas for improvement and quarterly disease management meetings during which dashboard metrics are reviewed.
“The expectation is that the data provided will generate two or three actionable items, with clear ownership assigned to site or provider leads,” Dr. Shah says. “We then track progress on those items using dashboard metrics in the following quarter to ensure follow-through, evaluate impact, and identify opportunities for further improvement.”
Dr. Shah is interested in introducing cohort-specific tracking dashboards and tailoring high-risk patient cohort definitions for each disease state to increase use among outpatient physicians. She is also interested in including additional diseases and subspeciality metrics, as well as patient-reported outcomes, where feasible. Long-term plans include the development of predictive models and the integration of the dashboards into daily workflows and with Epic.
“The ultimate goal is for everything we do to be data-driven,” Dr. Shah says. “It’s not enough to rely on anecdotal evidence or the belief that we’re doing well—we should be able to demonstrate our impact with data at every single meeting, and communicate that clearly to our physician peers, our patients, and the Health System.”
Featured

Neomi Shah, MD, MPH, MSc
Associate Dean, Faculty Career Advancement; System Vice Chair for Faculty Affairs, Department of Medicine; Director of Clinical Strategy and Oversight, Mount Sinai Respiratory Institute

Samira Khan, MPH
Assistant Director of Research and Clinical Initiatives, Mount Sinai Respiratory Institute
