For most cancers, tumor size is an important consideration in patient staging and prognosis. Finding an analogous metric for patients who present with pleural mesothelioma has not been easy, according to Mount Sinai’s Andrea Wolf, MD.
"There have been staging systems that attempted to retrofit the concept of tumor size, but they were not predictive of survival,” explains Dr. Wolf, a specialist in general thoracic surgery and Director of the New York Mesothelioma Program at the Mount Sinai Health System.
“The pleura is unique in that it is like a blanket in its healthy form. It is microns thick, but when it gets a tumor, it thickens. One of the most important discoveries we have made in the last 15 years is that pleural thickness matters a great deal for survival in mesothelioma and it can be measured in a standardized way.”
That discovery informs the forthcoming ninth edition of the TNM Staging System for Pleural Mesothelioma. Developed by the International Association for the Study of Lung Cancer’s mesothelioma cancer staging and prognostic factors committee, the revised edition recommends pleural thickness measurements in three areas based on computed tomography (CT) as a prognostic tool in clinical tumor staging.
“What we have found through our research is that having a higher sum of maximum pleural thickness at three specific levels measured in the axial plane predicts worse survival,” says Dr. Wolf, a committee member and co-author of the revised ninth edition.
“The measurement technique is explained to allow generalized application, but for most people, the details are not as important as the big picture,” she continues. “What is important is that we now have a standard way of measuring these tumors that is reproducible, reliable, and helps us establish guidelines for therapeutic interventions.”
Dr. Wolf says the revised manual is based on a review of the Association’s international registry of patients with pleural mesothelioma. The revisions are informed by data submissions solicited for patients diagnosed between 2013 and 2022, with expanded data elements such as pleural thickness, updated surgical nomenclature, and molecular markers.
The resulting database consisted of 3,598 cases from Europe, Australia, Asia, North America, and South America. Patients had a median age of 71 (range: 18-99); 77.1 percent (2,775) of them were male. The database also included more patients undergoing nonsurgical treatment than prior iterations, with only 1,310 undergoing curative-intent operations (36.4 percent). That percentage is down from 52.7 percent in the eighth edition (1,291) and 64.5 percent in the seventh edition (1,494), reflecting the fact that more patients are being managed nonsurgically. An executive summary of the database review, “The International Association for the Study of Lung Cancer Pleural Mesothelioma Staging Project: Expanded Database to Inform Revisions in the Ninth Edition of the TNM Classification of Pleural Mesothelioma,” was published in the Journal of Thoracic Oncology in early 2024.
“When you have a unique or rare cancer such as pleural mesothelioma, every patient is essentially a case report,” Dr. Wolf says. “An individual clinician may see a handful their entire life. If you were to draw conclusions based on that, it is not really scientific and not reliable. By performing continued assessments of larger, more comprehensive datasets, we start to see patterns that enable us to draw more reliable conclusions about this disease and do the right thing for patients.”
One conclusion the committee made is that there is no reproducible counterpart for pleural thickness in pathological staging, meaning that clinical and pathological staging are not linked directly. This, Dr. Wolf notes, is a novel concept that diverges from the TNM staging systems established for most other solid cancers by the American Joint Committee on Cancer and the Union for International Cancer Control. However, the finding does reflect both the unique nature of the cancer and how it is surgically resected most often through extended pleurectomy decortication.
“Typically, when you remove a piece of the colon, that includes the cancer,” Dr. Wolf says. “That is the same with breast cancer. With mesothelioma, we are literally taking this out in chunks. This means that although pleural thickness can be measured clinically, pre-surgery or pre-treatment, there is no standardized, reliable way for pathologists to measure the thickness because that tissue could be from anywhere.”
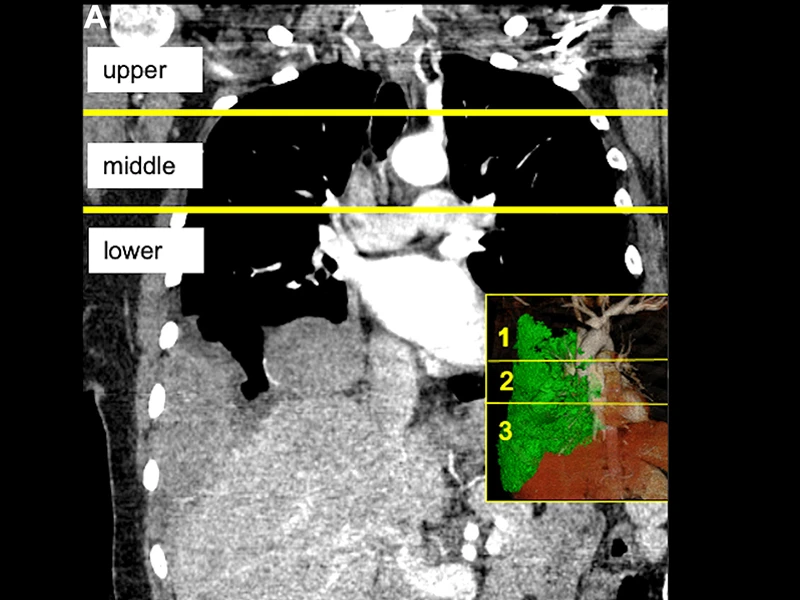
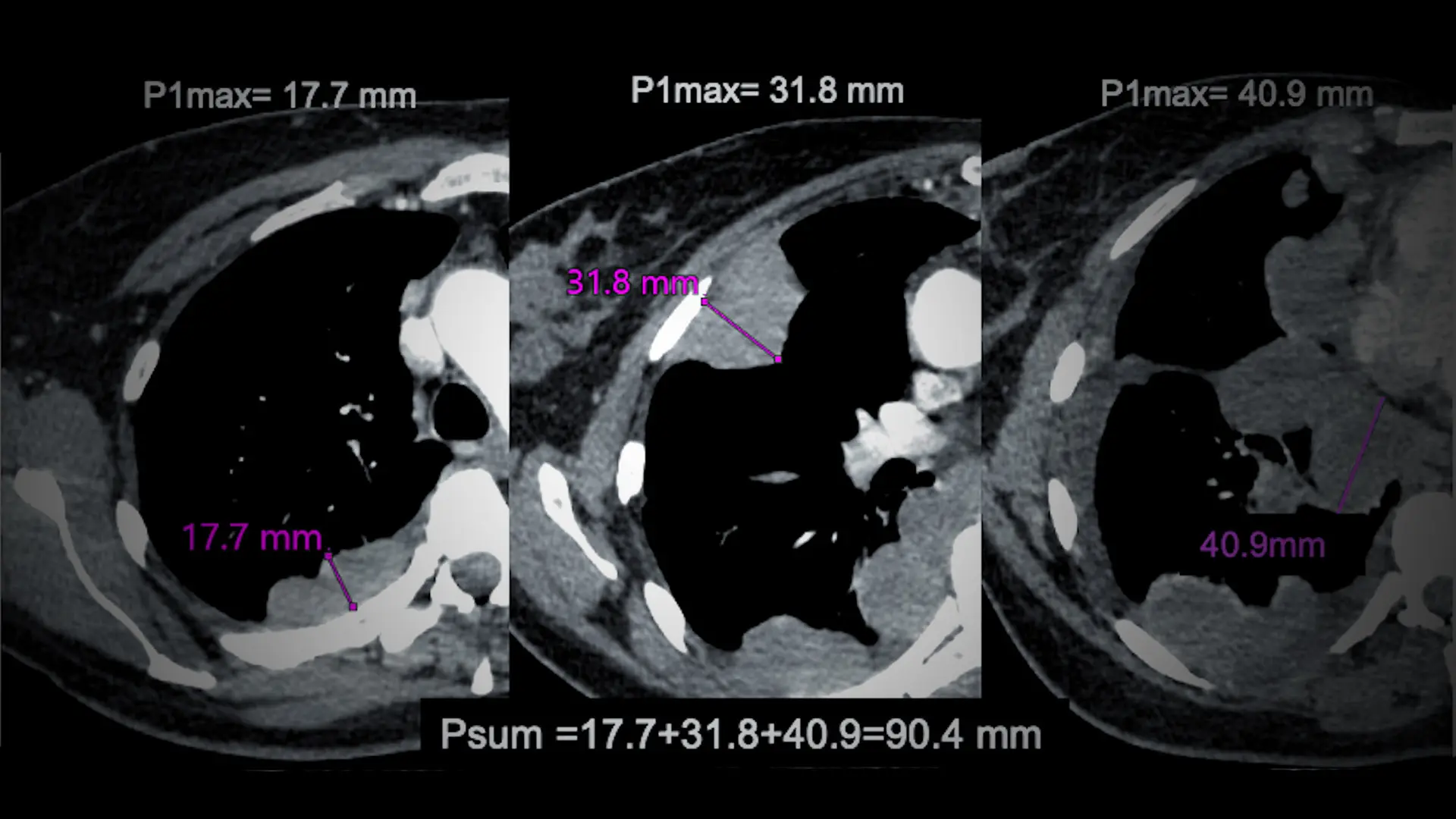
Coronal and sagittal images of patients with pleural mesothelioma illustrating division of the chest into approximate thirds by a line drawn at the level of the aortic arch and a second line at the top of the left atrium, dividing the chest into three relatively equal parts of upper, middle, and lower levels. The maximum pleural thickness on each of these levels (Pmax1, Pmax2, and Pmax3) is measured and combined to derive a sum of maximum pleural thickness (Psum=Pmax1 + Pmax2 + Pmax3).
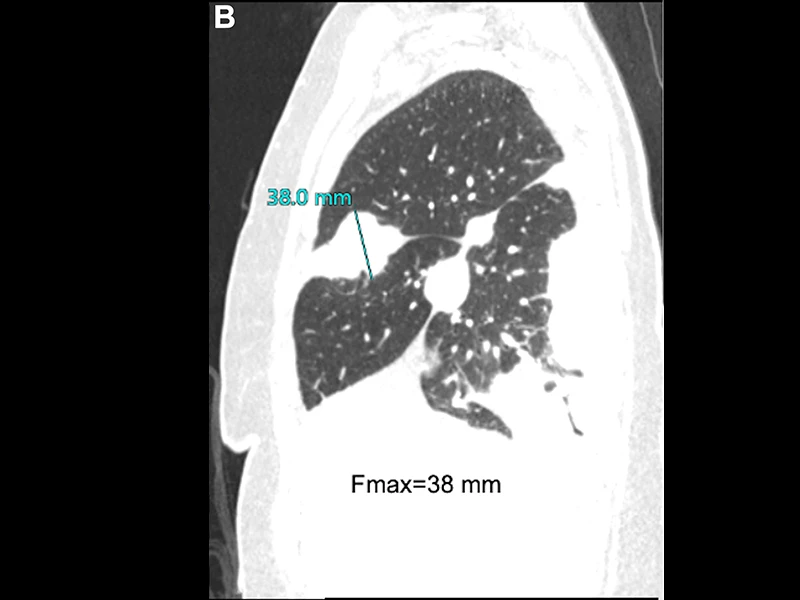
Sagittal image revealing fissure involvement by tumor; maximal fissure thickness Fmax=38 mm
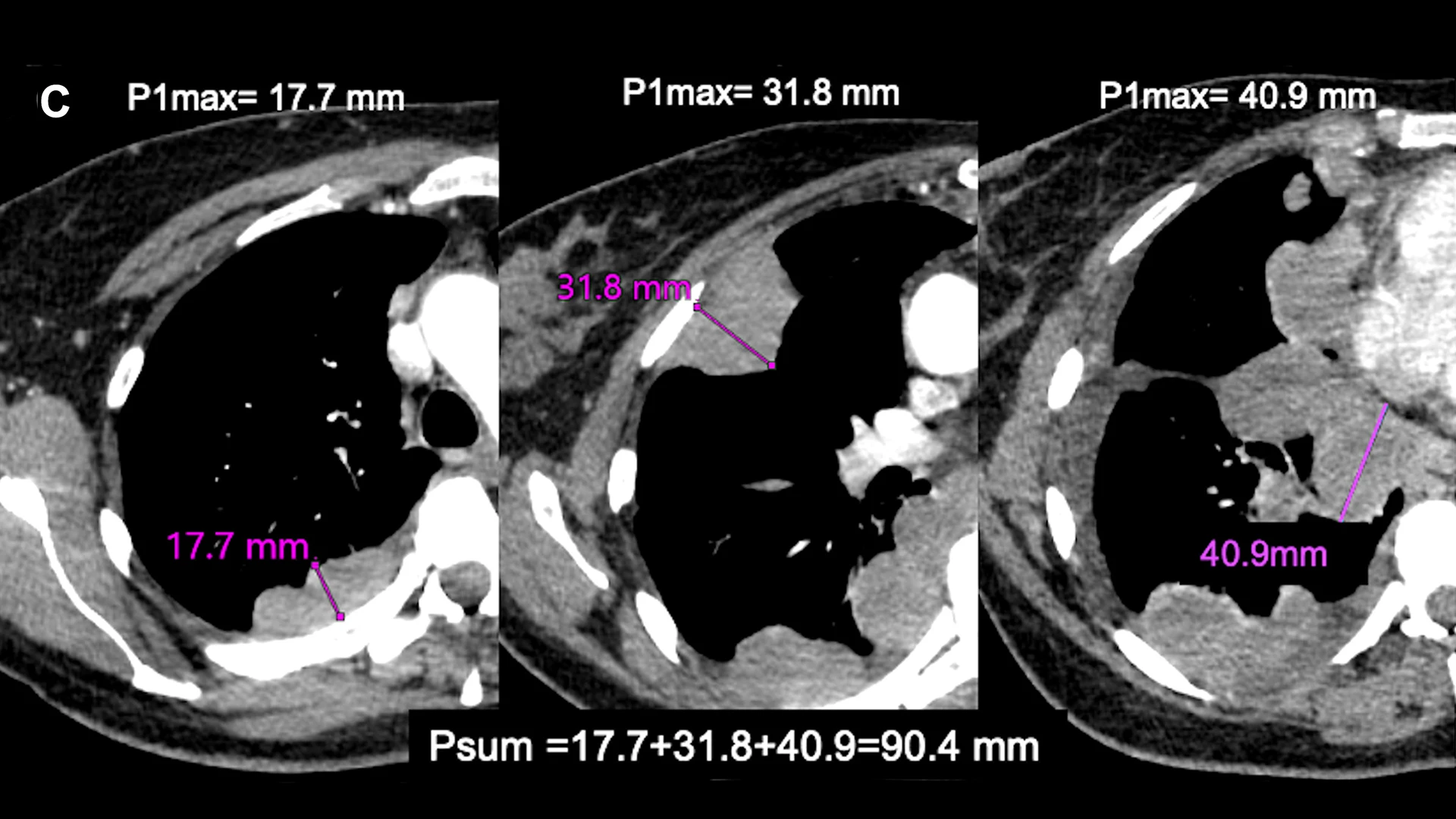
3. Axial images with maximal pleural thickness measurement at each of the three levels; P1max=17.7 mm; P2max=31.8 mm and P3max=40.9 mm, and Psum=17.7 + 31.8 + 40.9=90.4 mm
The committee’s dataset review also confirmed that the location and number of metastatic disease sites is not as significant in terms of patient outcomes as is the presence of metastatic disease. “For example, having metastatic disease in the bone versus in the liver, or having it in both, does not affect a patient’s survival differently,” Dr. Wolf says. “What we are finding is that having metastatic disease is bad and not having it is good.”
Having completed work on the ninth edition of the TNM staging manual, Dr. Wolf expects to reconnect with the committee in the coming months to start laying the groundwork for the 10th edition. She anticipates that she and her colleagues will focus on the potential of biomarkers and the efficacy of immunotherapies. This research demonstrates how far the field has advanced since Mount Sinai’s Irving J. Selikoff, MD, first identified the relationship between the disease and asbestos exposure in the 1960s. It also dovetails with Dr. Wolf’s own efforts to better understand outcomes and disparities among patients with pleural mesothelioma.
“The more we can standardize evaluation, the more we can individualize treatment strategies for individual patients, which is going to be the key,” she says. “Collaborations like this committee are the way we are going to get there.”