More than 60 percent of the 1.5 million new incidental lung nodules (ILNs) detected nationwide each year will be lost to follow-up. Through an innovative new ILN safety-net program, Mount Sinai’s Javier Zulueta, MD, is working to reduce that percentage to zero.
Launched in January 2023, the program uses natural language processing to scan all Mount Sinai Morningside and Mount Sinai West chest-related radiological reports for any reference to nodules—including related terminology such as lesions and nodularity—and radiologist recommendations. These results and the patients’ computed tomography (CT) scans are then reviewed by the program navigator and a physician assistant to identify patients who should be engaged or tracked based on their risk for cancer.
“There are other centers that follow nodules or that have lung nodule clinics, but I am not aware of many that are taking a systematic approach to the management of patients with these nodules as we are doing with our program,” says Dr. Zulueta, Professor of Medicine at the Icahn School of Medicine at Mount Sinai and Chief of the Division of Pulmonary, Critical Care and Sleep Medicine at Mount Sinai Morningside.
To ensure the program is focused on ILNs, patient radiology reports and, at times, electronic health records are reviewed to identify cases involving known, benign, and no nodules. The exclusion criteria include false positives, calcified nodules, nodules being tracked through other studies, and cases where the radiologist recommends no further follow-up. These criteria typically result in the exclusion of 35 percent of cases.
Patients who are recruited to the program are then assessed for cancer risk based on factors such as age and history of smoking and whether they have an established follow-up pathway. Those who do not have a follow-up pathway are engaged immediately by the program navigator, who discusses their scan findings and offers them an opportunity to book a next-week appointment with the program’s nodule clinic. These patients are then tracked to ensure they continue with their follow-ups. Patients with an established follow-up pathway are also tracked, with engagement occurring only in instances where they miss a follow-up CT scan.
“We typically call the patient’s pulmonologist or primary care provider to let them know the CT scan was missed and ask them if they want us to get involved,” Dr. Zulueta says. “If they do, we contact the patient and offer to book them for an appointment at our clinic.”
A retrospective study of the program conducted between January 2023 and January 2025 shows that it has led to improved follow-up rates among Mount Sinai Morningside and Mount Sinai West patients with ILNs. Of 8,217 patient scans potentially containing lung nodules, 5,212 were included in the program. Of these, 2,205 (42 percent) had non-incidental nodules (discovered through, e.g., lung cancer screening); patients in this group were contacted and engaged only if their recommended follow-up was past due, while the rest were just tracked. Among the 3,307 patients with incidental nodules, 61.1 percent did not have an established follow-up pathway and were contacted and engaged, while 38.9 percent did have such a pathway and were only tracked.
Of the 2,256 studies that resulted in engagement, 29 patients were diagnosed with lung cancer, with 23 (79%) in stages I or II (Table 2). Among the 2,824 studies that were only tracked, 70 patients received a lung cancer diagnosis, with 33 (47%) in stages I or II. This indicated, the researchers said, that engaging patients leads to more cancers being caught in early, curable stages. Also, the program's design allowed for more focused use of resources by limiting the engagement efforts to patients who did not have an established follow-up evaluation plan or had fallen behind on that plan.
Preliminary results of the study were presented at the 2024 American Thoracic Society Meeting, and fuller results will be presented at the 2025 meeting.
"These results show that we are detecting cancers and we're helping to engage patients who are not getting their follow-ups done," Dr. Zulueta says.
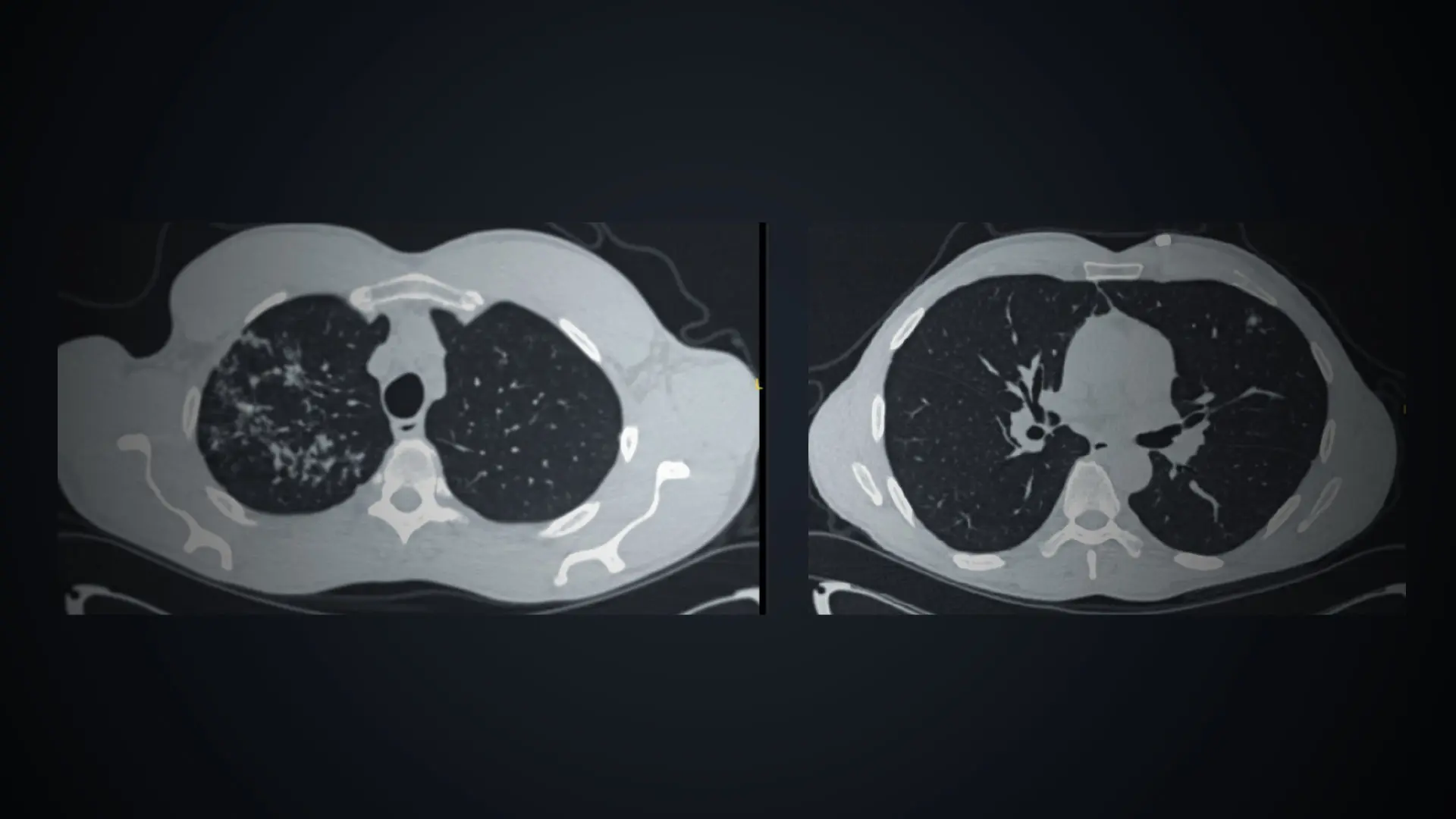
It is not just engaging patients with ILN where the program is making a difference. Dr. Zulueta says this safety net is facilitating diagnoses of other diseases among patients. Perhaps the most notable instance involved a patient who had been flagged after undergoing a coronary CT angiogram. The scan revealed a nodule on the left lung near the heart.
“In cases like that, we typically recommend a full CT of the chest,” he says. “In this case, the full scan also revealed a host of nodules and infiltrates on the upper right lobe, which indicated tuberculosis. This was a patient who was asymptomatic and thus posed huge public health risks; however, we were able to catch it early and deliver treatment as a result of this program.”
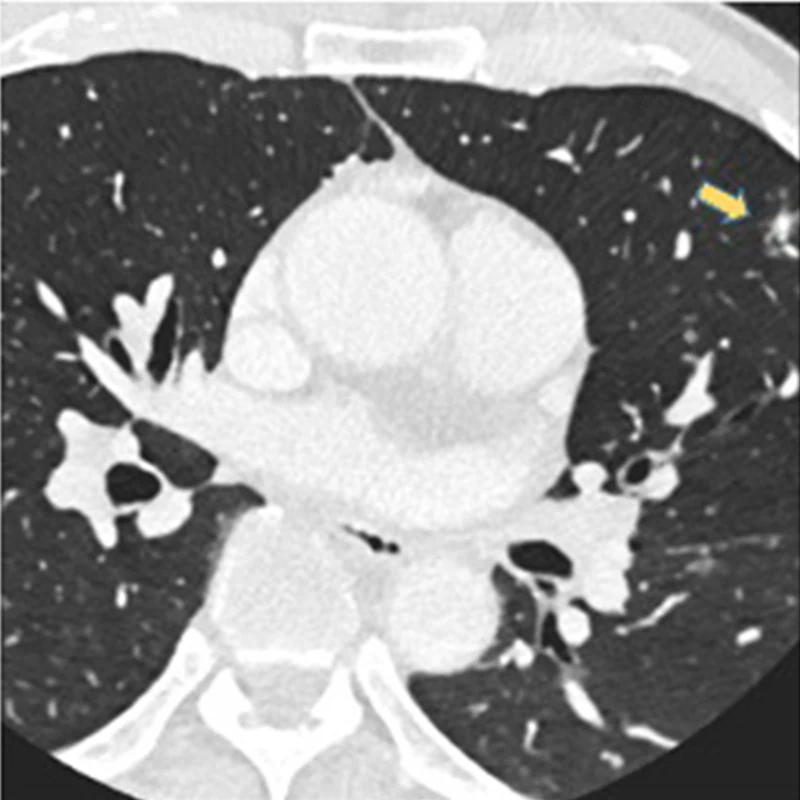
On a coronary angiogram, a nodule is visible in the upper right-hand corner, corresponding to the left upper lobe.
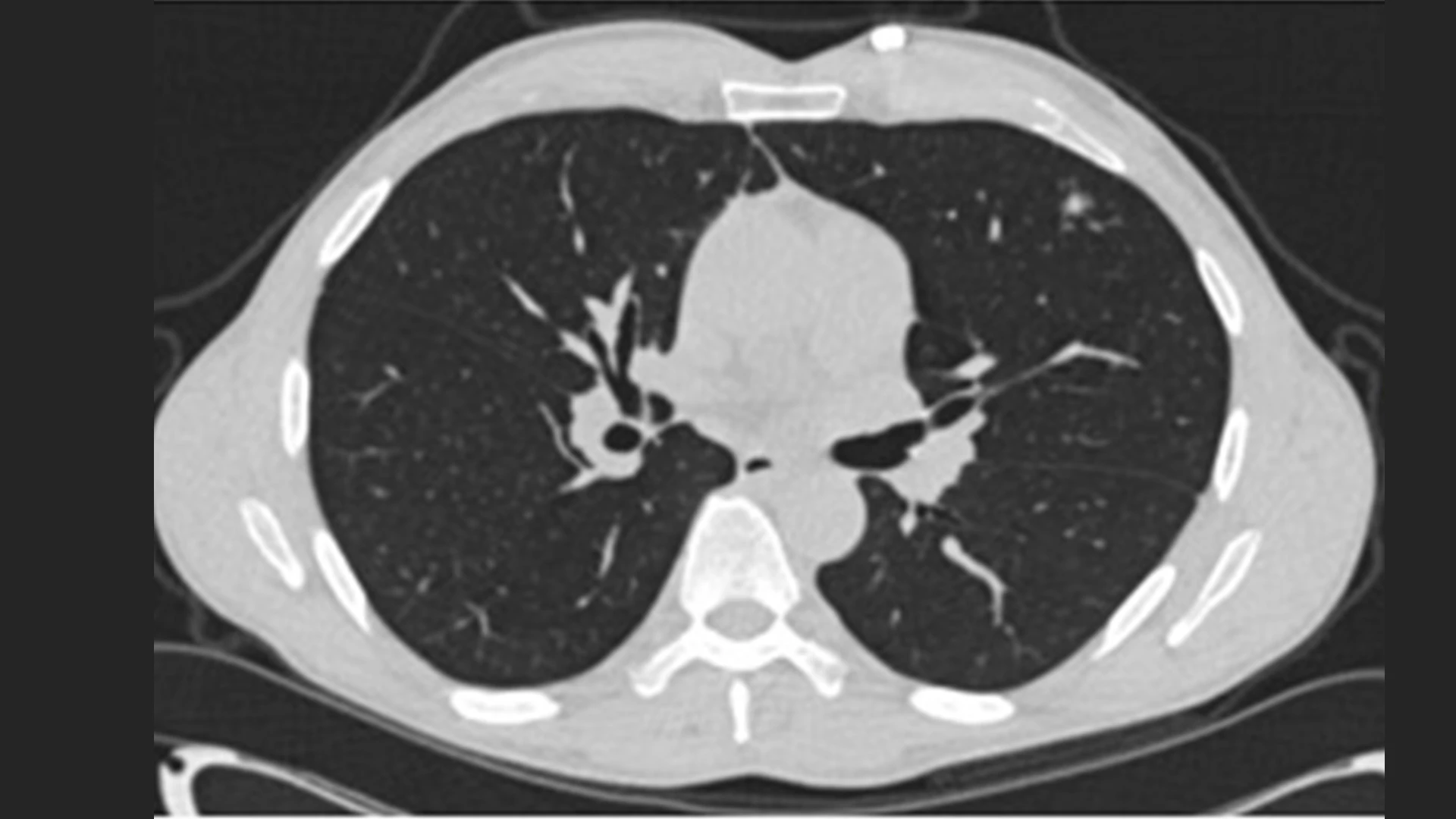
The patient's full chest CT confirmed the nodule in the left upper lobe.
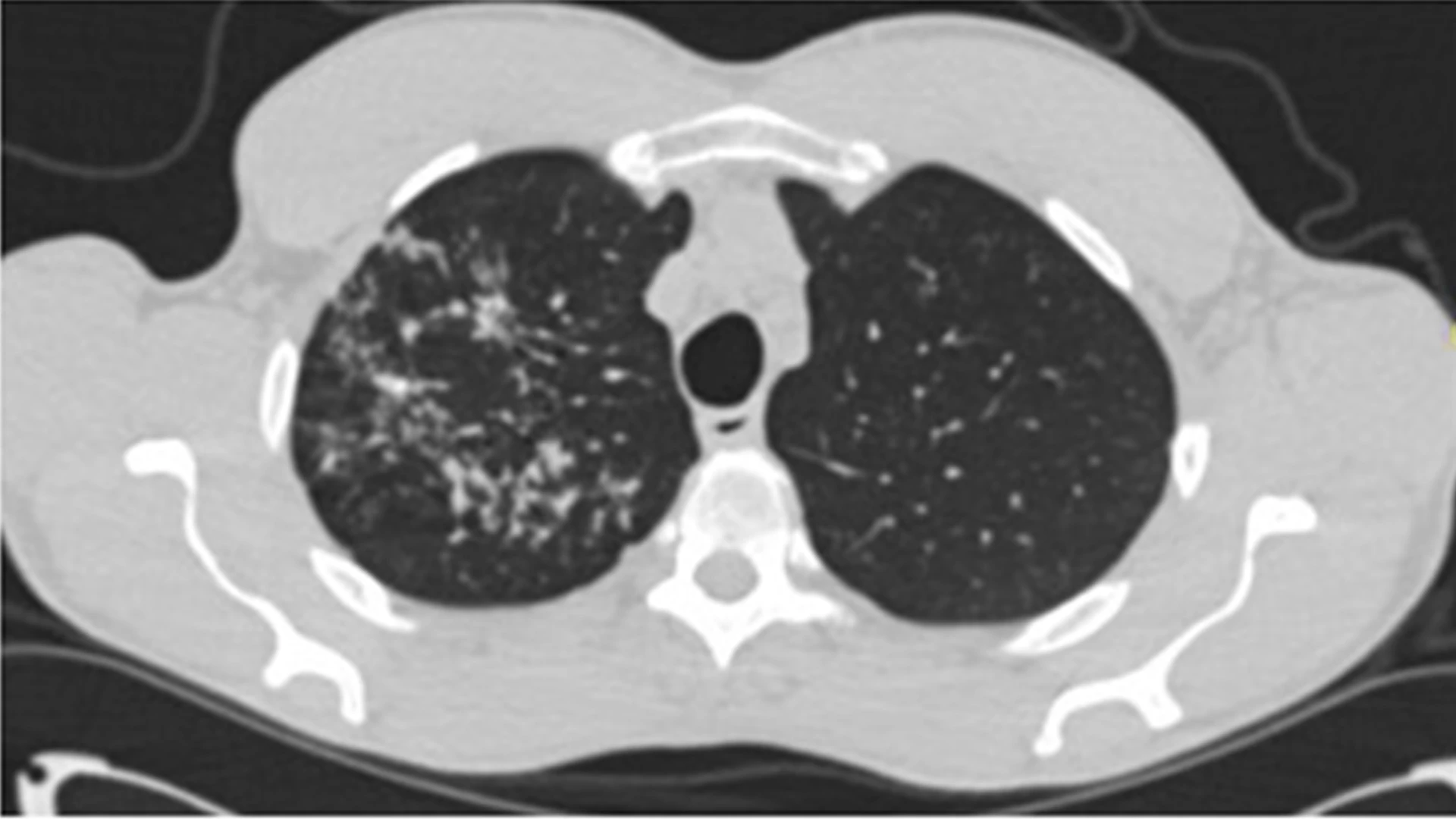
The chest CT also showed a nodular infiltrate in the right upper lobe. A bronchoscopy was performed and obtained positive cultures for tuberculosis.
Based on these successes, Dr. Zulueta plans to expand the program across the entire Mount Sinai Health System and conduct a retrospective study to determine which patients with ILN are also candidates for lung screening based on risk factors. But he also has more ambitious plans in mind: He is working with Mount Sinai’s Biomedical Engineering and Imaging Institute to explore the potential of using AI to directly scan patient imaging for incidental lung nodules. This, he believes, will result in more detailed insights on these nodules and their associated risks for cancer.
“AI is going to change our practice completely in many aspects, but in particular, it is going to make it much more efficient and much safer for patients,” he says.
Featured

Javier Zulueta, MD
Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)