The CFTR protein is well known to pulmonologists for its role in cystic fibrosis (CF), a relatively rare disease. Not widely known among clinicians is how this protein might figure in the infinitely larger landscape of lung infection and pneumonia. That prompted Mount Sinai physician/researcher Jaime Hook, MD, to see great value in the exchange of ideas and information among members of the relatively small lung research community that could push the boundaries of CFTR science.
Her receipt of a grant from the Cystic Fibrosis Foundation a year and a half ago led to her creation of the Regional Cystic Fibrosis Research Consortium, which has since met twice to pore over cutting-edge work emanating from some of the top labs in the field to promote a better understanding of CFTR and how it could lead to new therapies for lung infections.
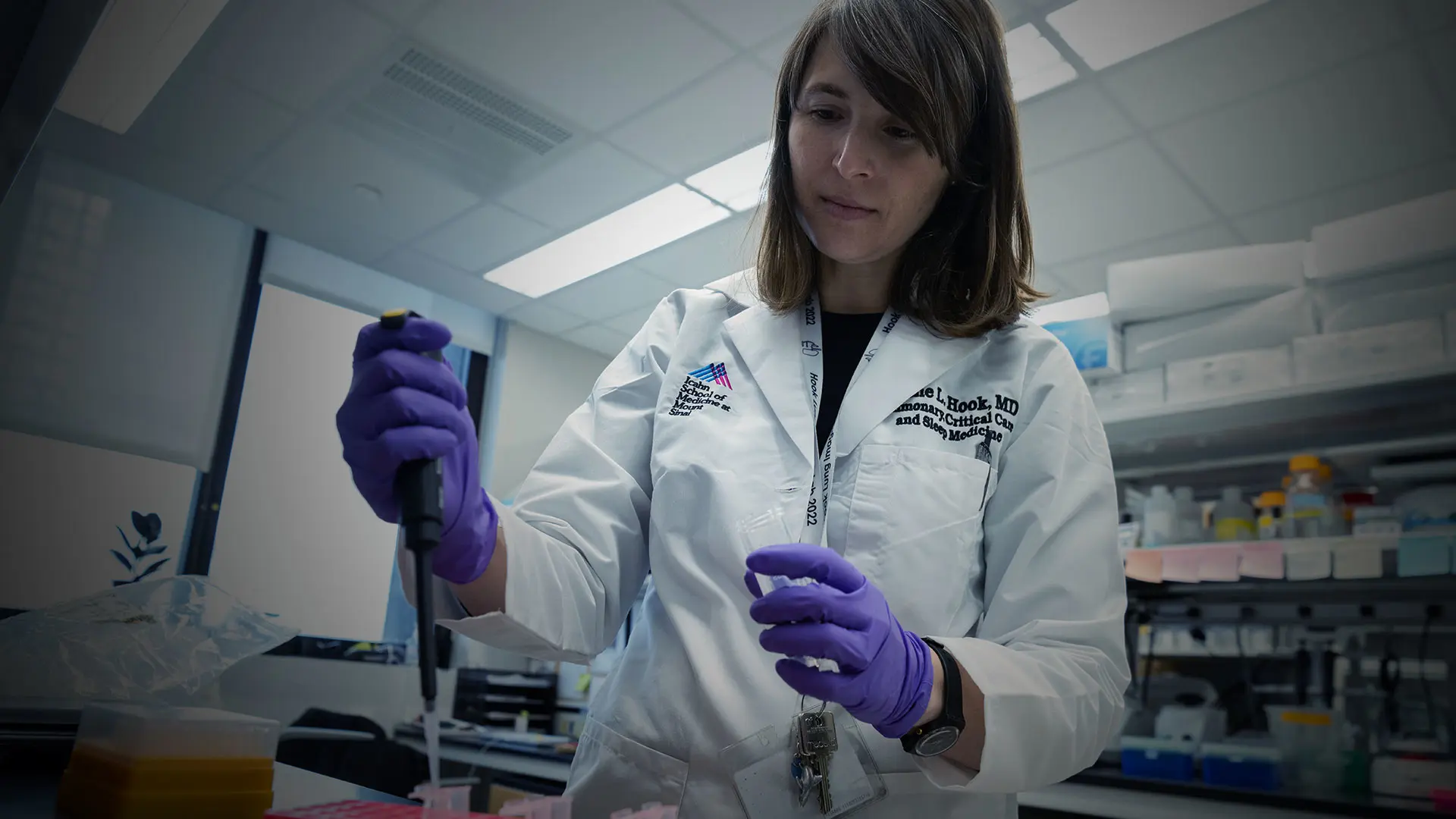
“My goal was to use some of that funding to bring together my lab and another one at Mount Sinai that were investigating CFTR in the context of pneumonia to review the work we were both doing,” recalls Dr. Hook, Assistant Professor of Medicine (Pulmonary, Critical Care, and Sleep Medicine) at the Icahn School of Medicine at Mount Sinai. “We then decided to broaden the scope to include other groups in New York City and regionally, and added Columbia and Yale to our consortium of five labs led by experts who are breaking new ground in their fields.”
The CFTR protein has traditionally been viewed by science through the lens of cystic fibrosis and, therefore, in the context of an airway disease. This perspective was reinforced by studies showing that mutations in the CFTR gene, which provides instructions for producing CFTR proteins, heavily impact the airways, as seen in patients who have trouble coughing up thick, sticky mucus. This occurs when CFTR proteins, which help to maintain the balance of salt and water on many surfaces of the body, fail to properly push chloride and water out of the cells. As a result, water cannot hydrate the cellular surface, causing mucus in the airways to thicken and get stuck, making breathing difficult.
“A new idea is surfacing that the lung’s air sacs, which dwarf the surface area of the airways, might be important in cystic fibrosis,” says Dr. Hook, “and we are at the forefront of that thinking because our research focuses on CFTR function specifically in the air sacs.”
That novel research was front and center at the recent session of the CF consortium, where Dr. Hook presented evidence that the air sac epithelium expresses CFTR and plays an important role in lung homeostasis. “Our work is designed to help us better understand the next step, namely, when things go wrong, whether it’s a flu infection or CF, how can we target those air sacs to make the lungs function better. Very few people in the field are talking about this.”
Dr. Hook hopes that research into a protein associated with cystic fibrosis will bring benefits for many other lung diseases as well.
Which serves to underscore the very mission of the consortium: to advance the emerging science of how CFTR functions in the respiratory tract as a way to discover effective new treatments. To that end, the 22 attendees at the recent forum listened intently as Sebastian Riquelme, PhD, Assistant Professor of Immunology at Columbia University Irving Medical Center, described his lab’s work on how bacteria interact with the CF lung, an incipient avenue of research. Alice Prince, MD, Professor of Pediatrics at Columbia, outlined how bacteria exploit the lung to establish a chronic infection.
Additional insights came from Clemente Britto, MD, Assistant Professor of Medicine at Yale School of Medicine, who put into clinical context the body’s immune responses to cystic fibrosis and how that affects people who are taking CFTR modulator drugs. Alison May, PhD, Assistant Professor of Cell, Developmental, and Regenerative Biology, and Otolaryngology, at Mount Sinai and a stem cell biologist, detailed for the group how the CFTR protein impacts the development of the salivary glands and the respiratory glands in the large airways in the lung.
The enthusiasm shown by participants at meetings to date, along with the robust scientific back-and-forth, has raised expectations by Dr. Hook for what the group might be able to achieve in the longer term.
“Recently we’ve begun to discuss the nuts and bolts of how we might develop new collaborations,” she acknowledges. “This gets into themes such as what research our labs undertake, what do we need help with, and could there be some complementary expertise to help each other and share responsibility for projects?”
For Dr. Hook personally, the success of the research consortium serves to validate the reason she created it.
“As a relatively new investigator, I can appreciate how critical it is to have good relationships with others in the field,” she says. “When you’re not only working on your own projects but contributing even a little bit to others, you’re increasing your impact, influence, and reach. Our consortium may ultimately help us translate scientific discoveries into new treatments for patients, and that’s really the goal.”