A multidisciplinary approach to managing lung nodules is streamlining diagnosis and treatment for patients at the Mount Sinai – National Jewish Health Respiratory Institute. Launched in 2022, the Mount Sinai Multispecialty Lung Nodules Diagnostic and Treatment Program builds on Mount Sinai Health System’s position as a leader in diagnosing and treating lung cancer. The program’s new, integrated approach brings together multiple specialists to improve care for patients with suspicious lung nodules.
Despite advances in lung cancer treatment, the disease remains deadly. “More people die of lung cancer than the next three common cancers combined—colon, breast, and prostate cancers,” says Timothy Harkin, MD, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Thoracic Surgery, at the Icahn School of Medicine at Mount Sinai. “And we know that the stage of lung cancer at the time of detection is a major determinant in survival.”

Timothy Harkin, MD
Managing Lung Nodules From Screening and Incidental Findings
Fortunately, physicians and the public are becoming increasingly aware of the importance of low-dose computed tomography (CT) screening for people who smoke or smoked and others at high risk of lung cancer. Such screenings can identify suspicious lung nodules that require further evaluation.
Incidental lung nodules also turn up on imaging done for other purposes, such as coronary calcium scans or chest X-rays following trauma. Patients with a nodule—whether identified through screening or incidentally—may be referred to the Lung Nodules Program.
Next steps are informed by standardized approaches guided by cancer risk assessment, including the Fleischner Society Guidelines for managing pulmonary nodules detected incidentally on CT images and the American College of Radiology's Lung CT Screening Reporting & Data System (Lung-RADS®) for nodules identified on lung cancer screening CTs. Determining the best option among those suggested by the guidelines involves several considerations. The Lung Nodules Program takes an integrated approach to assessing those factors.
“In one visit, patients in the program meet with several specialists, including a pulmonologist, interventional pulmonologist, oncologist, and/or thoracic surgeon, as indicated by the presentation. Then our team members confer and deliver a combined recommendation to the patient,” explains Charles A. Powell, MD, MBA, the Florette and Ernst Rosenfeld and Joseph Solomon Professor of Medicine at Icahn Mount Sinai, and Chief of Pulmonary, Critical Care and Sleep Medicine for the Mount Sinai Health System. “This approach is unique because multidisciplinary consultation has been integrated to a single point of care, without having to refer the patient to multiple specialists.”
Lung Nodules Classification and Diagnosis
The multidisciplinary program was born from recent advances in classifying lung nodules. Those discoveries have helped pinpoint which lung nodules likely require immediate intervention and which can be monitored for change over time. Smaller nodules, Dr. Harkin notes, are less concerning. “We’ve learned that size matters a lot. Nodules under about 6 millimeters are much more likely to be benign, while nodules over that size are more likely to be cancerous,” he says.
Yet even malignant nodules may not require immediate intervention. Much like prostate cancers that can stay localized for years without causing problems, some lung tumors are unlikely to grow and spread quickly, if at all. Research from labs, including Dr. Powell’s, has helped paint a picture of which nodules are concerning. “Our investigations have discovered distinct subtypes of lung adenocarcinoma, which range from indolent to very aggressive,” he says.
Those subtypes look different from one another on CT scans. “Indolent lesions tend to be characterized by nodules with a ground-glass appearance. Nodules that are more aggressive tend to have a solid appearance on imaging studies,” Dr. Powell says. “In the past, the management approach to those two types of nodules would have been the same. Now that we can distinguish subtypes based on imaging, we’re more comfortable following the low-risk lesions and intervening only when there has been a significant change.”
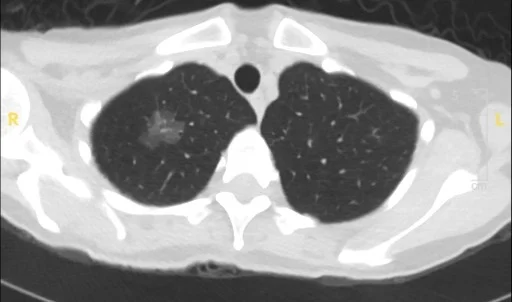
CT image of ground-glass and part-solid nodules taken in 2019
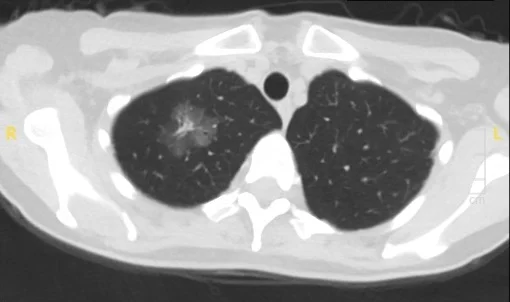
Same patient rescanned in 2023
Importantly, research also suggests that this watch-and-wait approach doesn’t increase risk to patients. “I’ve been monitoring some patients for 15 years with no changes to their indolent tumors,” Dr. Powell says. “And we’ve learned that when we do detect a change on imaging, we have sufficient time to intervene.”
Other recent innovations in lung cancer diagnosis and treatment are improving care for patients in the Lung Nodules Program. “We have a wealth of research experience to inform our management of patients with pulmonary nodules, and our team is ahead of the curve in implementing advances in diagnostics and treatment for patients with lung cancer,” Dr. Powell says.
In 2023, the Respiratory Institute adopted a robotic platform for bronchoscopy. “The robotic system allows us to target small nodules more precisely and to access and biopsy nodules in difficult-to-reach locations that we would never have attempted before,” Dr. Harkin says. Performing bronchoscopy to biopsy suspicious nodules also enables pulmonologists to use endobronchial ultrasound to look for lymph nodes in the chest during the same procedure. “If we’re highly suspicious of malignancy, we can perform a biopsy of the nodule and assess lymph nodes essential for staging the cancer in a single procedure instead of the traditional two,” he adds.
The Importance of Lung Cancer Screening
As leaders in research and management of lung nodules, the multidisciplinary experts of the Lung Nodules Program are committed to raising awareness about the latest findings in the field. In 2023, the team organized a pulmonary continuing education course for professionals, with sessions allocated to diagnosing and managing lung nodules.
Physicians should also be aware of the importance of following up with nodules found incidentally, Dr. Harkin says. “Whenever nodules are discovered, they need to be assessed. When a nodule is found on a scan ordered by a primary care doctor or cardiologist, we are happy to take care of the follow-up to ensure the patient is receiving the appropriate management,” he adds.
Although knowledge of lung cancer screening is growing, there is still work to be done, adds Scott Scheinin, MD, Professor of Thoracic Surgery at Icahn Mount Sinai.
“If you wait until you have symptoms of lung cancer, the likelihood of a cure is much less. Research shows that, with early detection, mortality goes down,” Dr. Scheinin says. “There’s a certain mindset in the general population of ‘don’t ask, don’t tell.’ But we need to change that and continue educating the public about the importance of screening and early detection.”
