Stenting to open complex and tortuous airway passages is entering a new era, and Mount Sinai is among a handful of sites across the world whose interventional pulmonologists are paving the way.
By bronchoscopically placing 3D-printed stents in the trachea or main bronchi, physicians are ensuring a more precise and comfortable fit for patients with central airway obstruction from either benign or malignant causes.
Customized 3D-printed devices are currently reserved for patients with the most complex airway anatomies. However, the demand is expected to steadily increase at Mount Sinai, especially with the growth of a newly established lung transplantation program.
“I see 3D-printed stents as the future for treating complex, benign central airway obstructions that require airway stenting,” says Udit Chaddha, MBBS, Assistant Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Thoracic Surgery, at the Icahn School of Medicine at Mount Sinai, and Associate Director of Interventional Pulmonology, who had performed each of the institution’s six selective placements as of April 2023. “They are ideal in cases where the airway is extremely distorted, and, when fitted properly, help to avoid tissue granulation and migration. All the procedures we’ve done have been quite successful.”
At Mount Sinai, the customization process begins with a CT scan of the patient’s chest. Working with proprietary software that allows 3D visualization of the airway—with all its complex twists, turns, and branching—Dr. Chaddha and his team design the customized stent and upload it to a Cleveland-based company, VisionAir Solutions, the sole supplier of 3D-printed airway stents in the United States. VisionAir Solutions creates a 3D-printed mold made of medical-grade silicone. This custom airway stent is then shipped to Mount Sinai within five business days.
“It’s a streamlined and highly efficient process that produces stents that fit the patient’s airway like a finger in a glove,” explains Dr. Chaddha. “That’s particularly beneficial in cases where an airway has narrowed in multiple segments and dimensions, and a simple, contemporary straight stent just isn’t optimal.”
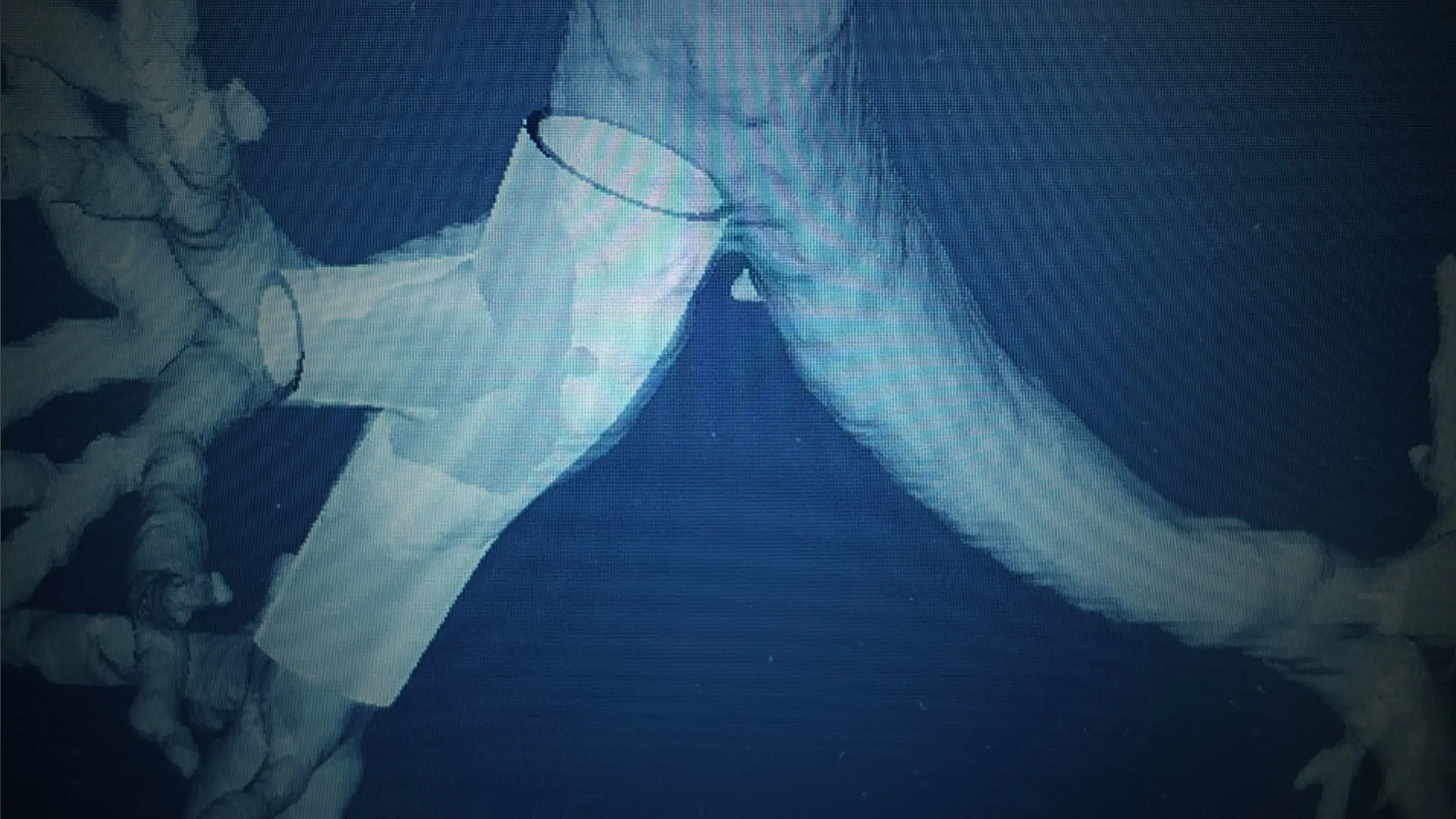
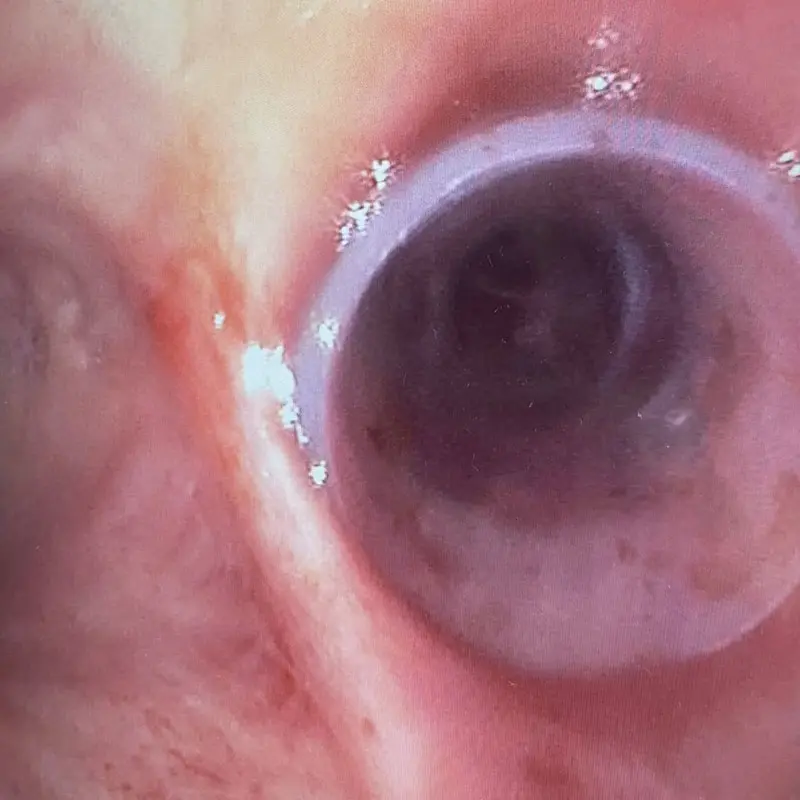
Below: Two views of the right main bronchi after stenting.
View from the trachea
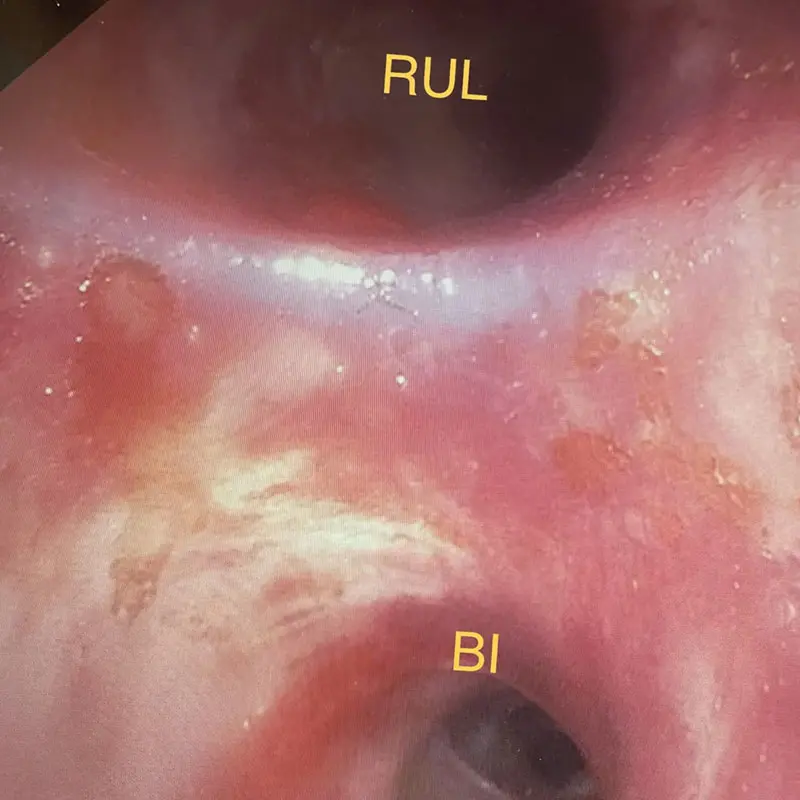
View from the right side
For all their advantages, 3D-printed airway stents pose at least one significant challenge.
“These devices are not easy for pulmonologists or surgeons to place,” explains Dr. Chaddha. “They require specialized training and expertise in rigid bronchoscopy, and a high comfort level with deploying Y-stents. That’s why the procedure must only be performed at centers of excellence around the country.”
The duration of the procedure depends on the complexity of the airway, he adds, but typically is about a half hour. It is done on an outpatient basis unless the patient is already in the hospital undergoing treatment.
Though 3D-printed airway stents are still at an early stage, Dr. Chaddha believes they could, over the longer term, replace standard stenting, particularly for benign central airway obstruction.
“They’re allowing us to open airways we couldn’t open before, and there’s no question we’re becoming more comfortable with the process,” he says. “For those reasons, and the fact that customized stents are no more costly than the ones we’ve always used, my own threshold for using them continues to improve.”
Featured

Udit S. Chaddha, MBBS
Assistant Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Thoracic Surgery