Related Article
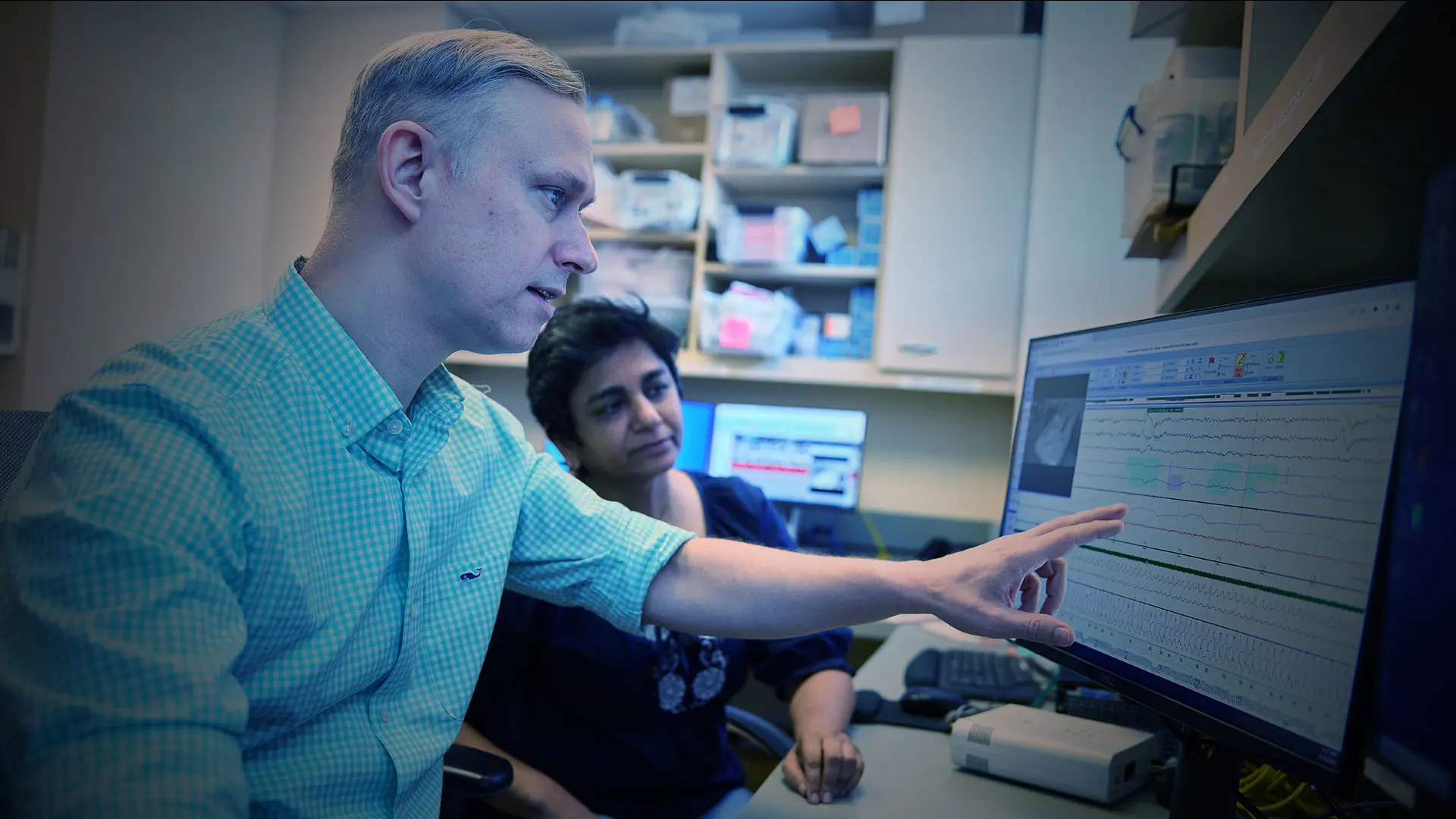
Skipping a few nights of continuous positive airway pressure (PAP) therapy for sleep apnea might not seem like a big deal. But a first-of-its-kind study led by Mount Sinai neuroscientist Andrew W. Varga, MD, PhD, suggests that even a brief withdrawal might increase one’s risk of developing Alzheimer’s disease (AD).
Dr. Varga found that withdrawal from PAP therapy among subjects with severe sleep apnea resulted in significant overnight changes in AD biomarkers and markers of neural injury measured in blood, and that an observed change in neurofilament light (NfL), a marker of neural injury, was significantly associated with apnea-related increases in intermittent hypoxia and sleep fragmentation.
The study, published in the American Journal of Respiratory and Critical Care Medicine, is the first to show an acute effect of sleep apnea on AD biomarkers—a field of exploration that is relatively nascent—but Dr. Varga cautions that these findings necessitate further study.
“For the first time we are showing that sleep apnea significantly induces some measure of neural injury,” says Dr. Varga, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine) at the Icahn School of Medicine at Mount Sinai. “However, we do not know whether that injury is reversible, so the long-term implications remain to be seen. That said, our findings do imply that if an individual continues to skip therapeutic PAP, cumulative neural injury could occur.”
The findings were based on analysis of blood collected in the evening (10:40 pm) and the next morning (6:40 am) across a night of polysomnographically recorded sleep among 30 participants with severe sleep apnea during conditions of therapeutic PAP or the third consecutive night of acute withdrawal from PAP in a counterbalanced fashion. The average age of the participants was 51.5; 27 percent of the participants were women and 67 percent were non-Hispanic white.
Andrew Varga, MD, PhD, and Korey Kam, PhD, use a centrifuge to process plasma for Alzheimer's disease biomarkers in sleep apnea patients who use continuous positive airway pressure therapy.
Dr. Varga and the research team looked at overnight changes in four plasma biomarkers associated with neural injury and AD—total tau; brain amyloid-beta40 (Aβ40) and brain amyloid-beta42 (Aβ42), peptides that contribute to formation of amyloid plaques; and NfL, an axonal protein that is released in response to neural injury and is highly correlated with the progression of the disease—between the two sleep conditions. Plasma samples were analyzed using a single molecular array (SIMOA) Neurology 3-Plex A assay kit, which enables detection of picomolar concentrations of amyloid and tau, and NF-Light™ kits. All samples were tested in duplicate and samples with a coefficient of variation ≥20 percent were excluded from the analysis.
Looking at the samples, the researchers observed a significant decrease in Aβ40 and a significant increase in NfL among participants after a third consecutive night without PAP therapy versus the therapeutic PAP sleep condition. “When we withdrew PAP therapy and induced sleep apnea acutely, the strongest signal we saw was the overnight increases in neurofilament light,” Dr. Varga says.
Although there was no significant difference observed in the other two AD biomarkers between the two sleep conditions, Dr. Varga says there appeared to be a signal for increased tau in the PAP withdrawal condition, and this warrants further study. There was no difference in all four AD biomarkers between the two sleep conditions at the start of the night within subjects.
Based on those findings, Dr. Varga and the research team subsequently investigated whether there are sleep physiology predictors of the biomarker changes that they observed. They looked at several sleep physiology biomarkers driven by PAP withdrawal and found that the number of sleep stage transitions—a marker of sleep fragmentation—and the amount of time below 90 percent O2 saturation were significantly associated with NfL. However, no identified sleep physiology biomarkers predicted the overnight change in Aβ40.
“There is considerable debate in the apnea field about what the apnea hypopnea index, or AHI, means,” Dr. Varga says. “There are those who believe it is bad to have a high AHI even if no events are associated with significant dips in oxygen. In the cardiovascular field, the consensus is that only intermittent hypoxia matters. Our findings suggest that it is both the dips in oxygen and the sleep segmentation that seem to predict change in this neural injury marker.”
Dr. Varga is exploring the significance of these findings further through a new study that is recruiting individuals ages 55 and older who have been newly diagnosed with sleep apnea. He will collect baseline measurements of the participants’ AD and neural injury biomarkers, administer PAP therapy, and measure biomarkers over a three-month treatment period to assess changes. Additionally, Dr. Varga will conduct high-field brain magnetic resonance imaging of the participants using a 7-Tesla brain MRI. This will enable him to resolve sleep-wake regulating centers in the brain and explore changes in functional connectivity in the brain as a result of treatment. That could yield more vital insights on the impact of PAP therapy on the biomarkers of AD and risk of developing the disease.
“Very few sleep scientists have really researched the impact of treatment with regard to sleep apnea,” Dr. Varga says. “Through our studies, we are filling that gap and our findings have the potential to improve long-term outcomes for patients with sleep apnea.”
From left: Korey Kam, PhD, Assistant Professor of Medicine; Saranya Ravi, MS, Research Coordinator; Andrew Varga, MD, PhD, Associate Professor of Medicine; Daphne Valencia, MA, Research Coordinator; Ankit Parekh, PhD, Assistant Professor of Medicine; Indu Ayappa, PhD, Professor of Medicine
Featured Faculty and Division Leadership

Andrew W. Varga, MD, PhD
Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)

Charles A. Powell, MD, MBA
Chief of Pulmonary, Critical Care and Sleep Medicine; Director, Mount Sinai Respiratory Institute