John F. Davis, age 75, is a production designer and storyboard artist with impressive film and television credentials. In 2018, the Yonkers, New York, resident was diagnosed with interstitial lung disease. But due to the intervention of Mount Sinai’s End-Stage Lung Disease and Transplant Program, Mr. Davis has been able to improve his quality of life.
Mr. Davis’s story began on September 11, 2001. At the time, he lived in a 38th-floor apartment just four blocks northwest of the World Trade Center. Over the following weeks, he watched trucks transport debris from Ground Zero to barges in the Hudson River, scattering dust with each trip. Mr. Davis thought little of it, even when air masks were handed out to residents. But years later, while undergoing routine imaging for hip replacement surgery, the impact of that dust was revealed: a black spot on his left lung.
Until that moment, Mr. Davis had not experienced any significant respiratory issues, other than asthma as a child. But in the weeks following the diagnosis, he experienced a rapid decline and increasingly curtailed his activities as he struggled to breathe. “My left lung was at 38 percent capacity,” he recalls. “My right one was at 48 percent. My doctor advised me to get on a lung transplant list as soon as possible so I would not die waiting for a replacement, but he was also implying that I would have a hard time getting one.”
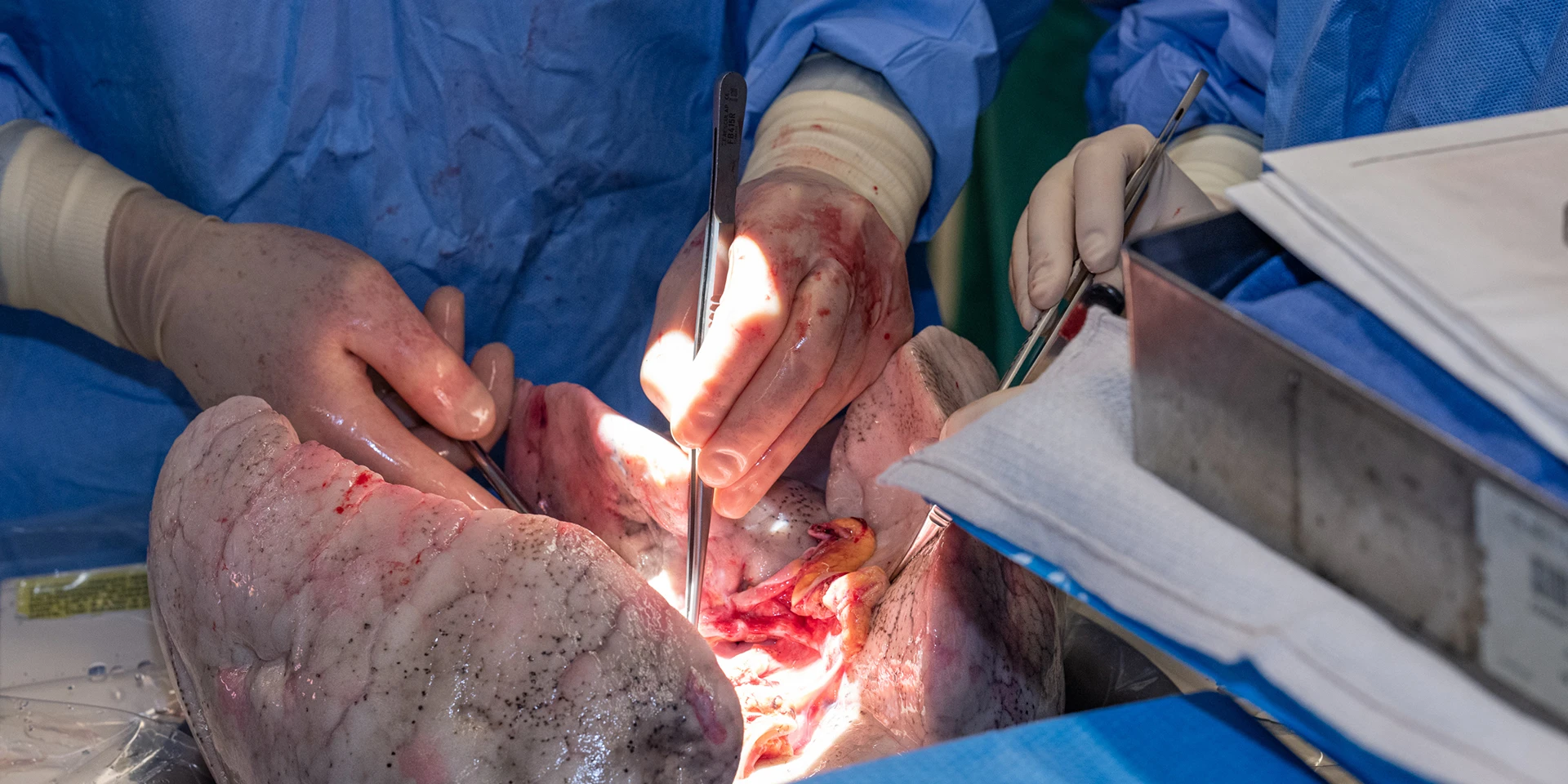
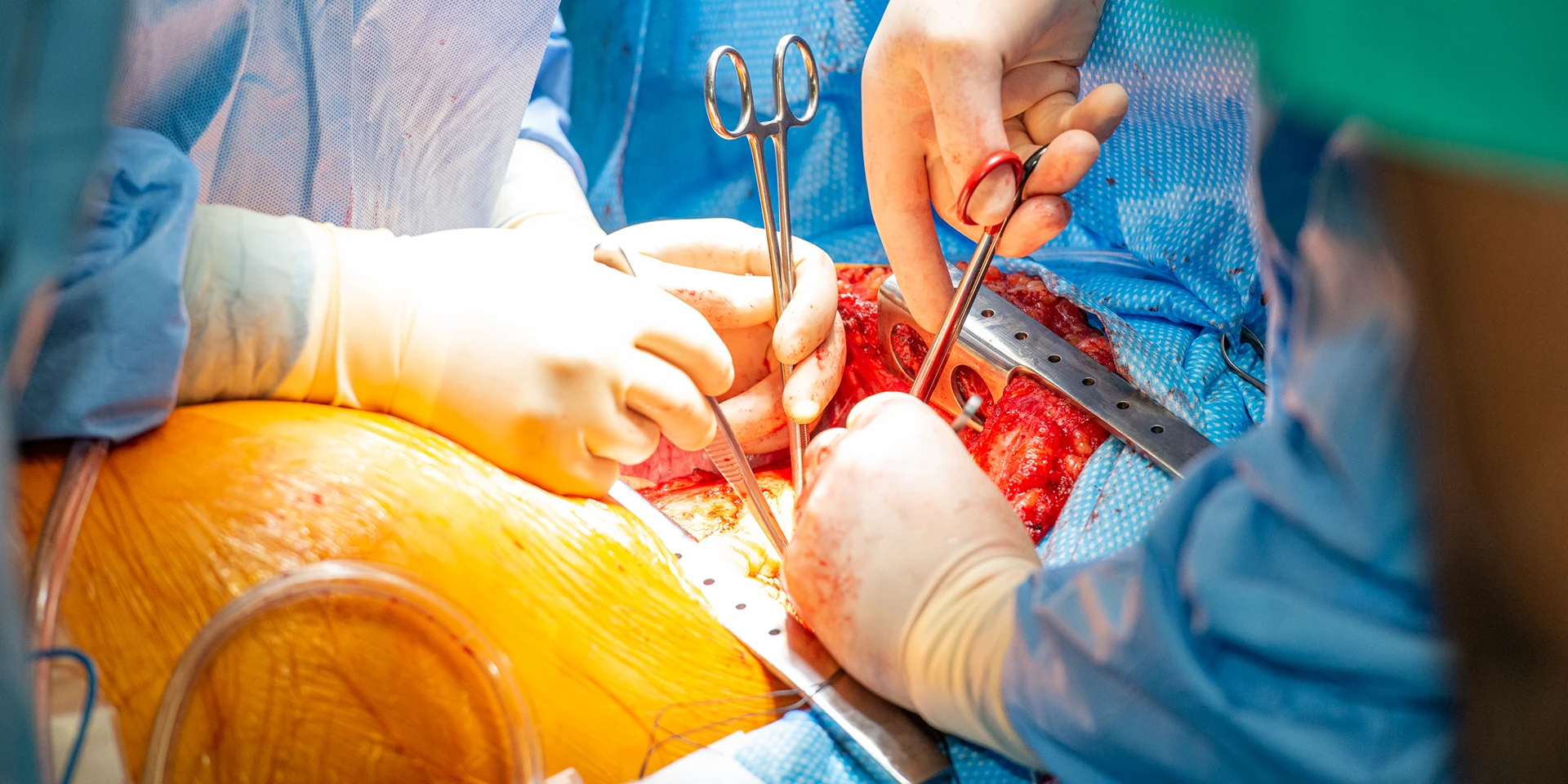
There were other concerns, as Mr. Davis had donated a kidney to his brother and has heart disease combined with his age and World Trade Center exposure, all factors that made him a high-risk candidate. Because of their extensive experience in treating such patients, Mount Sinai’s Scott Scheinin, MD, and Harish Seethamraju, MD, believed otherwise. For them, this was an opportunity to intervene and to help establish the End-Stage Lung Disease and Transplant Program as a leader in treating complex cases. On March 17, 2022, they proceeded with a five-hour left lung transplant procedure for Mr. Davis.
“We were meticulous in our approach in every aspect of this process. This includes the extensive pretransplant evaluation, the precise application of our surgical skills to minimize bleeding and complications, and finally the careful modulation of Mr. Davis’s immune suppression,” says Dr. Scheinin, Senior Faculty in Cardiovascular Surgery and Thoracic Surgery at the Icahn School of Medicine at Mount Sinai and Director of the Lung Transplantation Program for the Mount Sinai Health System. “We managed this case in a thoughtful and effective way and, as a result, this patient did remarkably well. In doing so, we demonstrated that we can achieve positive outcomes in complex cases that others would deem to be too high-risk.”
Mr. Davis was the second patient to undergo lung transplantation after the program’s launch in May 2021. The outcome is a testament to the more than three decades of excellence Drs. Scheinin and Seethamraju have achieved in caring for more than 1,000 lung transplantation patients. Their legacy continues at Mount Sinai Health System: As of December 2022, they had completed 14 transplantations, including six double lung transplants and eight single transplants.
Extensive expertise in surgical interventions also enables Drs. Scheinin and Seethamraju to offer patients alternatives to transplantation, such as lung volume reduction surgery, which eliminates the risks associated with immune suppression. Dr. Seethamraju describes the procedure as underutilized, in part because it is challenging to identify patients who are suitable candidates, such as those whose disease is localized in one area of the lung.
“Dr. Scheinin and I have the ability to make those determinations because we participated in the first clinical trial of this procedure in the United States,” says Dr. Seethamraju, Senior Faculty in Medicine (Pulmonary, Critical Care and Sleep Medicine) and Medical Director of the program. “There is an endobronchial approach to lung volume reduction that is less invasive. We are continually evaluating patients with severe emphysema and will tailor the appropriate procedure to the particular patient’s risk profile. Having all available treatment options provides us the ability to treat patients in a much more precise manner, rather than a one-size-fits-all approach.”
Drs. Scheinin and Seethamraju also have expertise in managing patients who have developed pulmonary graft-versus-host disease (GVHD) following bone marrow transplant. They have applied that knowledge to treat several Mount Sinai patients, successfully navigating them through the acute phase of their disease process.
“Immune suppression following a lung transplantation creates two significant risks for patients with GVHD,” Dr. Scheinin says. “One is the risk for recurrence of primary cancer, and the other is the risk of severe infection complications based on the amount and duration of immune suppression. We can manage the disease effectively among our patients through carefully developed steroid regimens without proceeding to surgery.”
Through research and clinical trials, Drs. Scheinin and Seethamraju are exploring other opportunities to reduce or eliminate the risks for those who do undergo surgery. Using patient-donated tissue from Mount Sinai’s BioMe™ Biobank, they are gaining new insights into lung disease and therapeutic agents that could provide safe, effective treatment. They are also developing an animal lung transplantation model to investigate chronic rejection in partnership with colleagues at National Jewish Health and Jefferson Health, and assessing the impact of disparities in the availability of donor organs on outcomes.
Drs. Scheinin and Seethamraju have also shown an ability to achieve positive outcomes in the face of the COVID-19 pandemic. Their first transplantation case at Mount Sinai, a double lung transplantation performed on "Iron Chef" winner and Ground Zero volunteer James Kelly, involved a donor who tested positive for the Omicron variant of SARS-CoV-2—a factor that would automatically disqualify the donor at many centers, according to Dr. Seethamraju.
“Because Dr. Scheinin and I managed so many COVID-19 cases during the pandemic, we were very well aware of its ramifications,” says Dr. Seethamraju. “We conducted a computed tomography scan and a bronchoscopy bronchoalveolar lavage with a polymerase chain reaction test, which we then repeated. Based on what we observed, we believed the donor’s COVID-19-related infection was likely confined to the upper airway, creating a window of opportunity to use the donor’s lungs.”
Mr. Kelly was closely monitored and showed no signs of SARS-CoV-2 infection or rejection of the new lungs. (View this video of Mr. Kelly's story.)
As for Mr. Davis, in the months since he underwent surgery, his story has changed from one of struggling to breathe and inactivity to one in which he takes long walks through Central Park with his wife, June Bateman.
“There was a time when John was so sick that he would find a bench and just sit there,” says Ms. Bateman. “Now he is averaging 7,000 steps per day, thanks to Drs. Scheinin and Seethamraju. The whole Mount Sinai team was consistently attentive, gracious, and professional, and that made all the difference.”

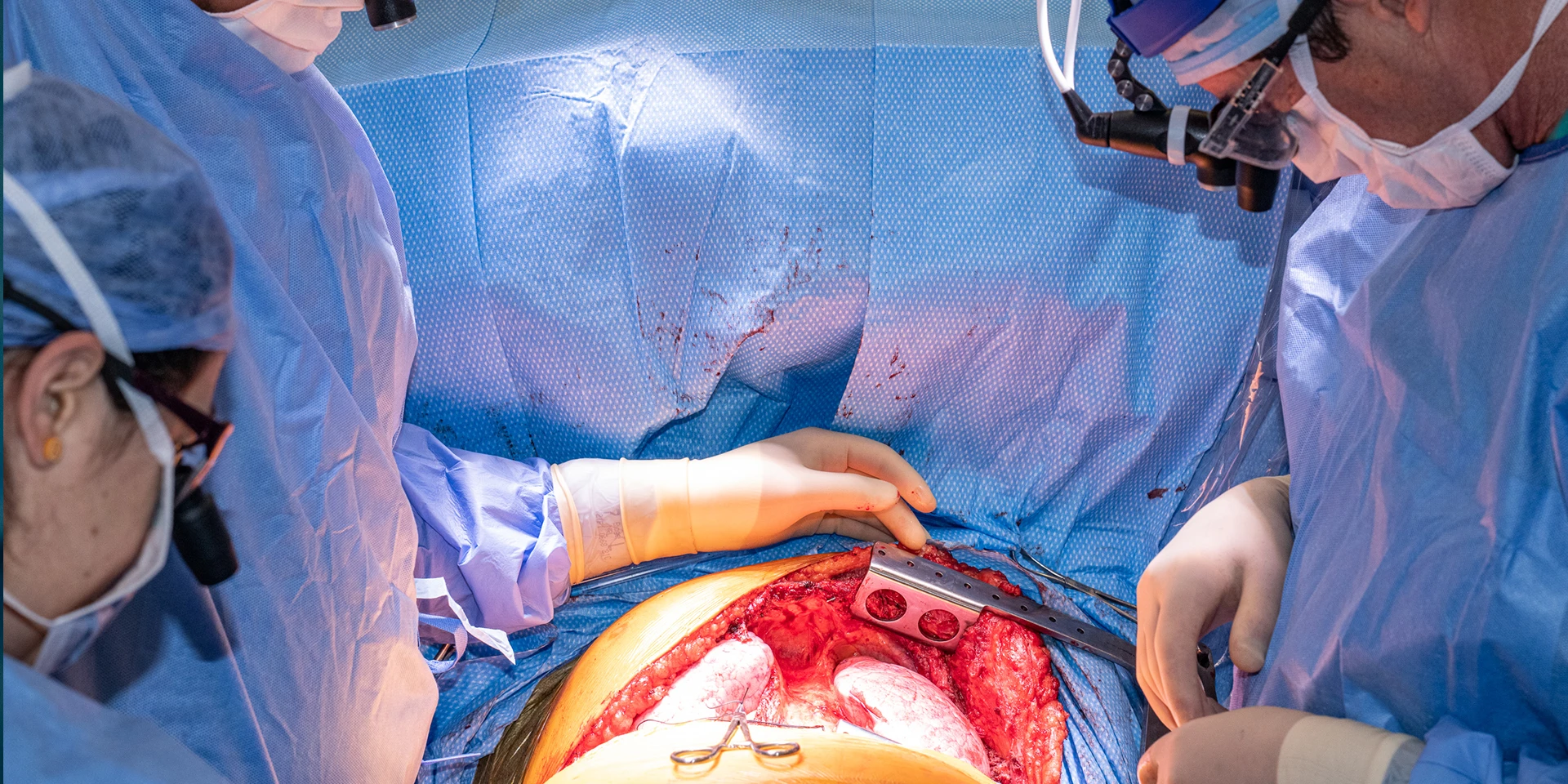
John F. Davis, who was diagnosed with interstitial lung disease after the September 11 attacks, received a lung transplant at The Mount Sinai Hospital.

Mr. Davis, center, with the transplant team, from left: Rozelle Dukette, FNP-BC, Harish Seethamraju, MD, Scott Scheinin, MD, Brian Housman, MD