Related Article
Despite significant progress in therapeutic approaches over the past decade, an estimated 5 percent to 10 percent of patients with severe asthma are not well served by current therapies. Part of the problem, according to Linda Rogers, MD, is that researchers have traditionally approached asthma as a single disease.
“When we look at patients whose asthma is not controlled by existing therapies, we find that they are very heterogenous in terms of disease drivers,” says Dr. Rogers, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), Icahn School of Medicine at Mount Sinai; Clinical Director, Adult Asthma Program, Mount Sinai – National Jewish Health Respiratory Institute; and Clinical Director, Medicine Clinical Trials Office.
“Some of the therapies we administer do not necessarily treat the type of inflammation they have, or their inflammation might be better controlled by other treatments—such as ones used to treat other diseases—based on disease mechanisms research we have done. Thus, we are interested in the potential of a precision medicine approach to treating these patients.”
Dr. Rogers is playing a key role in one of several initiatives at Mount Sinai to better understand the factors that contribute to severe asthma and identify new treatments. She is the site Principal Investigator for the Precision Interventions for Severe and/or Exacerbation-Prone Asthma (PrecISE) Network Study, funded by the National Heart, Lung, and Blood Institute. This study was designed with input from Monica Kraft, MD, while she was at the University of Arizona; Dr. Kraft is now the Murray M. Rosenberg Professor of Medicine, and Chair of the Department of Medicine, at Mount Sinai Health System and Icahn Mount Sinai.
Through this study, more than 30 centers nationwide are working on developing precision medicine approaches to the treatment of severe asthma. That includes investigating the possibility of using biomarkers and other patient factors to inform patient treatment.
“Although biomarkers such as blood eosinophil counts and exhaled nitric oxide levels have been used in the clinical setting to assess patient eligibility for certain advanced therapeutics, this study is collecting samples such as sputum, nasal brushings, and exhaled breath condensate to better understand the disease and identify more biomarkers and targets for therapy,” Dr. Rogers says. “We are also collecting genetic data and using that to select novel targeted therapies that are not currently used in clinical practices.”
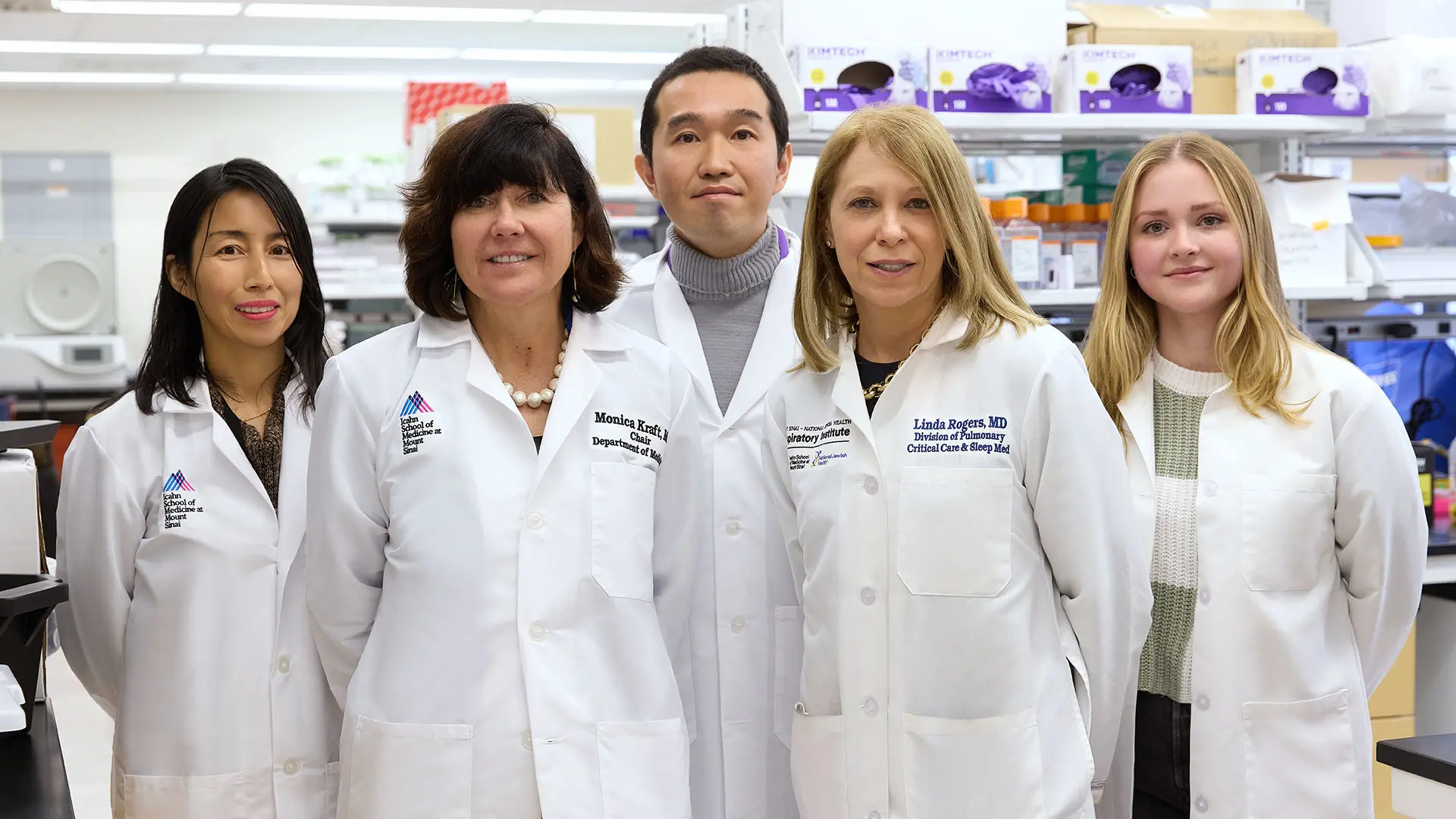
From left: Naoko Kimura, MD; Monica Kraft, MD; Hiroki Kimura, MD, PhD; Linda Rogers, MD; Allyson Molzahn, Associate Researcher
The study is unique in that it is using an adaptive protocol to assess the efficacy of five therapeutic agents—imatinib mesylate, Broncho-Vaxom®, clazakizumab, medium chain triglycerides, and cavosonstat—among 600 participants who have severe asthma with symptoms that are not well controlled through high-dose inhaled corticosteroids and other therapies. These therapeutic agents were proposed by participating centers based on preliminary data from mechanistic, animal, and other studies suggesting efficacy. Each participant will be administered one of these agents, or a placebo, for a period and, following a washout, will be eligible to receive up to four additional therapies over the course of the study.
“Adaptive platform studies have been used in both COVID-19 and cancer clinical trials but to our knowledge this is one of the first times this protocol has been used to develop precision medicine therapeutics for asthma,” Dr. Rogers says. “It will enable us to conduct a series of five parallel phase 2 studies to assess asthma treatments that are promising but that are not under commercial development for an asthma indication. If we determine one agent is unsuccessful based on statistical analysis, we can abandon it to explore the efficacy of another agent, which accelerates the drug development process.”
As Dr. Rogers evaluates a precision medicine approach to treat severe asthma, Sonali Bose, MD, MPH, is investigating the impact of environmental and nutritional factors on asthma control among a cohort of 30 pregnant individuals. Her goal is to identify opportunities to improve health outcomes among pregnant patients and potentially reduce the intergenerational risk of respiratory disease in their children.
“Asthma is the most common respiratory disease in pregnancy and can have a significant impact on both the health of mom and baby. Poor asthma control during pregnancy has been associated with many complications of pregnancy and a higher risk of respiratory disease in the offspring. Since asthma control can be dynamic during pregnancy, it is important to capture asthma health throughout gestation in a way that will allow us to intervene in a timely manner,” says Dr. Bose, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Pediatrics, at Icahn Mount Sinai.
“We want to gain a better understanding of the determinants of asthma control during pregnancy, particularly among urban Black and Hispanic populations, who have a disproportionate risk for asthma morbidity and traditionally have the highest rates of pregnancy complications as well.”

From left: Nicholas Brereton, clinical research coordinator; Sonali Bose, MD, MPH; Rachel Meislin, MD, fellow; Zhi-Yuan Wang, MD, clinical research coordinator
Dr. Bose is conducting two pilot studies among this cohort. One, building on her prior work on the influence of indoor exposures on asthma in other populations, focuses on the impact of indoor air pollution, specifically indoor fine particulate matter exposure, on asthma during pregnancy among 20 participants. Each trimester, Dr. Bose and her research team are collecting one week of data from two air monitors—a traditional model that captures particulate matter in real time and a PurpleAir sensor, a low-touch commercially available monitor. Simultaneously, her team is performing daily home spirometry tests and capturing home activities, asthma symptoms, and medication use. The one-week data collection duration was chosen to maximize resources for the study.
The second study assesses whether a higher omega-3 status is associated with improved asthma control during pregnancy among 30 participants—15 recruited from her cohort and 15 from Duke University. The team is rigorously collecting nutritional intake data as well as measuring blood omega levels repeatedly during each trimester of pregnancy. Previous studies have demonstrated that omega-3 polyunsaturated fatty acids (PUFAs) have an anti-inflammatory influence, which could have therapeutic value among patients with asthma. The team is specifically interested in whether downstream metabolites of PUFAs called specialized pro-resolving mediators help combat the inflammation associated with asthma.
Dr. Bose is particularly interested in exploring that protective aspect at an individual level among pregnant people and is collaborating with the Mount Sinai Maternal Fetal Medicine division, as well as researchers at the University of Nebraska, University of Colorado, and Duke University, to complete this work.
In addition to a better understanding of risk factors that influence the asthma health of the mother and its likely implications for the fetus, data gleaned from these studies will enable Dr. Bose to design larger follow-up studies that assess the efficacy of interventions such as reduction of indoor air pollution or increased omega-3 intake.
“Poor asthma control during pregnancy has been linked to consequences such as spontaneous premature birth, gestational hypertension, and gestational diabetes,” Dr. Bose says. “Through our work, we can gain more knowledge about upstream factors that impact asthma control and thus help improve maternal and fetal health.”
Dr. Bose's research is supported by a Mount Sinai Transdisciplinary Center on Early Environmental Exposures Pilot Research (P30) grant (grant number P30ES023515) and the American Lung Association Airways Clinical Research Center (ALA-ACRC) pilot award.
Watch a video about Dr. Rogers's work.
Featured Faculty and Division Leadership
Linda Rogers, MD
Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)

Monica Kraft, MD
Murray M. Rosenberg Professor of Medicine; Chair of the Department of Medicine

Sonali Bose, MD, MPH
Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Pediatrics

Charles A. Powell, MD, MBA
Chief of Pulmonary, Critical Care and Sleep Medicine; Director, Mount Sinai Respiratory Institute