Over the past 20 years, Javier Zulueta, MD, has seen more patients present with late-stage lung cancers than he can count. It is a legacy that haunts him because he knows those patients could have benefited from early intervention and treatment if they had participated in a lung cancer screening program.
But fewer than 10 percent of potential candidates undergo screening for myriad reasons, such as fear of what screening might reveal, debates about the merits of screenings, the Medicare-mandated shared decision-making consultation, and the use of negative or outdated consultation tools that are not designed to address concerns such as the potential harm of overdiagnosis and false positives.
“If you look at the data from the Early Lung Cancer Action Program, you will see that eight out of 10 patients with cancer detected through screening get cured with surgery,” says Dr. Zulueta, Professor and Chief of Pulmonary, Critical Care and Sleep Medicine at Mount Sinai Morningside. “We need to get the correct information out to physicians and patients that lung cancer screening works and that it is more efficient than breast cancer screening. The number of patients who need to undergo lung cancer screening to save one life is less than 500. For breast cancer, it is more than 1,000.”
[Related: a new Mount Sinai study supports the value of increased screening.]
For Dr. Zulueta, the goals are clear: expand existing screening criteria, engage physicians and candidates, and position Mount Sinai Morningside as a screening hub that catches cancers early and achieves positive outcomes in West Harlem, a community that is home to an underserved population with a high incidence of lung cancer.
< 10
percent of potential candidates undergo lung cancer screening
8 of 10
patients with cancer detected through screening get cured with surgery
Age and smoking history are the key factors now used to identify high-risk individuals who should undergo annual low-dose computed tomography (CT) lung cancer screening, and Dr. Zulueta says there is compelling evidence for changing that. A 2015 study he coauthored found that the United States Preventive Services Task Force’s screening criteria miss up to 40 percent of cancers. He believes factors such as chronic obstructive pulmonary disease and emphysema—which was found to be a powerful biomarker of the risk of lung cancer in a previous study by his group in 2006—should be considered, and he is conducting further research that he hopes will bear that out.
Dr. Zulueta is also expanding the International Early Lung Cancer Action Program to Mount Sinai Morningside, making it a hub of the program. For years, the program has provided interpretation and recommendations for patients who have undergone low-dose CT scans conducted at Mount Sinai Morningside. The newly expanded program will further harness the extensive expertise of Mount Sinai Morningside’s clinical specialists in treating critically ill pulmonary patients.
“The opportunity to apply my previous experience in growing an academic division and do it for a world-leading health care system is what drew me here,” says Dr. Zulueta, who led the expansion of the Pulmonary Service division at the Clínica Universidad de Navarra in Pamplona, Spain. “I want to expand the division to include clinical research and to incorporate lung cancer as an important reference.”
Since joining Mount Sinai Morningside in April 2021, Dr. Zulueta has launched a new lung nodule program with a dedicated multidisciplinary team of experts who will oversee screening and follow all nodules. This program will also run an incidental lung nodule program, which will focus on the diagnosis and monitoring of nodules that have been identified in patients who have undergone CT scans for conditions such as chest pain, coronary disease, or a pulmonary embolism. It is an ambitious undertaking, given that an estimated 1.5 million to 2 million incidental nodules are identified each year.
Examples of incidental nodules
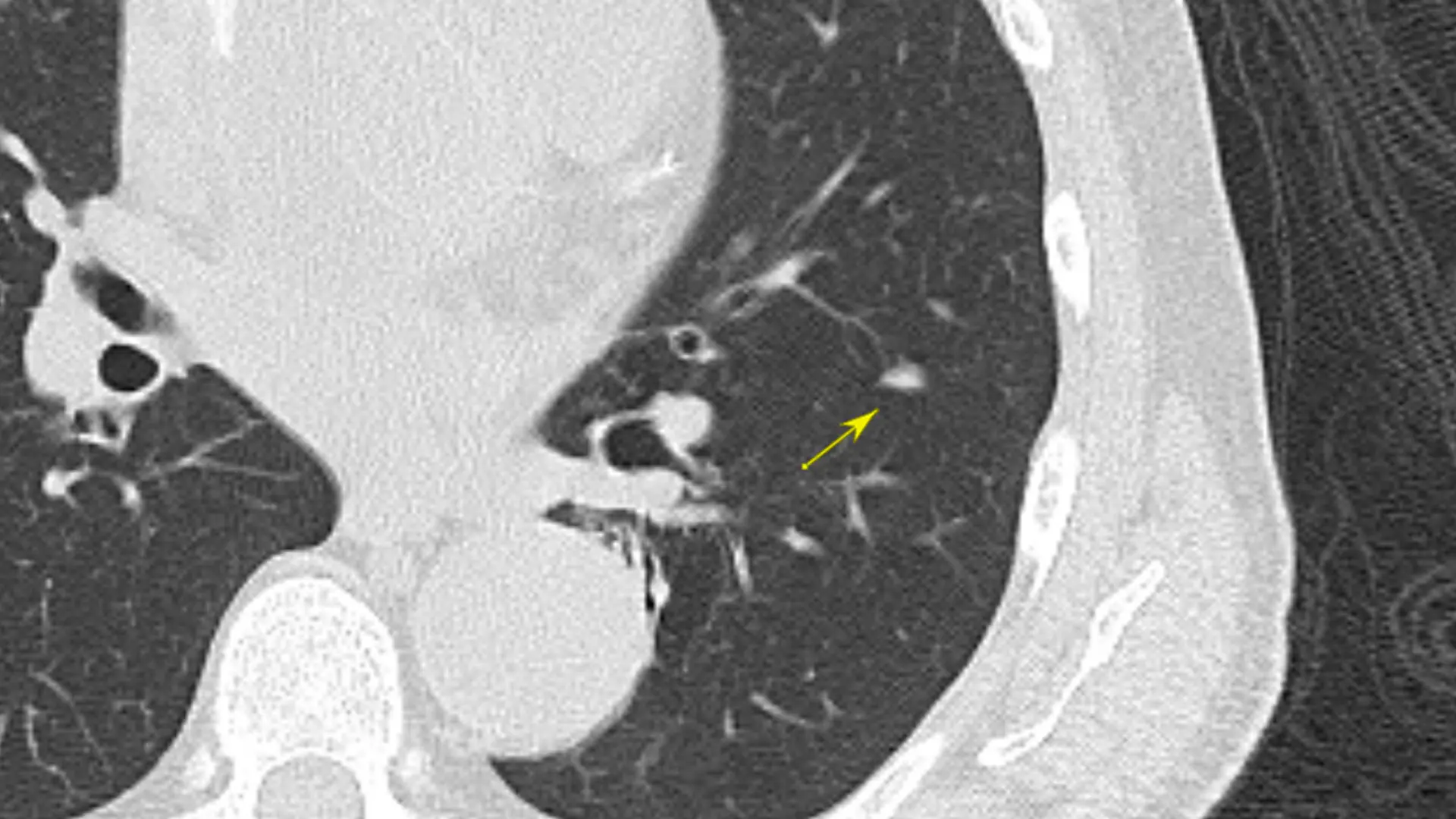
Triangular solid nodule: most likely a lymph node. The triangular shape and the location in the major fissure are characteristic of benign nodules.
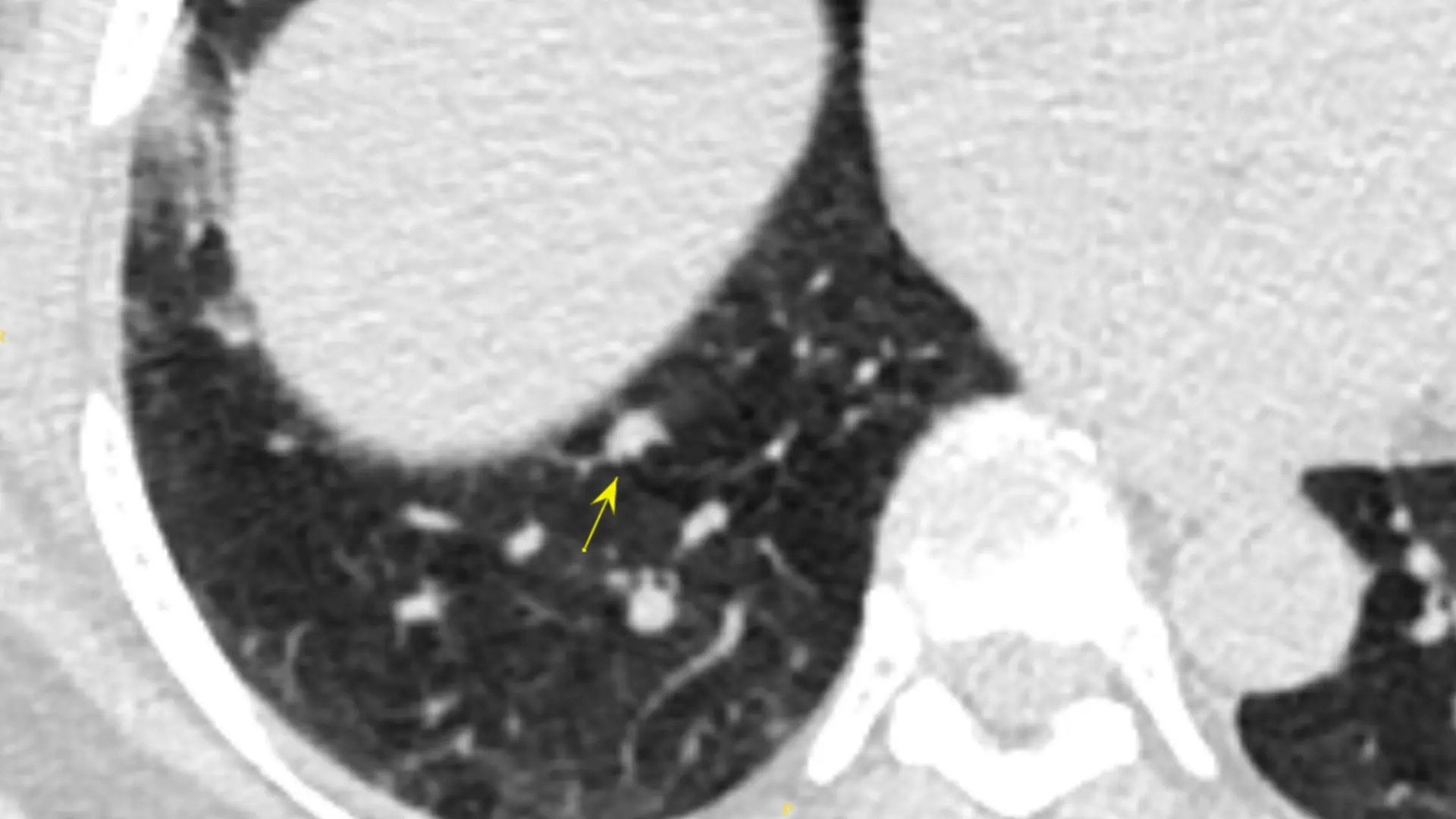
Solid nodule 8x6 mm: also needs follow-up in 6-12 months according to the guidelines.
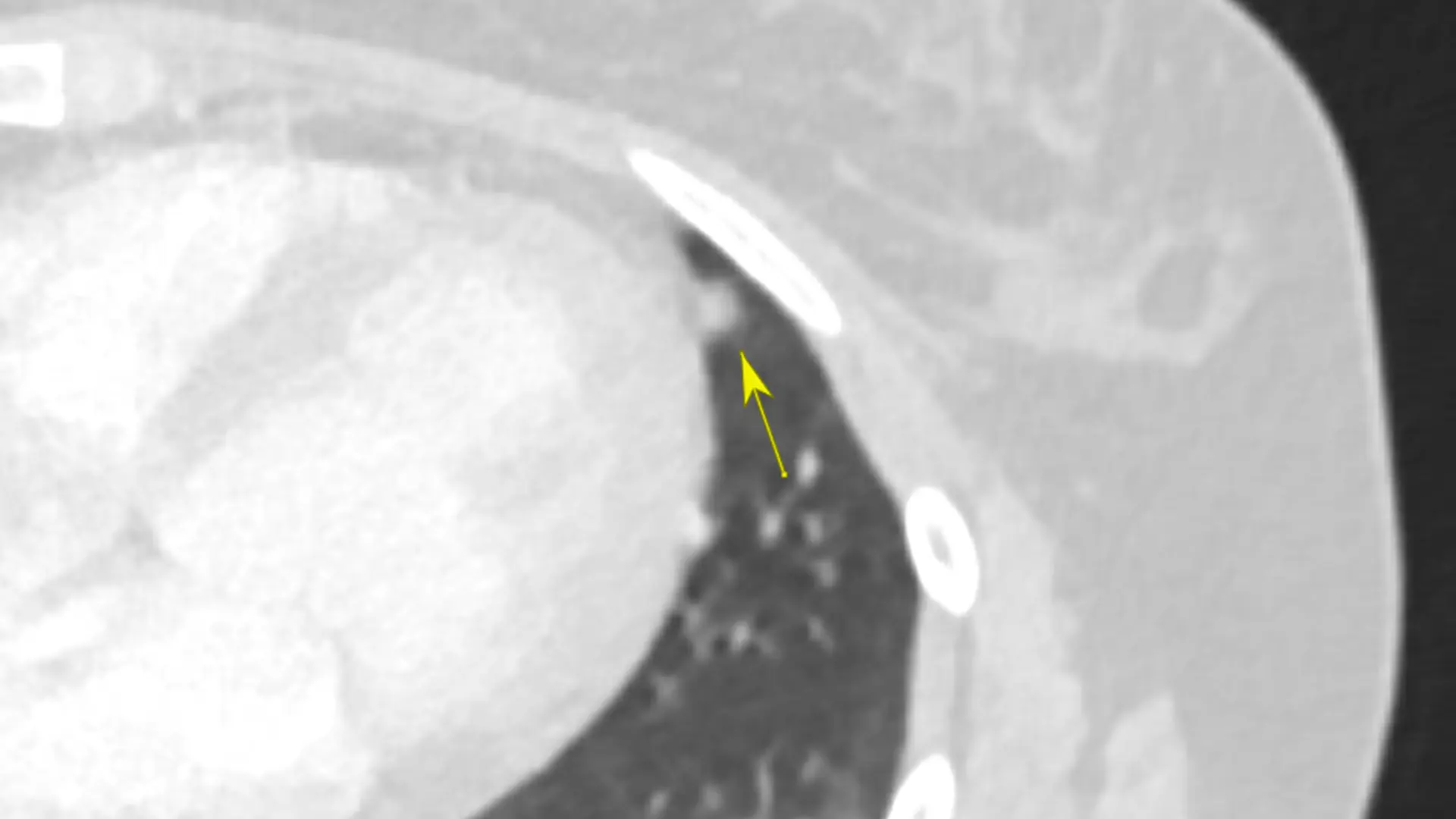
Solid nodule lingual 5 mm: according to Fleischner guidelines, in high-risk people this requires a follow-up in 12 months with a new CT.
“The complexity involved in managing incidental nodules is such that up to 60 percent are not worked up despite the fact that a significant percentage of them will end up being cancer,” Dr. Zulueta says. “My experience in lung cancer screening and in assessing the very small nodules detected during screening provides an opportunity for Mount Sinai Morningside to expand into this field of incidental findings. I believe this program will feed the lung cancer screening program in a very significant way.”
To ensure that no incidental nodules are overlooked, Dr. Zulueta is also exploring the potential of implementing software that uses natural language processing to flag CT scans that have detected nodules. The goal, he notes, is not to reevaluate CT scans that have been reviewed by radiologists but to ensure that the reports containing those findings do not fall through the cracks once they circulate beyond radiology. “Our multidisciplinary group will look at the reports, classify the patients based on risk for lung cancer, and then ensure that their primary care providers are aware of the findings and recommendations and follow guidelines,” he says.
As Mount Sinai Morningside’s expanded lung cancer screening program takes shape, Dr. Zulueta is engaging in outreach with primary care providers and the community alike to increase awareness of and interest in screening. Those efforts, which will include in-person educational meetings, have been hampered to some extent by the COVID-19 pandemic, but primary care practices have been receptive to the new program. “The success of screening is highly dependent on getting the word out,” he says. “Underserved areas nationwide, including the community we serve, have lower screening rates than the national average, and I believe that is due to lack of information. That is why community education and outreach will be a major component of our efforts. The more we get the word out about the importance of screening, the more we can engage the patients who are at risk.”
Success for Dr. Zulueta will be an average of 10 patients screened per week by the end of his first year, a significant growth from the one patient screened per week that Mount Sinai Morningside has averaged over the past four years. Ideally, he would like to see two to three times that number screened, which would help to reduce the number of New York City residents, now estimated at 3,000, who die each year due to lung cancer. This growth would also facilitate the development of more robust thoracic surgery and lung oncology programs at Mount Sinai Morningside, and the pursuit of research opportunities that could lead to new diagnostic and treatment targets such as blood biomarkers. Eventually, his plan is to expand the lung cancer screening program to be a thoracic health program that will help reduce the three most common causes of death—chronic obstructive pulmonary disease, coronary artery disease, and lung cancer.
"It is going to take consensus among several specialties to reach that point, but I believe we are going to see screening change significantly over the next three to five years,” Dr. Zulueta says. “I want Mount Sinai Morningside to be at the forefront of that effort.”
Featured

Javier Zulueta, MD
Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)
