Expecting mothers often take a wide range of medications for various purposes, but it is not clear whether those drugs have any associated risk for offspring autism spectrum disorder (ASD). Mount Sinai researchers have teamed up with other institutions to explore these links.
The first-of-its-kind study, published online in European Psychiatry in August 2025, uses a unique methodology that combines classic pharmacoepidemiology with computational pharmacology, says Abraham Reichenberg, PhD, Professor of Psychiatry, and Environmental Medicine at the Icahn School of Medicine at Mount Sinai, and joint senior author of the paper.
“By combining epidemiology, pharmacological sciences, and bioinformatics, we were trying to obtain more reliable insights to medications that may be associated with a higher, or lower, risk than we could before,” says Dr. Reichenberg.

Abraham Reichenberg, PhD, Professor of Psychiatry, and Environmental Medicine at the Icahn School of Medicine at Mount Sinai (right), and Shlomit Beker, PhD, Assistant Professor of Psychiatry (left), are part of the Seaver Autism Center for Research and Treatment, which works to unravel the various causes of the disorder. Using a unique methodology that combines classic pharmacoepidemiology with computational pharmacology, Dr. Reichenberg and a team of researchers are exploring links of medications that expecting mothers take with offspring autism risk.
The other key authors of the paper include Avner Schlessinger, PhD, Professor of Pharmacological Sciences at the Icahn School; Magdalena Janecka, PhD, Associate Professor of Child and Adolescent Psychiatry, and Population Health at NYU Langone Health, New York City; and Stephen Levine, PhD, Professor of Social Welfare and Public Sciences, University of Haifa, Israel.
The team of researchers identified two prescription drugs that could be associated with increased ASD risk following prenatal exposure and one that could be associated with a decreased risk. They also identified the associated pharmacological targets of the drugs, gaining insight into the biological plausibility of the relation to ASD.
A Challenging Study
Testing medications that expecting mothers might take while pregnant is difficult due to ethical concerns about their impact on the development of the fetus, says Dr. Reichenberg.
“It is also challenging, but very important, to untangle confounding by indication. We decided to take a multidisciplinary, prescription-wide approach to exploring these associations to see what we could find,” he says.
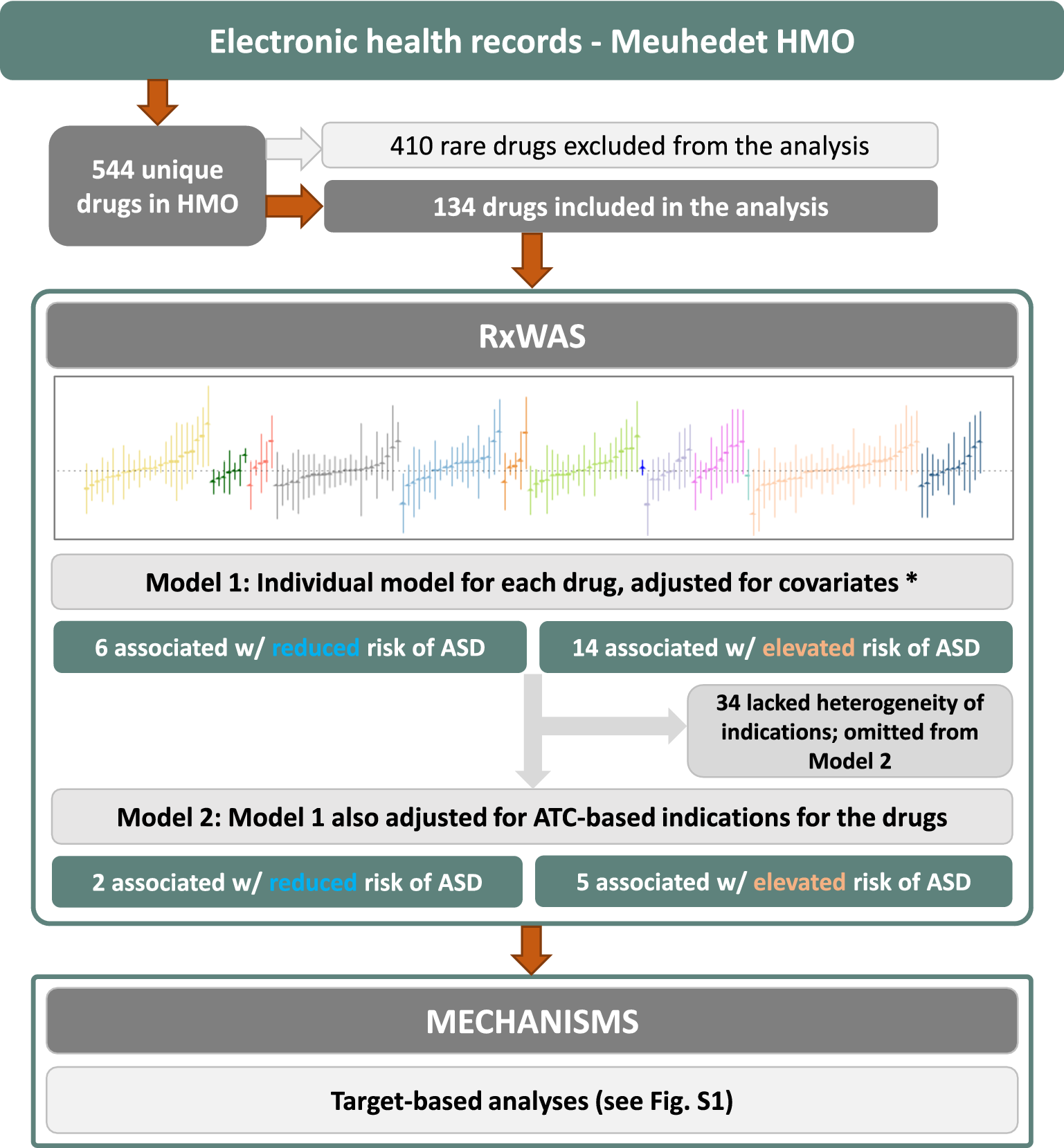
The study looked at 1,400 individuals with and 94,713 without an autism spectrum disorder diagnosis from the Meuhedet health maintenance organization in Israel. Researchers then assessed 134 medications against the study group, using regression models that adjusted for factors such as birth year, maternal age, child sex, and health care utilization.
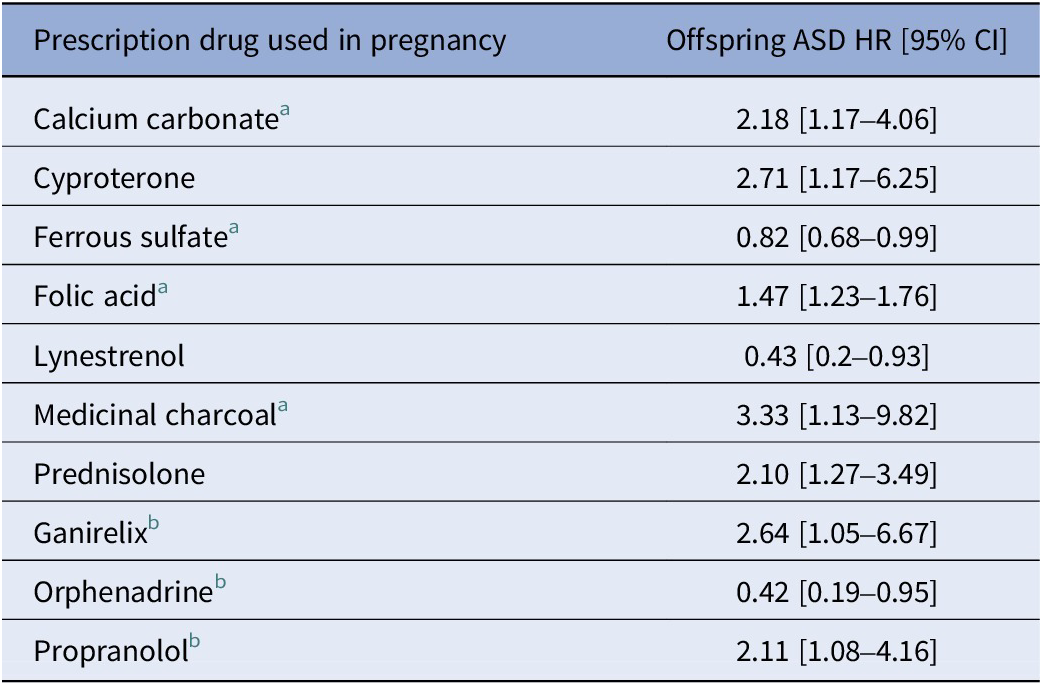
The strongest indication-adjusted associations in the analysis included the following: medicinal charcoal (HR=3.33, 95% CI=1.13–9.82), cyproterone (HR=2.71, 95% CI=1.17–6.25), and prednisolone (HR=2.10, 95% CI=1.27–3.49). However, Dr. Reichenberg cautions against drawing any further conclusions about these medications causing autism risk based on these associations, and more studies, replication, and validation with larger and more diverse sample sizes are needed to confirm any findings.
The study used a case-cohort sample from the Meuhedet health maintenance organization (HMO) in Israel drawn from people born between 1998 and 2008. The sample consisted of 1,400 individuals with an ASD diagnosis and 94,713 individuals without.
“We were fortunate to be able to examine the range of medications. We did not have to specify a priori which medications we would test,” explains Dr. Reichenberg.
That unfettered access enabled the researchers to look at exposure to all drugs received during the 12 months before childbirth, which encompassed medications and supplements with an anatomical therapeutic chemical (ATC) code included in the HMO’s prescription register.
Finding Links, Or Lack Thereof
Of the 544 unique prescribed drugs identified in the database, the team excluded 410 from their prescription-wide association analysis because of infrequent use. For the remaining 134 medications, the researchers applied regression models that adjusted for factors such as birth year, maternal age, child sex, and health care utilization. They then used the same models to also adjust for indication (using level 2 ATC codes).
The researchers identified two prescribed drugs that were statistically significantly associated with increased risk for offspring ASD, one associated with a decreased risk and showed no evidence for confounding by indication. These included cyproterone (an antiandrogen, HR=2.71), prednisolone (a corticosteroid, HR=2.10), and lynestrenol (a progestogen, HR=0.43).
The researchers then analyzed the pharmacological targets of the drugs to identify potential mechanisms for the associations. They identified 22 targets, four of which were statistically significantly associated with offspring ASD risk. These were: butyrylcholinesterase (HR=2.04), carbonic anhydrase IX (HR=1.81), neuronal acetylcholine receptor, alpha4/beta4 (HR=1.45), and serotonin-2b receptor (HR=1.31). These findings were subsequently corroborated through pathway analysis.

Some members of the Seaver Autism Center, from left to right: Dr. Reichenberg; Danielle Halpern, PsyD, Associate Professor of Psychiatry; Alex Kolevzon, MD, Clinical Director of the Center; Audrey Rouhandeh, PhD, Clinical Research Coordinator; Paige Siper, PhD, Assistant Professor of Psychiatry; and Tess Levy, MSc, Assistant Professor of Psychiatry.
“The novel aspect of this approach was that we identified mechanisms that could be linked to the underlying biology of autism,” Dr. Reichenberg says.
Dr. Reichenberg cautions that further replication and validation in independent samples are required to confirm the associations observed in this study. He and his colleagues have received funding to study larger samples, and they plan to repeat the analyses to see if the results are similar across different samples and populations.
“For physicians and those who are pregnant, the most important thing to know is most of the medications we were able to study had no association with a risk for autisms” says Dr. Reichenberg.
“We are also interested in using similar methods to look at broader questions about the impact of medications on pregnancy and offspring,” he adds. “The hope is we will see consistency in results and be able to provide more information to the public on medications that could increase or decrease risk for neurodevelopmental disorders.”
Featured

Abraham Reichenberg, PhD
Professor of Psychiatry, and Environmental Medicine at the Icahn School of Medicine at Mount Sinai
