The placebo effect—a phenomenon where one’s condition shows improvement simply from the belief of having received treatment—is a well-known example of belief affecting neurobiology. But much of the actual mechanisms underlying those interactions remain unknown. A first-of-its-kind study from a team of Mount Sinai researchers has shown that human beliefs can alter brain activities and behavior in ways that are similar to the effects of pharmacological agents.
The study, published in nature mental health in January 2024, explored whether beliefs about nicotine could induce dose-dependent responses in the human brain.
“Findings from the study could be crucial for advancing our knowledge about the role of beliefs in addiction as well as a broad range of disorders and their treatments,” says Xiaosi Gu, PhD, Associate Professor of Psychiatry, and Neuroscience, at the Icahn School of Medicine at Mount Sinai, and Director of Center for Computational Psychiatry at Mount Sinai.

The study that Xiaosi Gu, PhD, is conducting advances our knowledge about the role of beliefs in addiction, which opens the doors to new ways of looking and treating various substance-use disorders.
Links between nicotine beliefs and thalamus activity
In the randomized, double-blind study, the research team conducted neural activity imaging on 20 nicotine-dependent participants, who underwent three identical experimental sessions.
Each participant was asked to vape an electronic cigarette that they were told had either a low, medium, or high level of nicotine, despite the levels being consistent throughout the study. Participants were asked to rate their perceived nicotine strength using a ten-point scale.
The team chose nicotine for the study because it is a potent neuroactive substance that is also subjective to modulation by cognitive factors. It is also known to affect the thalamus and the striatum, which are important for cognition and decision-making.
After vaping, each participant performed a functional magnetic resonance imaging (fMRI) decision-making task specifically chosen to engage the neural circuits affected by nicotine. In the task, participants made sequential investment choices in simulated stock markets based on their prediction of market return. A cohort of 31 non-smoking healthy controls also performed this task without vaping.
Participants who were told they had a higher-strength electronic cigarette reported perceived their electronic cigarette to be stronger, supporting the premise that belief can be manipulated by instruction.
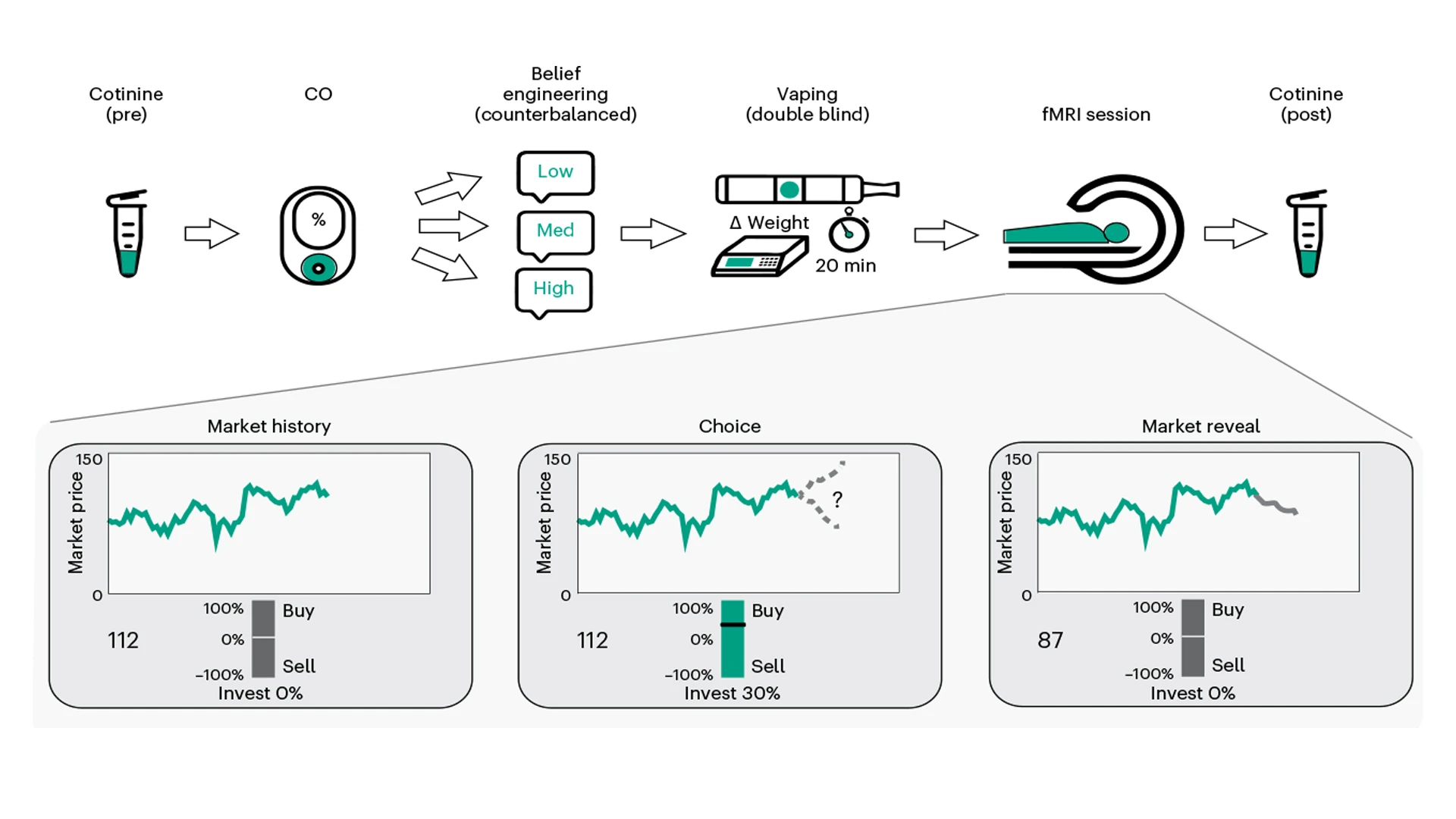
In the schematic showing the study protocol, researchers collected saliva samples for cotinine measurement and assessed exhaled carbon monoxide (CO) levels. They then told participants about the nicotine strength of their vape to influence their beliefs, and had them vape the e-cigarette. Researchers then measured the participants' brain activities using fMRI as they engaged in a decision-making task and collected a second saliva sample post-scan.
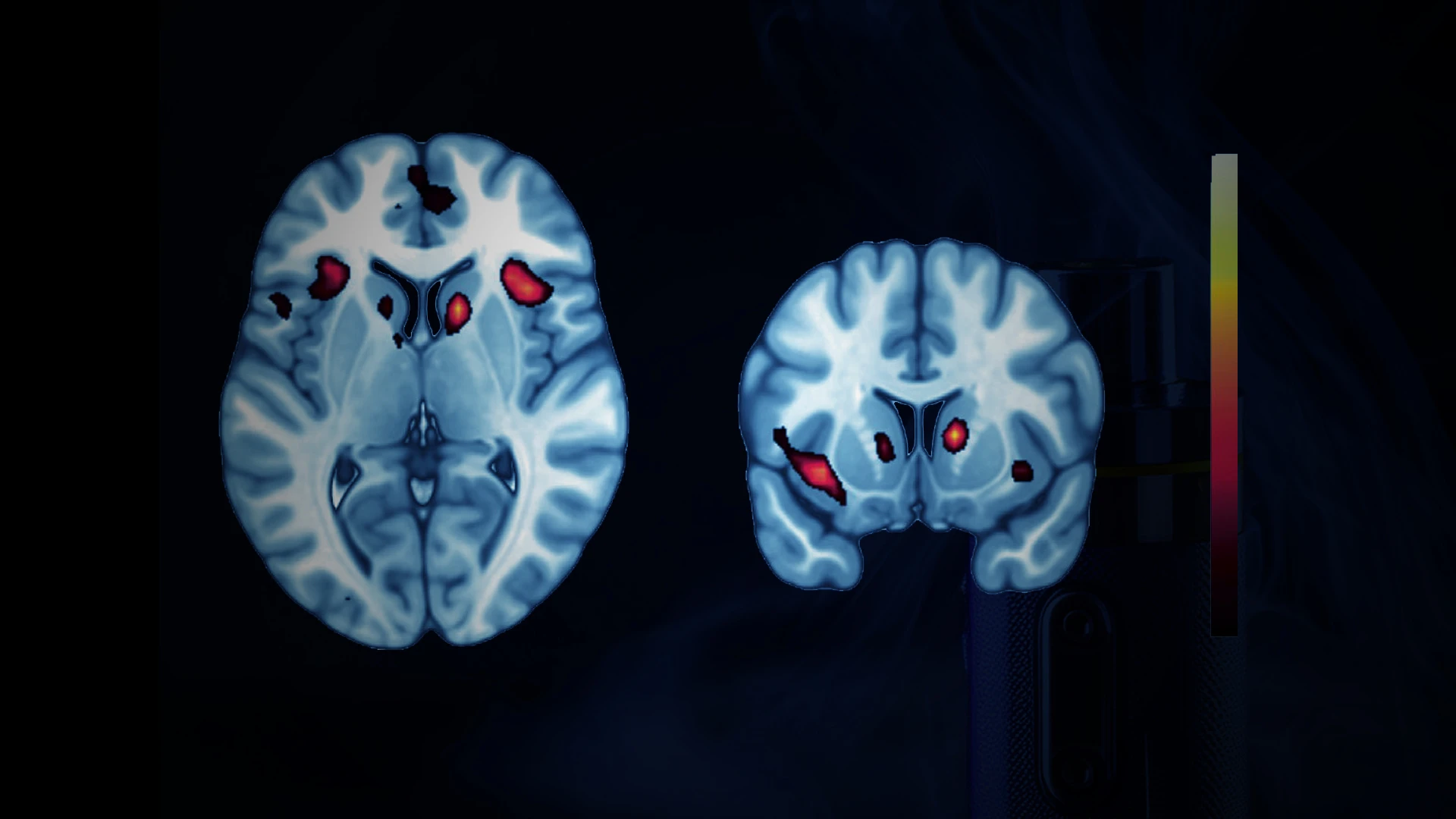
Imaging revealed that stronger beliefs about nicotine levels resulted in correspondingly higher neural activity in the thalamus but not in other brain regions, such as the striatum. This confirms that subjective beliefs, which were shaped by instructions about nicotine dosage, also induced dose responses in the thalamus. Taken together, these results pinpoint the thalamus, particularly the posterior thalamus, as a key neural substrate representing nicotine-related beliefs.
The findings were surprising, as although the thalamus contains the highest concentration of nicotine receptors in the human brain and is an initial binding site for the stimulant, it is considered a low-level region in the hierarchy of brain regions affected by nicotine. There is no direct evidence that participant belief affected nicotine binding, but the possibility could be explored in future studies using other imaging techniques.
“Our findings provide a mechanistic explanation for the well-known variations in individual responses to drugs and suggest that subjective beliefs could be a direct target for the treatment of substance use disorders,” Dr. Gu says.
Based on these findings, Dr. Gu says beliefs can be traced through brain activity much like more tangible stimuli, such as images and sound, despite a lack of understanding of where they are stored, or which part of the brain is involved in processing beliefs. The study also provide empirical evidence as to how the brain perceives the world, even in the case of a potent drug like nicotine.

The heat map (left) on the effects of instructed beliefs on participants, demonstrating the link between the thalamus and the ventromedial prefrontal cortex (vmPFC). As functional coupling strength between the thalamus and vmPFC of smoking participants and nonsmoking controls were plotted out (right), there was a statistically significant difference between groups, especially comparing those who were told they were given high-dose e-cigarettes and the controls.
Such findings, Dr. Gu adds, open avenues for exploration that could be transformative for patients who present with substance use and mental health conditions that have proven resistant to biological interventions.
For example, it is possible to gain more insights on the efficacy of cognitive interventions such as psychotherapy among patients, Dr. Gu points out. There is also the potential to better understand the variance in responses among patients to therapeutic agents and mental health treatment, and to harness drug-related beliefs to improve impacts and outcomes.
The goal now is to explore the effects of patient beliefs on other drugs, including addictive substances such as cannabis and alcohol and therapeutic agents such as antidepressants and psychedelics. Dr. Gu is particularly interested in how drug potency could impact the effect of patient beliefs on their brains and behaviors and how long these effects could last. She is also interested in quantifying beliefs through conversations or therapeutic dialogues to examine how they impact brain signals and clinical outcomes.
“Our findings could potentially revolutionize how we view drugs and therapy in a much broader context of health,” she says.
Featured

Xiaosi Gu, PhD
Associate Professor of Psychiatry, and Neuroscience; Director of the Center for Computational Psychiatry