Although Asians are the fastest-growing population in the United States, accounting for 7 percent of the population, their participation in Alzheimer’s disease research has typically been less than 3 percent, and their representation can be as low as 0.5 percent in datasets and clinical trials. Mount Sinai is working with 16 academic medical research centers to increase such participation through the Asian Cohort for Alzheimer’s Disease (ACAD) study.
“Many Alzheimer’s disease variants are population-specific, have very different frequencies, and very different effect sizes,” says Clara Li, PhD, Associate Professor of Psychiatry at the Icahn School of Medicine at Mount Sinai, and principal investigator of the Mount Sinai site. “We need to bring Asian Americans into Alzheimer’s disease research, so we know if they have specific biomarkers associated with the disease and if they need unique treatments.”

Although researchers are learning more about biomarkers in Alzheimer’s disease, that knowledge remains limited when it comes to Asian populations, due to a historical lack of inclusion of those demographics in clinical trials. The Asian Cohort for Alzheimer’s Disease (ACAD) study seeks to close that gap by focusing on Asian Americans, says Clara Li, PhD, Associate Professor of Psychiatry at the Icahn School of Medicine at Mount Sinai.
Funded by a $40.5 million grant from the National Institute on Aging (NIA), part of the National Institutes of Health (NIH), the study is the first major Alzheimer’s disease genetics study for Asian Americans and Asian Canadians. The five-year study, which began in July 2023, aims to recruit 5,000 participants in more than 10 cities/metropolitan areas in the United States and Canada. Sites are collecting research participant histories, blood samples, cognitive tests, and lifestyle surveys.
Unveiling Alzheimer’s Pathways in Asian Populations
The research team will focus on identifying blood biomarkers to establish key pathways for the research community to study Alzheimer’s disease among Asian American and Asian Canadian populations.
ACAD Study at a Glance:
5 Years, >10 Sites
5,000
Participants
>$40M
Funding From NIH
The team will also explore nongenetic biomarkers, such as 40-residue amyloid beta (A40), 42-residue amyloid beta (A42), glial fibrillary acidic protein, neurofilament light chain, and phosphorylated tau 217, along with lifestyle and clinical information to build polygenic risk profiles of Alzheimer’s disease among Asian populations, which have been understudied when compared to those with European ancestry. These pathways could also be used to assess effectiveness of treatment, and whether a unique treatment strategy might be needed.
“Evaluation and treatment of Asian Americans with Alzheimer’s disease is based in large part on research findings that reflect European ancestry and thus may not be applicable to this group,” Dr. Li says. Literature has shown that several well-known Alzheimer’s disease-related genetic loci, such as APOE, SORL1, and ABCA7, have various frequency and effect size across populations.
“This study opens the door for us to develop and validate new ways to detect, diagnose, treat, and prevent the disease among these populations,” says Dr. Li.
Addressing Cultural and Language Barriers
The study will also help to address the linguistic and cultural barriers that have long contributed to underrepresentation among Asian Americans and Asian Canadians in Alzheimer’s disease research. These include the difficulty in obtaining informed consent to participate in studies, as well as the availability of cognitive tests in Asian languages—in which cultural and linguistic differences make assessment of cognitive abilities difficult or inaccurate.

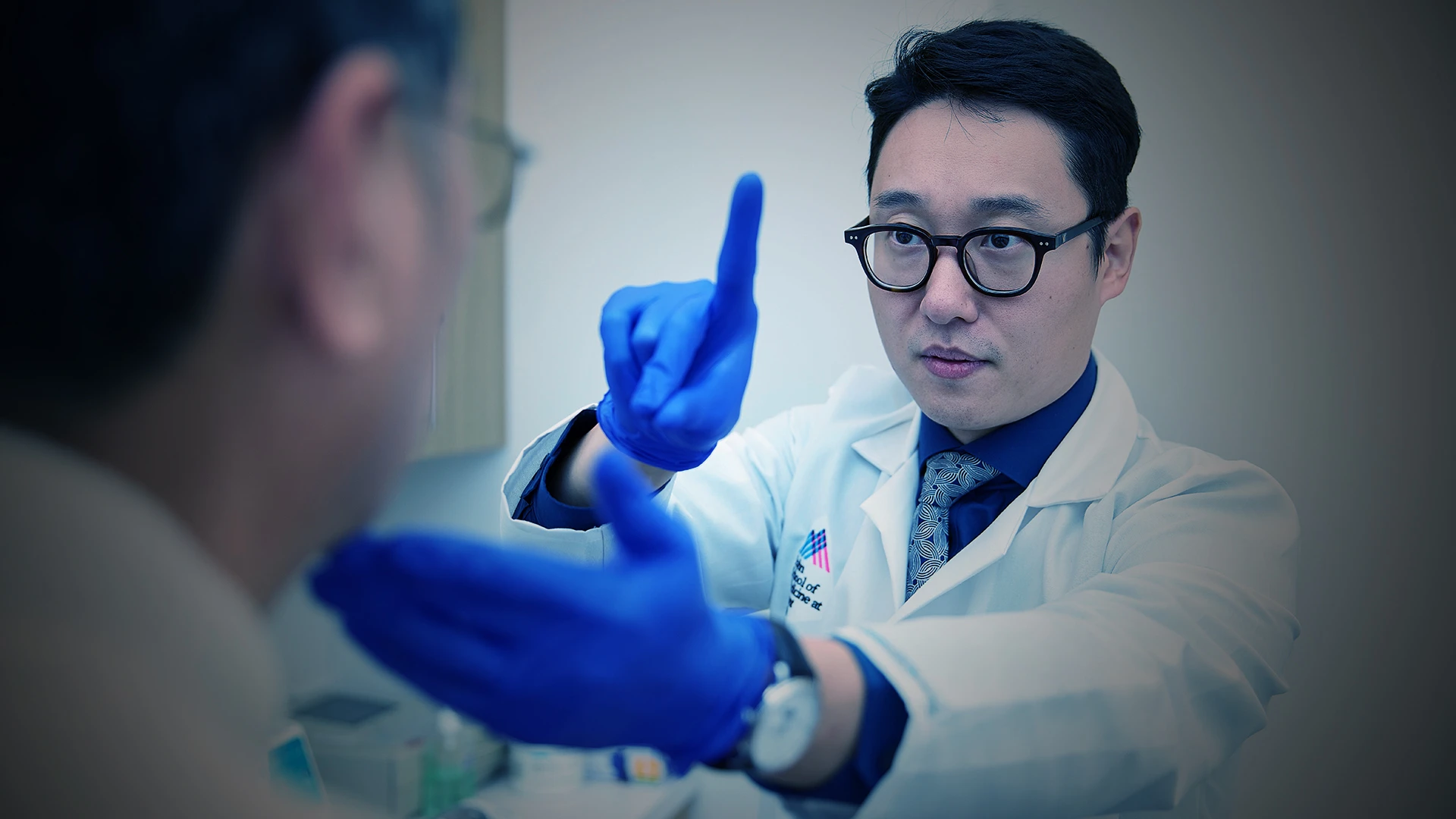
Dr. Li (right) is principal investigator of the Mount Sinai site. The study will look at known nongenetic biomarkers, including amyloid beta, glial fibrillary acidic protein, neurofilament light chain, and phosphorylated tau 217, to see how these proteins and peptides might be pathogenic in Asian populations.

Judith Neugroschl, MD, Associate Professor of Psychiatry at Icahn Mount Sinai, and members of Dr. Li’s team are also collecting lifestyle and clinical information to build polygenic risk profiles of Alzheimer’s disease.
“For example, on a standard confrontation naming test used in dementia evaluations, the stimuli might not always be relevant or identifiable to patients from non-Western countries. So, I have had patients who have identified a beaver as a rat, a pretzel as a snake, and other similar errors due to cultural and linguistic differences. This might incorrectly present as a sign of dementia or language impairment when, in fact, it might be more representative of other noncognitive factors,” Dr. Li says.
The ACAD research team consulted with community advocates on best practices for engaging Asian participants, and created the Brain Health, Education, and Risk of Dementia (B-HEARD) Core. It led to the development of culturally and linguistically appropriate outreach and assessment tools for the study. These tools were extensively tested during the study’s two-year pilot phase, with feedback incorporated into the study design. The team also recruited bilingual and trilingual staff—fluent across English, Mandarin, Cantonese, Korean, and/or Vietnamese—to help engage study participants.
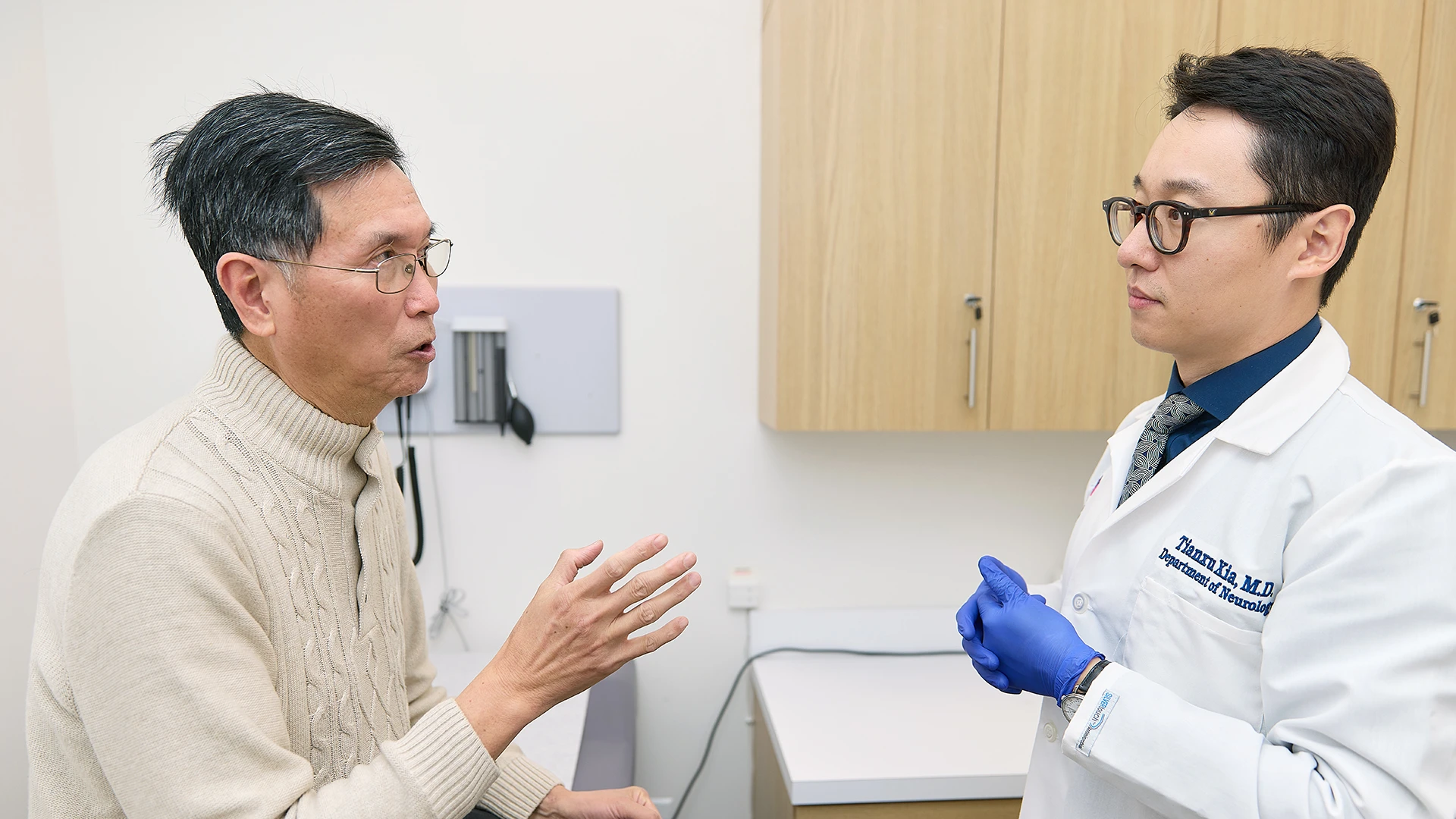
Tianxu Xia, MD, Assistant Professor of Neurology and Psychiatry (right) at Icahn Mount Sinai, sees patients with dementia and neurodegenerative conditions. As he conducts cognitive assessments for Asian populations, he might have to bridge language and cultural barriers, as lack of English proficiency from patients could result in inaccurate diagnoses, which has happened from practitioners historically.
Recruitment is underway at participating sites. The current focus is on recruiting adults with and without cognitive issues who are 60 and older and who are of Chinese, Korean, and/or Vietnamese ancestry, but there are plans to expand recruitment to more Asian subpopulations as the study progresses. That helps provide more insights into Alzheimer’s disease in Asian populations, but also helps dispel misconceptions about the disease among them.
“I think there is an assumption that Asian Americans are healthier and better educated, so they do not have a problem with Alzheimer’s disease,” says Dr. Li. But looking at the Alzheimer’s disease rate in other places, such as in China, it is clear that Asian people do get the disease. “This study thus represents a significant milestone in advancing our understanding of Alzheimer’s disease and related dementia in Asian populations in the U.S. and Canada,” she says.