The discovery by Rita Goldstein, PhD, Chief of the Neuropsychoimaging of Addiction and Related Conditions (NARC) research program at the Icahn School of Medicine at Mount Sinai, of people who are dependent on cocaine or heroin having signaling impairment in a specific brain pathway is groundbreaking for the science of drug addiction. Recent work from her team potentially uncovers a new target that could aid drug addiction treatment and prevention.
The study revealed there was a microstructural disruption in the pathway between the prefrontal cortex (PFC), which is responsible for regulating higher-order executive functions, and the habenula, a region pivotal to reward and reward-associated learning, and previously identified as a key driver of drug-seeking behaviors in animal models. Those findings in humans were reported in Neuron in November 2022.

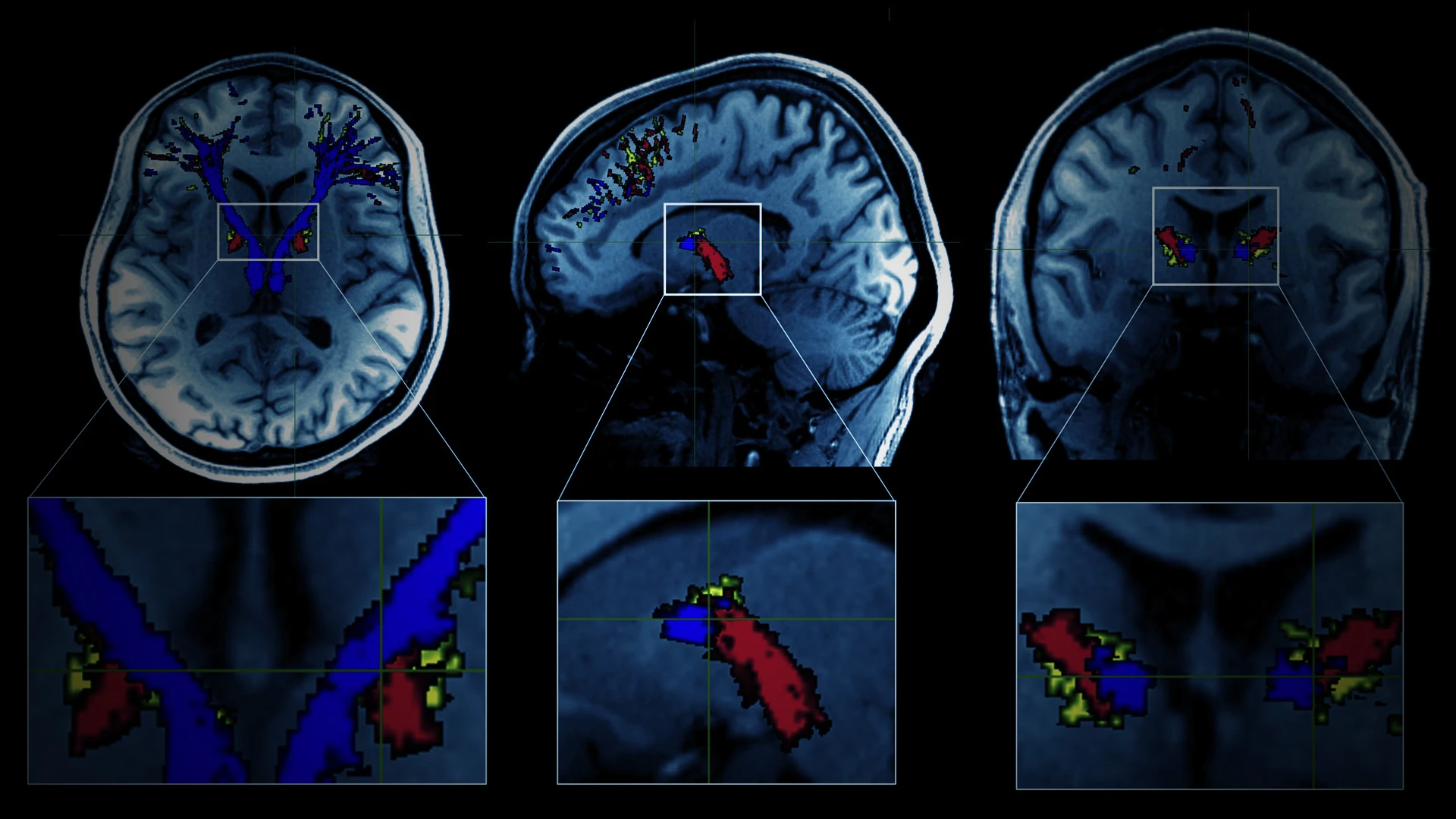
Using neuroimaging, researchers were not only able to map out the pathways between the prefrontal cortex and the habenula involved in cocaine and heroin addiction, but also show evidence for specific impairments along this tract.
Dr. Goldstein, who is the Mount Sinai Professor in Neuroimaging of Addiction, is currently also exploring how various therapies, along with her brain circuitry findings, could be used to benefit patients.
“We have been testing the use of transcranial direct current stimulation as an add-on therapy in drug addiction and are now excited about taking some of the preliminary findings to the next testing phase,” Dr. Goldstein says.
A Novel Target in Addiction Medicine
In the study published in Neuron, Dr. Goldstein’s team evaluated the microstructure of the PFC-habenula pathway of both healthy individuals and people with cocaine or heroin addiction using diffusion magnetic resonance imaging (MRI) tractography.
Her team found reduced diffusion along the PFC-habenula tract of both short-term abstainers and current cocaine users, compared to healthy control subjects. Similar results were seen in a separate cohort of people with heroin addiction, compared to their own control group. They also found that greater white matter disruption in the whole tract was associated with a younger age of first drug use across all addiction subgroups.

Nelly Alia-Klein, PhD, Associate Professor of Psychiatry, and Neuroscience at Icahn Mount Sinai (left), works closely with Rita Goldstein, PhD, Chief of the Neuropsychoimaging of Addiction and Related Conditions research program (right), to take findings further. This includes exploring additional biomarkers or finding ways to guide interventions for cocaine and heroin addiction.

The neuroimaging results in human addiction to cocaine and heroin that Dr. Goldstein (left) and Dr. Alia-Klein (right) are exploring have previously only been identified in animal models, and their efforts to build brain maps of risk- and reward-seeking behaviors hold great potential for collaboration with other drug addiction intervention researchers.
With the goal of turning these findings into concrete benefits for patients, Dr. Goldstein and her team are actively exploring these white matter and additional biomarkers that could facilitate early intervention, or predict treatment trajectory. They are drafting plans for a longitudinal neuroimaging study that assesses patient recovery over the course of an entire year to determine which kind of marker—blood (genetic, molecular) and/or behavioral—best correlates with patterns of change in the brain’s white matter.
“We know in the future we won’t be able to image people on a large scale because of cost, and that creates the need for identifying a predisposing marker, using something like a blood draw, that’s both accessible and affordable to the general population,” says Nelly Alia-Klein, PhD, Associate Professor of Psychiatry, and Neuroscience at Icahn Mount Sinai, and Co-Chief of the NARC research program.
Based on the team’s latest research, a core marker for addiction could be some measure of the microstructural deficit in the PFC-habenula tract, which could indicate vulnerability factors that contribute to or impact the development and maintenance of the addiction cycle. Exposure to drugs like cocaine or heroin during adolescence has been shown to impact neurodevelopment, Dr. Alia-Klein points out.

Dr. Goldstein examining a patient's brain MRI scan. Her team is pushing forward on a Phase 2 study that builds on initial findings regarding the direct brain stimulation of brain regions involved in cocaine and heroin addiction.
Other studies from this research team build on targeting brain circuitry for treating drug addiction and include the use of transcranial direct current stimulation of the dorsolateral prefrontal cortex, a hallmark region implicated in impairment of inhibitory control in drug addiction. A study, published in European Journal of Neuroscience in May 2021, administered this noninvasive, low electrical, direct current brain stimulation over 15 sessions encompassing five weeks to individuals with cocaine use disorder.
Though the Phase 1 study had a limited sample size, the Mount Sinai psychiatric team was encouraged by the results and are pushing forward with a Phase 2 study that is now ongoing.
“In addition to a reduction in self-reported craving, we saw in participants who received stimulation increases in arousal and motivation to change their drug use behavior, a proxy for treatment engagement and change,” notes Dr. Goldstein, senior author of the study.
An Advocate as an Ally
As Dr. Goldstein pushes forward in addiction science through neuroimaging, she works to ensure the advances are for the sake of a core group: people. A key component to achieving that goal is the addition of Alan Charles, who overcame cocaine addiction, to her lab three years ago. Mr. Charles is an important part of the team’s subject recruitment efforts.
Mr. Charles battled a cocaine addiction for 24 years, and lost many things in his life, including relationships with spouses and children, and homes. But he recovered from that addiction, through rehabilitation programs, and has written a book about his journey.
Recruitment for addiction studies can be tricky, given the inherent stigma of even seeking treatment for substance-use disorders in the first place. “We knew that Alan would be a great addition to our lab by helping us communicate clearly to people with addiction about our studies and their relevance to their struggles,” Dr. Goldstein remarks.
Having an advocate who has experience recovering from addiction helps dispel the stigma of seeking treatment. “He brings it down to ground level for these individuals by being intimately familiar with what they’ve been through,” Dr. Goldstein adds.
“I’m not a doctor or a scientist,” says Mr. Charles. “I was a person with addiction, just like they are. And when I sit with them and they listen to my story, they let their guard down and start to see there is hope. That they, too, can get better.”
Featured

Rita Goldstein, PhD
Chief of Neuropsychoimaging of Addiction and Related Conditions Program; Mount Sinai Professor in Neuroimaging of Addiction

Nelia Alia-Klein, PhD
Associate Professor of Psychiatry, and Neuroscience, Icahn School of Medicine at Mount Sinai