For the past 10 years, Grant Mitchell, MD, Chair of Psychiatry at Mount Sinai Beth Israel, has imparted to his residents a message about the mental health system: it fails too many patients and their families.
The existing system clearly needs reform, he notes. Patients and families face challenges in accessing timely care, having to navigate care that is often decentralized and lacks sub-acute, or step-down, outpatient behavioral health services. The situation is further complicated by the fact that many patients with mental illness also experience physical health problems and substance-use disorders, which must be addressed, as well.
“Unfortunately, patients often end up having to attend multiple programs in different locations, which contributes to fragmented care and poor outcomes,” says Dr. Mitchell.

Patient Care Assistants Whitleigh Webb (left) and Deny Alexis (right) play important roles in providing compassionate and dignified care at the Mount Sinai Behavioral Health Center, helping patients with basic needs.
The Mount Sinai-Behavioral Health Center (MSBHC) reimagines how to deliver behavioral health care and aims to break down the current silos by integrating all of these services in one location. This landmark initiative, which had its grand opening event on June 8, will help prevent patients from falling through the cracks and provide critical new services to address gaps in the continuum of behavioral health care.
This $140 million, 135,000-square-foot facility—believed to be the largest private investment in mental health care in New York State history—offers a seamless, integrated, patient-centric approach to treatment and clinical research by having mental health, substance use, and primary care in the same location.
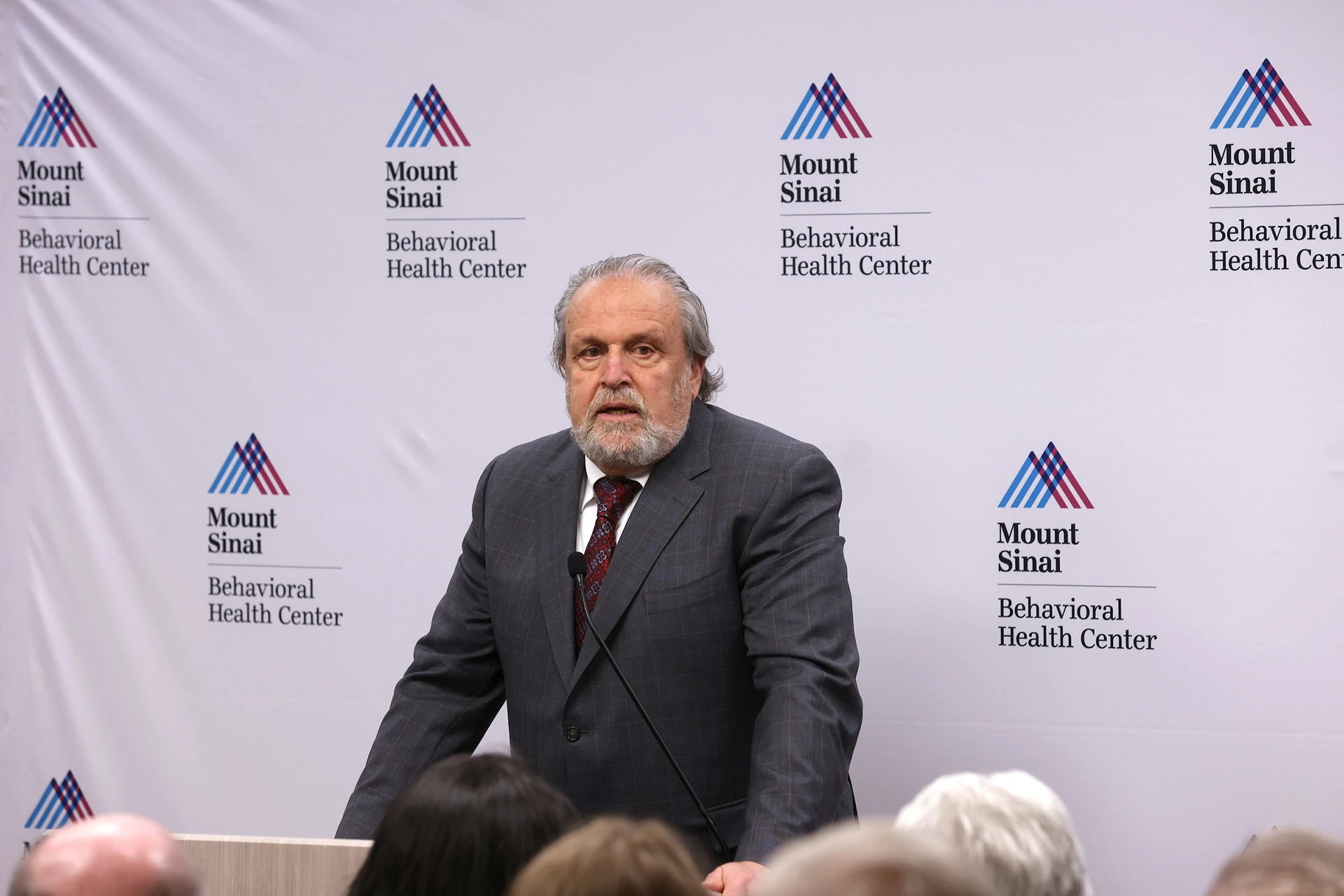
Mount Sinai is committed to investing in behavioral health resources for the community, despite challenging economic climates, says Dennis Charney, MD, Anne and Joel Ehrenkranz Dean of the Icahn School of Medicine at Mount Sinai, at the ribbon cutting ceremony of the Mount Sinai Behavioral Health Center.
“The Behavioral Health Center reflects a major commitment to mental health by Mount Sinai in all aspects—from substance-use disorders to serious mental illness conditions, such as schizophrenia and bipolar disorder, to primary care,” says Dennis S. Charney, MD, Anne and Joel Ehrenkranz Dean of the Icahn School of Medicine at Mount Sinai and President for Academic Affairs of the Mount Sinai Health System.
“We feel it is our obligation to make those kinds of discoveries, and, through MSBHC, we have brought together the resources to make that happen,” Dr. Charney says.
The facility means dedicated space and resources for the Department of Psychiatry, without a need to compete with other disciplines, says René S. Kahn, MD, PhD, Esther and Joseph Klingenstein Professor of Psychiatry at Icahn Mount Sinai, and Chair of Psychiatry for the Mount Sinai Health System. “That means we can focus our extensive academic, clinical, and training expertise on developing a research program, delivering quality care to our patients, and launching new programs and approaches for treatment.”
Origins and Features of the Mount Sinai-Behavioral Health Center
To meet increased needs for mental health services, especially following COVID-19, and to advance scientific breakthroughs, Mount Sinai leadership recognized that a retrofit or refresh of the Department of Psychiatry's longstanding location at Mount Sinai Beth Israel would not be sufficient. The Health System chose a historic six-story building known as Rivington House as the canvas for reimagining what behavioral health care and dedicated research space under the same roof could look like and engaged HKS, a Dallas-based firm, as the architect.
“We made a commitment early on to listen and incorporate ideas and feedback from our patients, families, staff, and the community as the building and programs were being designed,” Dr. Mitchell says.
The design that emerged features natural light, top-end flooring, high ceilings, and comfortable furnishings to create a welcoming ambience rather than a clinical one. Inpatient rooms are limited to one or two patients to offer more privacy, minimize noise, and optimize comfort.
The site’s co-location and integration of mental health, substance use, and primary care services are important, as many people who have mental health challenges also have substance-use disorders and physical health issues, says Prameet Singh, MD, Vice President of Behavioral Health, and Associate Professor of Psychiatry.

Mount Sinai senior leadership and officials from New York City and New York State came together to welcome the opening of the Center, which was lauded as a sorely needed facility in a neighborhood where the need for such services was high.

The Mount Sinai Behavioral Health Center establishes a new model of care that is compassionate, dignified, and integrated for patients, says Grant Mitchell, Chair of the Department of Psychiatry, Mount Sinai Beth Israel.
“We also know that people who have a range of issues tend to drop out of treatment because it is often impossible to adhere to such a complicated regimen,” Dr. Singh says. “By concentrating all aspects of treatment in one location, we believe we can improve adherence to treatment and thus achieve better outcomes than are possible by just focusing on mental health.”
MSBHC has designed programs to create a continuum of care that bridges the gaps in traditional inpatient and outpatient care. “We can increase or decrease the support we deliver to meet our patients where they are in their mental health journeys,” says Jeremy Boal, MD, Executive Vice President and Chief Clinical Officer of the Mount Sinai Health System, who was president of Mount Sinai Beth Israel when the MSBHC project was conceived.
For example, patients can transition from inpatient care to an array of outpatient services, including the partial hospital program, which enables them to sleep in their own beds at night while continuing to receive counseling, monitoring, and group therapy support each day. “By establishing a longitudinal connection, we can gain insights on their progress, intervene when there are issues, and thus reduce the risk of rehospitalization,” says Dr. Boal.
A Focus on Research
The Mount Sinai Behavioral Health Center will conduct basic science as well as clinical research, with the latter providing access for patients to innovative therapeutic approaches that are not yet widely accepted or available. Those efforts will be facilitated, in part, by the diversity of the population MSBHC serves, which will help address inequities in treatment and innovation.
“There is a great unmet need for new interventions, either psychological or pharmacological,” Dr. Kahn says. The Center is looking at launching clinical trials that look at risk factors for addiction, both genetic and environmental, and studies on the therapeutic potential of psychedelics to treat patients with post-traumatic stress disorder and on the molecular mechanisms of depression.
The goal underpinning Mount Sinai’s investment in this transformation will be measured by its impact on patients. “For me, this is all about outcomes,” says Dr. Charney. “Are the results of our treatment superior to those being achieved by any other facility in New York City or nationwide? Are we collaborating in ways that are addressing our patients’ comorbidities? Are we discovering therapeutic modalities that are changing the lives of people with mental illness? Those are the metrics I will be looking at to measure success, but I fundamentally believe that, through the Mount Sinai-Behavioral Health Center, we have made a significant commitment to advancing the understanding and treatment of mental illness.”
Featured

Jeremy Boal, MD
Executive Vice President and Chief Clinical Officer of the Mount Sinai Health System

Dennis S. Charney, MD
Anne and Joel Ehrenkranz Dean of the Icahn School of Medicine at Mount Sinai, President for Academic Affairs of the Mount Sinai Health System

René S. Kahn, MD, PhD
Esther and Joseph Klingenstein Professor and Chair, Department of Psychiatry and Behavioral Health

Grant Mitchell, MD
Chair of Psychiatry at Mount Sinai Beth Israel
Prameet Singh, MD
Vice President of Behavioral Health, Associate Professor of Psychiatry




