As researchers continue to make significant inroads in the investigation of genetics, genomic sciences, and precision medicine in the fields of cancer and cardiovascular disease, Mount Sinai’s Panos Roussos, MD, PhD, MS, is looking to make similar breakthroughs in neuropsychiatric disorders by establishing the Center for Disease Neurogenomics (CDN).
“The human brain is a complex and vast field of study, with billions of cells, thousands of cell types, and many different brain regions,” says Dr. Roussos, Professor of Psychiatry, and Genetics and Genomic Sciences, at the Icahn School of Medicine at Mount Sinai, and member of The Friedman Brain Institute and the Icahn Genomics Institute.
“Our goal is to understand how genetic liability affects this developmental process, determine which cell types and molecular markers are affected as disease progresses, and use those insights to enable effective, personalized therapeutic approaches.”
Panos Roussos, MD, PhD, MS
Launched in 2022, the Center’s exploration of the genetics of neuropsychiatric disorders has the potential to predict the severity of clinical phenotype, optimal treatment, and outcomes for each patient. These spell significant benefits for a broad swath of the population. For instance, more than 6 million Americans are living with Alzheimer’s disease, and this number is projected to rise to nearly 13 million by 2050. But the Center’s work would also benefit millions of Americans who live with, or are caregivers to someone who has, schizophrenia, Parkinson’s disease, bipolar disorder, depression, and other neuropsychiatric and neurodegenerative diseases.
“We are interested in how genetics can be used for the benefit of patients, specifically in identifying therapeutic approaches that would work best for them,” Dr. Roussos says. “Ideally, we would not treat every schizophrenic patient with the same medication; instead, through our research, we could use their genetic profile to identify the most effective treatment for each person. However, finding effective drug targets for neuropsychiatric disease is challenging because there are no reliable biomarkers and the effect of each genetic risk factor is very small.”

Members of the Center for Disease Neurogenomics, from left to right: Georgios Voloudakis, MD, PhD; John F Fullard, PhD; Gabriel E Hoffman, PhD; Panagiotis Roussos, MD, MS, PhD; Kiran Girdhar, PhD; Donghoon Lee, PhD; Jaroslav Bendl, PhD

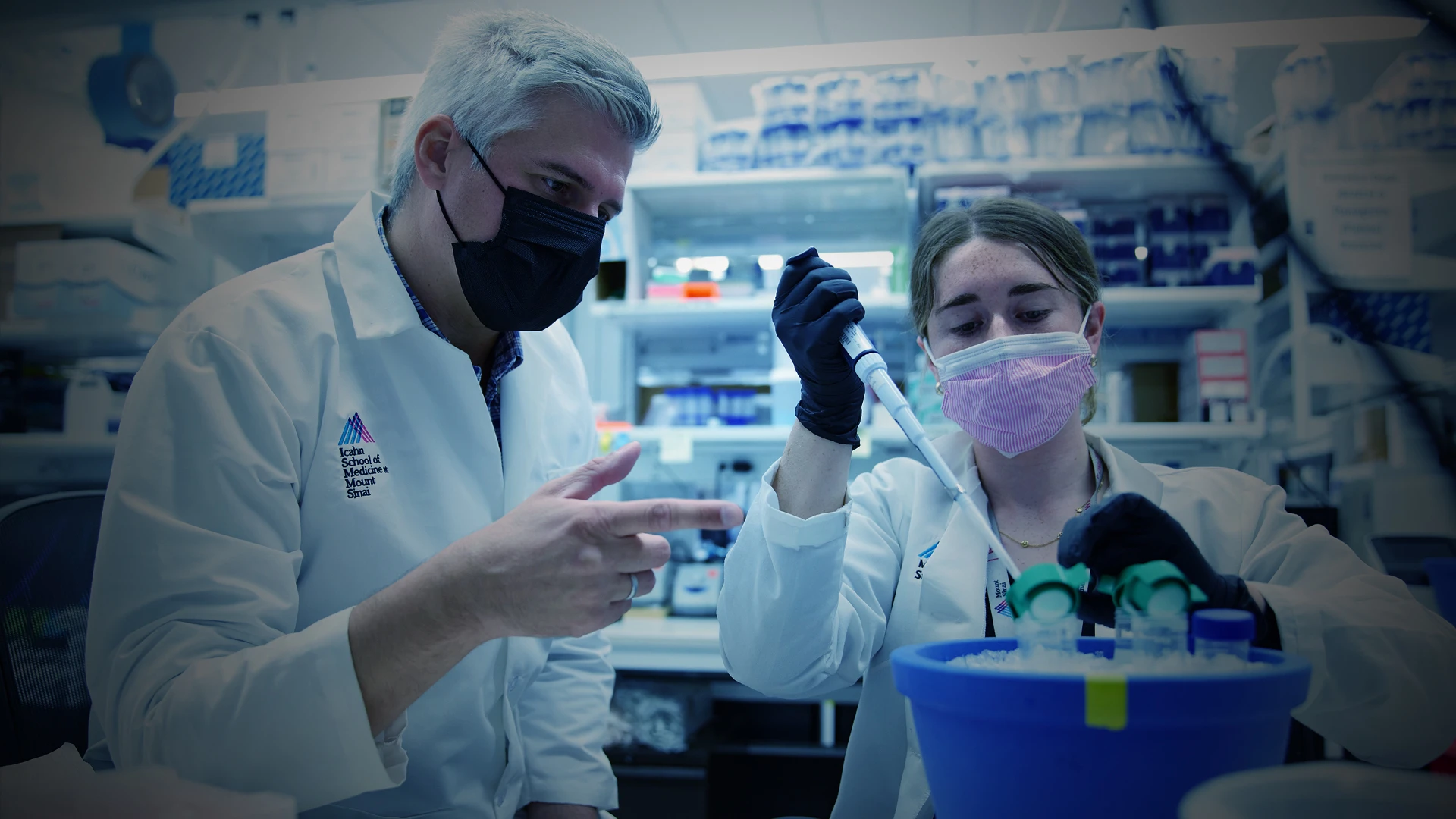
Dr. Roussos attending a presentation of findings from team members.
Two Key Ingredients: Interdisciplinary Expertise and Access to Population-Level Data
To overcome those challenges, the Center is taking an interdisciplinary approach that brings together computational scientists, biomedical scientists, psychiatrists, and genomic scientists. Many of its researchers are cross-trained and have advanced knowledge in key areas that span “omics” technology, single-cell biology, data integration using artificial intelligence, and statistical genetics.
That breadth and depth of genetic expertise will further benefit from the Center’s unparalleled access to brain tissue and datasets that reflect the population-level sample sizes necessary to conduct such vital research. Data sources include biorepositories, such as the Million Veteran Program, the Mount Sinai BioMe BioBank program, the UK BioBank, and psychEMERGE. Relationships with brain banks, neurosurgeons, and health care systems are also providing access to fresh brain tissue, which is advantageous to study cells that are critical for Alzheimer’s disease.
These data are enabling researchers to conduct large-scale studies—including groundbreaking multi-ethnic studies—that are leading to a deeper understanding of risk variants and genetic liability. And findings from those studies are fed through Mount Sinai’s supercomputer Minerva, a powerful resource that enables analysis and management of data. Combined, they create a solid foundation for innovation in neuropsychiatric disorder investigation that has already resulted in the development of several groundbreaking techniques to meet the Center’s objectives, including:
Innovative methods to isolate human brain cells to perform cell-type specific assays and generate large-scale functional omics;
New computational and machine-learning approaches to analyze large scale functional omics and understand cellular and molecular mechanisms in disease perturbation; and
Novel predictive models to assess gene expression, disease manifestation, and treatment outcomes
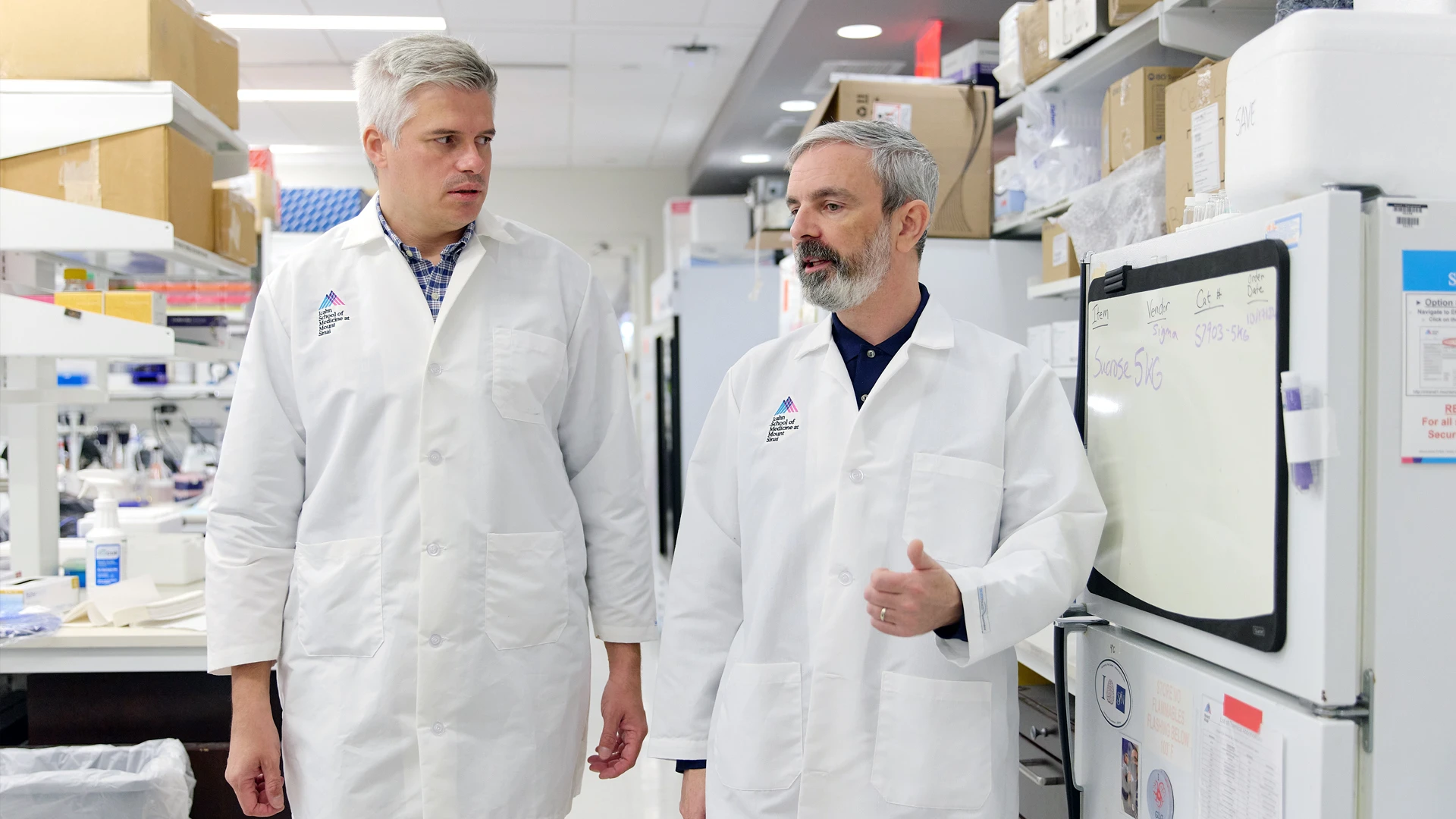
Dr. Roussos with Dr. Fullard in the wet lab.
“I’m energized by this team’s enormous productivity in just six months,” Dr. Roussos says. “We are functionally validating our findings in cell-type specific contexts. And we are translating these discoveries to uncover new drug targets, repurpose existing drugs for neuropsychiatric diseases, and optimize treatment for each individual based on their genetic profile—which is the ultimate goal of precision psychiatry, and will pave a new era in patient-centric care.”
Featured

Panos Roussos, MD, PhD, MS
Professor of Psychiatry, and Genetics and Genomic Sciences