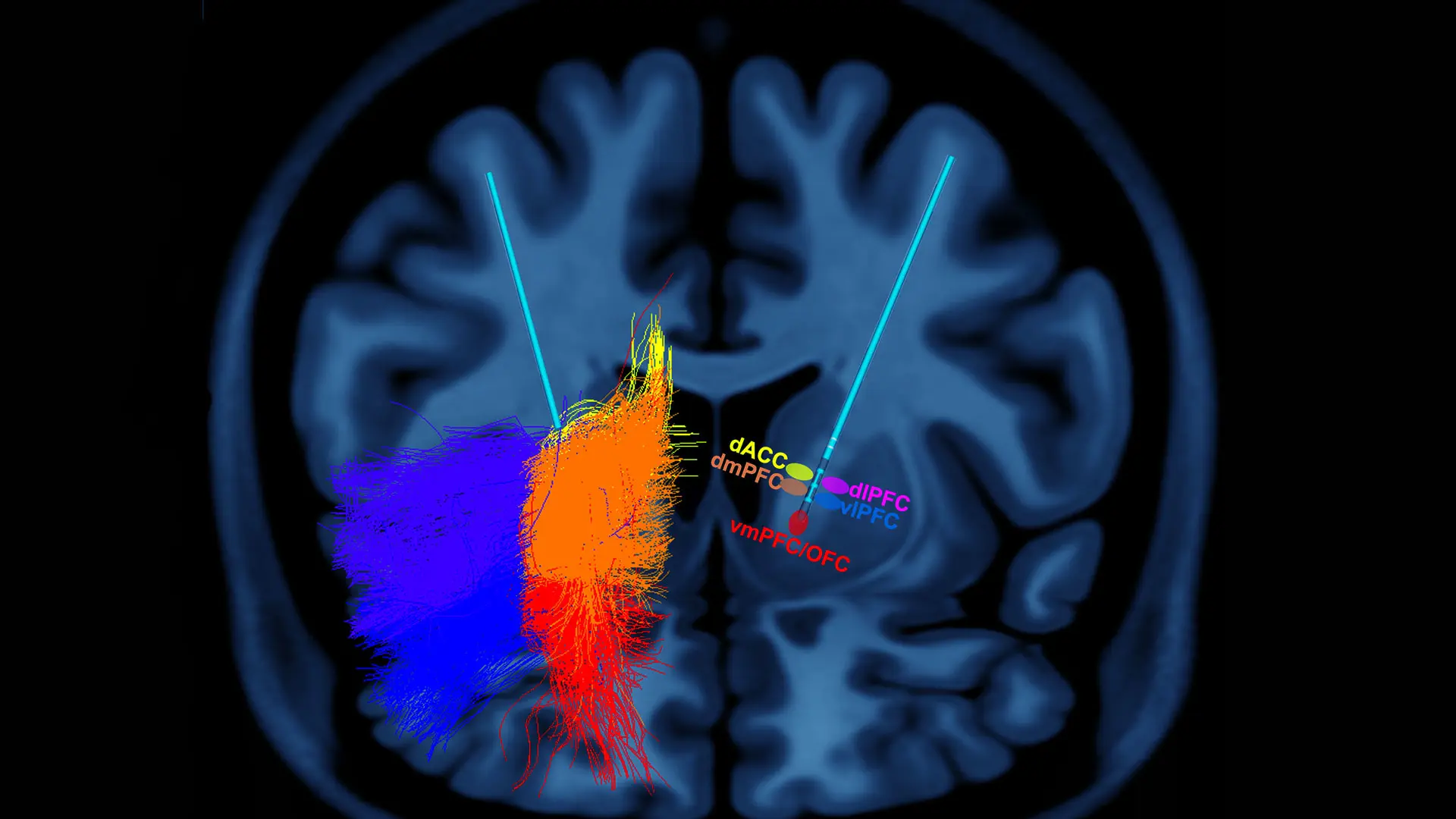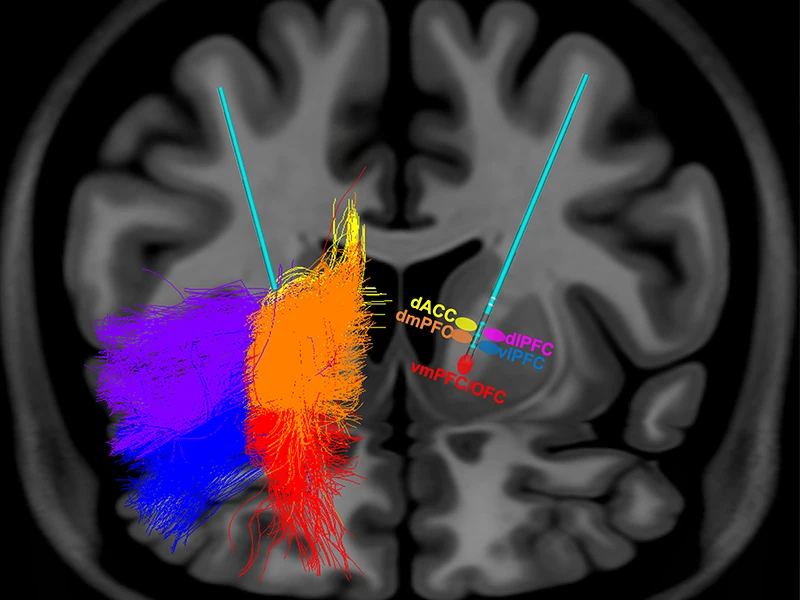
This image highlights symptom and circuit selective stimulation in deep brain stimulation (DBS) for obsessive-compulsive disorder. The colored areas represent the selective white matter tracts impacted by stimulation at respective contacts on the DBS electrode.
The unique pairing of two highly specialized research centers of excellence at the Icahn School of Medicine at Mount Sinai has generated some of the nation’s most integrative applied research into the brain for treating complex neuropsychiatric disorders. By leveraging the Center for Computational Psychiatry with the deep brain stimulation (DBS) scientific expertise of the Nash Family Center for Advanced Circuit Therapeutics (C-ACT), Mount Sinai is producing a growing body of transdisciplinary research, including innovative new studies about the use of DBS for obsessive-compulsive disorder (OCD) and treatment resistant depression (TRD).
“The synergy of research and clinical care catalyzed by the co-localization of clinicians and neuroscientists at C-ACT is enabling us to systematically interrogate the various brain circuits that underlie severe psychiatric illnesses during DBS treatment,” says Helen Mayberg, MD, Founding Director of C-ACT, and Professor of Neurology, Neurosurgery, Psychiatry, and Neuroscience at the Icahn School of Medicine at Mount Sinai. “We have organized our human research questions around ongoing surgical neuromodulation treatments, drawing on a wide range of experts, including those in psychiatry, neurology, neurosurgery, radiology, engineering, and neuroscience.” This effort would not have been possible without the dedication and support from the Department of Neurosurgery and the clinical Center for Neuromodulation at Mount Sinai West.
A critical partner for new discoveries in this growing field is the Center for Computational Psychiatry—one of the first integrated centers in the world to study how algorithms and big data can improve mental health diagnosis and treatment. “Dr. Mayberg’s team brings human DBS and clinical psychiatric experience to the table, while our group brings basic neuroscience and computational experience,” says Xiaosi Gu, PhD, Director of the Center for Computational Psychiatry, and Associate Professor of Psychiatry, and Neuroscience. “It’s a truly balanced partnership.”
“Dr. Mayberg’s team brings human deep brain stimulation and clinical psychiatric experience to the table, while our group brings basic neuroscience and computational experience. It's a truly balanced partnership.”
- Xiaosi Gu, PhD
The area of OCD is emblematic of their joint success. Dr. Mayberg says, "C-ACT’s ongoing imaging and electrophysiological studies in the surgical OCD treatment program at Mount Sinai West have made important advances in recent years, but new computational approaches will take this work to the next level. Dr. Gu's group was able to provide that advantage, which in turn helped us secure a major new grant, with opportunities for many additional projects across other disorders treated with DBS.”
Dr. Gu and Vincenzo Fiore, PhD, Assistant Professor of Psychiatry, have also joined forces with the OCD research group at C-ACT on a new National Institute of Mental Health grant led by co-principal investigators Martijn Figee, MD, PhD, Associate Professor of Psychiatry and Neurosurgery; and Ki Sueng Choi, PhD, Assistant Professor of Neurosurgery, Diagnostic, Molecular, and Interventional Radiology. Other key investigators on the project include Allison C. Waters, PhD, Assistant Professor of Psychiatry, and Neuroscience; and Brian Kopell, MD, Professor of Neurosurgery, Neurology, Psychiatry, and Neuroscience.
The team has refined the surgical approach to a well-established clinical DBS target for OCD, a complex white matter fiber bundle called the anterior limb of the internal capsule (ALIC), with encouraging new results. Their challenge, however, has been to better define the specific pathways that travel through the ALIC that mediate specific
symptom changes and optimal clinical outcomes in OCD patients treated with DBS.
This team will work on new innovative treatments for OCD
Dr. Gu’s and Dr. Fiore’s computational expertise adds an important quantitative behavioral readout of these pathways’ specific stimulation effects, building on imaging studies by Drs. Choi, Figee, and Kopell, and electrophysiological signatures defined by
Dr. Waters. Together, the team will construct a comprehensive network blueprint, or “atlas,” for OCD using the association of white matter structural connections, electrocortical responses, and behavioral outcomes to refine DBS surgery and guide DBS treatment delivery in order to maximize clinical outcomes for patients. More information about the work can be found here.
This innovative, transdisciplinary research approach, now being tested in treatment-resistant OCD and depression (two of the most challenging psychiatric disorders), has already provided important new scientific insights with direct impact on DBS treatment and patient outcomes. As this collaboration continues to grow and mature, the opportunities for development of additional neuroscience-informed circuit therapeutic
treatment options for other severe psychiatric disorders will lead to profound
implications for the future of patient care.
Featured

Xiaosi Gu, PhD
Director, Center for Computational Psychiatry, and Associate Professor of Psychiatry, and Neuroscience

Helen Mayberg, MD
Director of the Nash Family Center for Advanced Circuit Therapeutics, and Professor of Neurology, Neurosurgery, Psychiatry, and Neuroscience