Specialists in different disciplines may prescribe the same immunotherapy drug for their patients, but the unique insights they’ve gleaned as a result often remain only within their own academic circles.
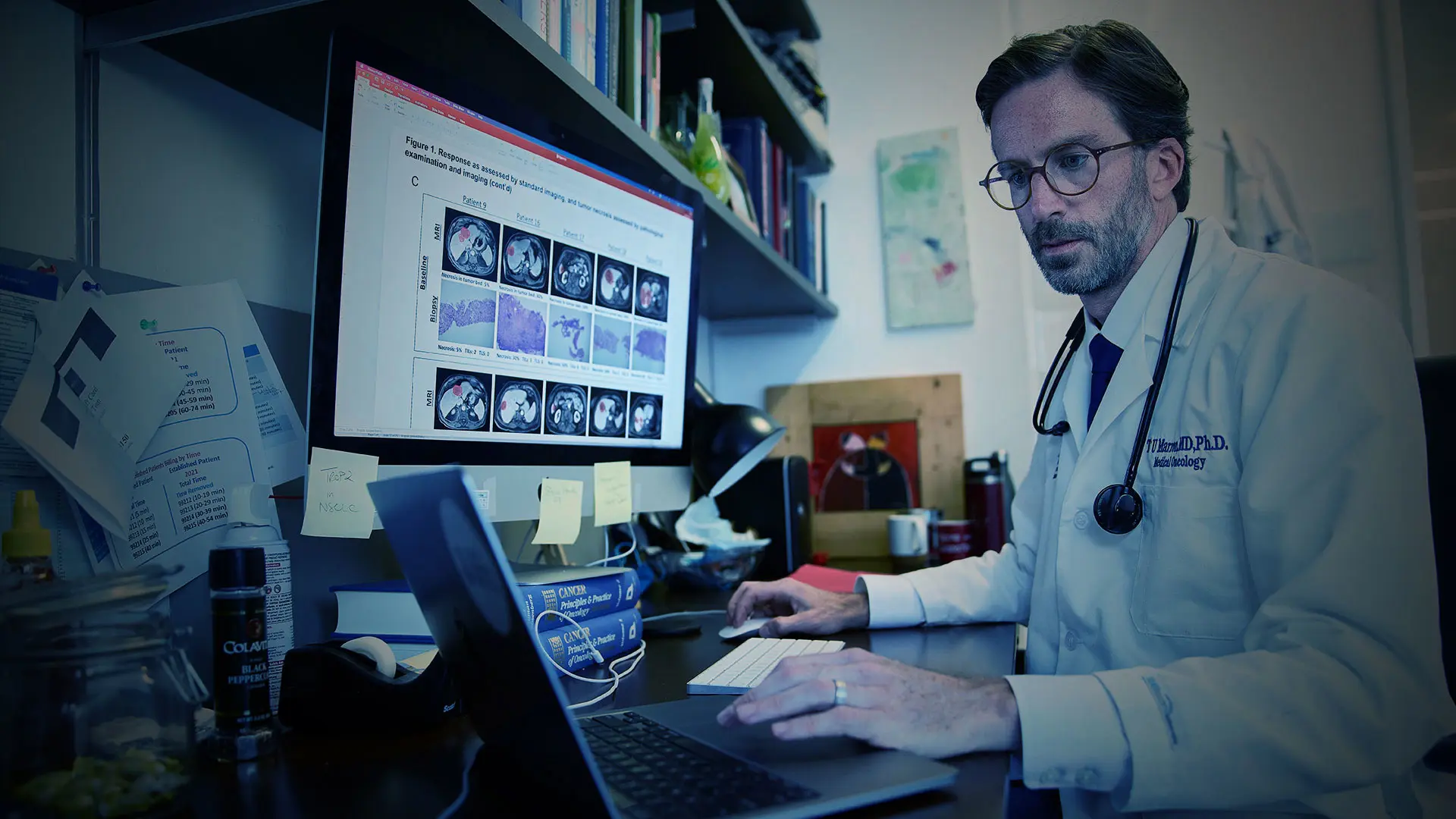
“At other large academic institutions, researchers tend to work in these silos where we don't talk to each other. Oncologists aren't necessarily talking to the rheumatologists, neurologists, and cardiologists about their work in understanding and treating the immunologic defects underlying the diseases in their respective clinics,” says Thomas Marron, MD, PhD, Director of the Early Phase Trials Unit in The Tisch Cancer Institute (TCI) at the Icahn School of Medicine at Mount Sinai.
To bridge these silos, Dr. Marron and Miriam Merad, MD, PhD, Director of the Marc and Jennifer Lipschultz Precision Immunology Institute at Icahn Mount Sinai (PrIISM) and co-Director of the Cancer Immunology Program at TCI, have launched two programs: The Neoadjuvant Research Group to Evaluate Therapeutics (TARGET) and the Immunotherapy and Novel TargEt Research Across Clinical Teams (INTERACT).
Thomas Marron, MD, PhD, with patient
These translational research platforms, described in Nature Medicine in March 2022, are intended to guide new treatment regimens by fostering highly productive collaborations among physicians and researchers.
TARGET aims to expedite the identification of new immunotherapy treatments for patients with cancer and optimize the use of the new therapies being developed today; while INTERACT focuses on fostering collaborations—both scientific and clinical—among physician-scientists who specialize in studying a myriad of diseases related to faulty immune systems. They are designed to extract the most useful information from the high-dimensional immune profiling capability of the Human Immune Monitoring Center (HIMC) in PrIISM. INTERACT features meetings to promote sharing of early data and brainstorming about how biologics being successfully used in one disease may be helpful to other patient groups, such as those in whom a similar immune pathway gone awry had been identified by immune profiling. Oncologists leading TARGET are working within the infrastructure provided by INTERACT to build bridges between the field of oncology and other fields treating immunological diseases, to help repurpose biological therapies developed elsewhere for cancer patients, and vice versa.
INTERACT was started during Mount Sinai’s response to COVID-19. As the epicenter of the early pandemic, Mount Sinai physicians were trying various antibody treatments and drugs that anecdotal experiences from China and Italy suggested may help to limit cytokine storms in patients who were very sick, Dr. Marron said. But identifying the key cytokines to target therapeutically proved tricky.
“We realized the drugs weren’t really doing what we wanted,” Dr. Marron said. “The Infectious Diseases doctors asked us, ‘What other things should we try?’” As he spoke with other specialists at Mount Sinai who were not oncologists, such as rheumatologists and dermatologists, he realized there were many biologics approved by the U.S. Food and Drug Administration (FDA) that he didn't even know about. “They're using so many cytokine-targeted therapies that I don't normally use as an oncologist,” Dr. Marron said. “We realized that these silos we work in make us oblivious to the biologic therapies being regularly used in other specialties that might be applicable for cancer and other diseases.”
Sharing Solutions to the Shared Immune Mechanisms of Disease
Dr. Merad initially set up regular meetings for immunologists within PrIISM with diverse clinical expertise to talk about how to treat COVID-19. But as the pandemic waned back in June 2020, Drs. Marron and Merad realized that this collaborative approach could be used for other diseases that have common immune mechanisms, and evolved that pandemic task force into the INTERACT program

Researchers from different medical specialties began sharing cutting-edge data in their respective fields and began strategizing how to synergize their trials. For example, Drs. Merad and Marron recently found that lung cancer shares an immune component with eczema and asthma. It also turned out that alopecia areata—an immune-related condition that causes baldness—shares this same immune mechanism. INTERACT researchers Dr. Marron and Emma Guttmann, MD, PhD, Chair of the Department of Dermatology, are now leading parallel trials of dupilumab, used for eczema and asthma, to treat lung cancer and alopecia.
Other efforts from INTERACT members Dusan Bogunovic, PhD, Director of the Center for Inborn Errors of Immunity; and Brian Kim, MD, Director of the Mark Lebwohl Center for Neuroinflammation and Sensation, include exploring how inhibitors of specific Janus kinases—enzymes that control inflammation—can be used to treat different inflammatory diseases.
Physician-scientists participating in INTERACT act as ambassadors within their specialties, spreading the word about the role the immune system can play in disease and what existing FDA-approved treatments might merit testing. “It's really about bringing all the different teams of physician-scientists together so that we tear down those silos and we all work together as a team. We can learn from each other and move our respective fields forward even faster at the same time,” Dr. Merad said.
Harnessing Window-of-Opportunity Trials to Understand Cancer Drugs
Similarly, the TARGET program applies the core principles of teamwork and data sharing to early-phase cancer immunotherapy trials. It focuses on novel immunotherapies that can activate the immune system to recognize and kill cancer cells.
“Understanding why some patients respond and why some do not to a specific drug treatment will help identify novel drug targets and potential biomarkers of response.”
- Thomas Marron, MD, Phd
High-dimensional immune profiling was already being employed in PrIISM by Sacha Gnjatic, PhD, as Director of the Mount Sinai Cancer Immune Monitoring and Analysis Center (CIMAC), one of four centers that form an Immuno-Oncologic Biomarkers Network, to understand how cancer immunotherapies work and to identify new targets and biomarkers. The CIMACs are funded by the National Cancer Institute Cancer Moonshot program and via the Partnership for Accelerating Cancer Therapies with 12 pharmaceutical companies.

In TARGET, several groups working in the neoadjuvant space sample the tissue, blood, and stool of patients who are scheduled to have their cancers removed. The patients are then given a brief intervention of immunotherapy, and then have the tumors removed as they normally would. Using the high-dimensional profiling capabilities of the HIMC, available at few academic centers, TARGET researchers compare the samples before and after the intervention, and can characterize the dynamic changes that are happening and also look at the heterogeneous responses among patients.
“That’s really going to enable us to find who is going to respond and who is not, and the reasons for these different responses” said Dr. Merad. “Our primary goal is to not waste our time, or more importantly our patients’ time, using anything but the optimal drug combinations to cure cancer.”
One study using the TARGET platform was published in The Lancet Gastroenterology & Hepatology in March 2022. The findings showed that an immune checkpoint blockade therapy currently used in treatment of late-stage hepatocellular carcinoma might be more efficacious when given much earlier, before surgical removal of the tumor. Myron Schwartz, MD, Director of Liver Surgery, led this study with Dr. Marron.
“Our hope is that giving immunotherapy before surgery will enable the patient’s immune system to recognize and destroy these microscopic tumor deposits before they grow to be detectable.”
- Myron Schwartz, MD
Further high-dimensional profiling performed by the Merad team on these patients during this window of opportunity trial has revealed that responders have specific cellular and molecular interactions in tumor tissues. The results are posted in this preprint, and the researchers are now exploring how to promote these beneficial interactions in cancer lesions using different experimental models.
By combining forces with other oncologists at Mount Sinai, all tumor types can be examined. And by using complementary protocols for immune profiling in trials in the TARGET platform, researchers can compare datasets as well. Immunotherapy targeting these shared pathways could potentially be treatment options for a variety of cancers.
In addition to its large clinical capability, Mount Sinai has cutting-edge tools that TARGET could leverage. “We have amazing surgeons and pathologists, radiologists, and interventionalists, but we also have arguably the best immune monitoring center in the world that can look at the single-cell transcript and proteomic level,” Dr. Marron said.
“Through a clinical trial that enrolls 21 patients, we obtain trillions of data points. We have all these tools that allow us to probe in depth how these drugs are working, so we can really define what is happening at the single-cell level, and we can use them more intelligently,” Dr. Marron said. “Our goal is to use these drugs better so we don’t merely treat cancer, rather we cure cancer.”
Featured

Thomas Marron, MD, PhD
Director of the Early Phase Trials Unit in The Tisch Cancer Institute
Miriam Merad, MD, PhD
Mount Sinai Professor in Cancer Immunology; Director of PrIISM