The recent explosion of new therapies for inflammatory bowel disease (IBD) has been a remarkable development for patients, but the large number of therapies makes it hard to choose. This often means children must go through successive unsuccessful trials of medications to find one that works.
A game-changing approach using skin tapes is being pioneered at Mount Sinai Health System by Elizabeth A. Spencer, MD, MS, Assistant Professor of Pediatrics (Gastroenterology) in the Jack and Lucy Clark Department of Pediatrics at the Icahn School of Medicine at Mount Sinai. She is leading several cutting-edge initiatives to foster non-invasive precision care for children with IBD and related high-risk conditions, partnering with world-renowned dermatologist Emma Guttman-Yassky, MD, PhD, Waldman Chair of Dermatology at Icahn Mount Sinai and Chair of the Kimberly and Eric J. Waldman Department of Dermatology for the Mount Sinai Health System.
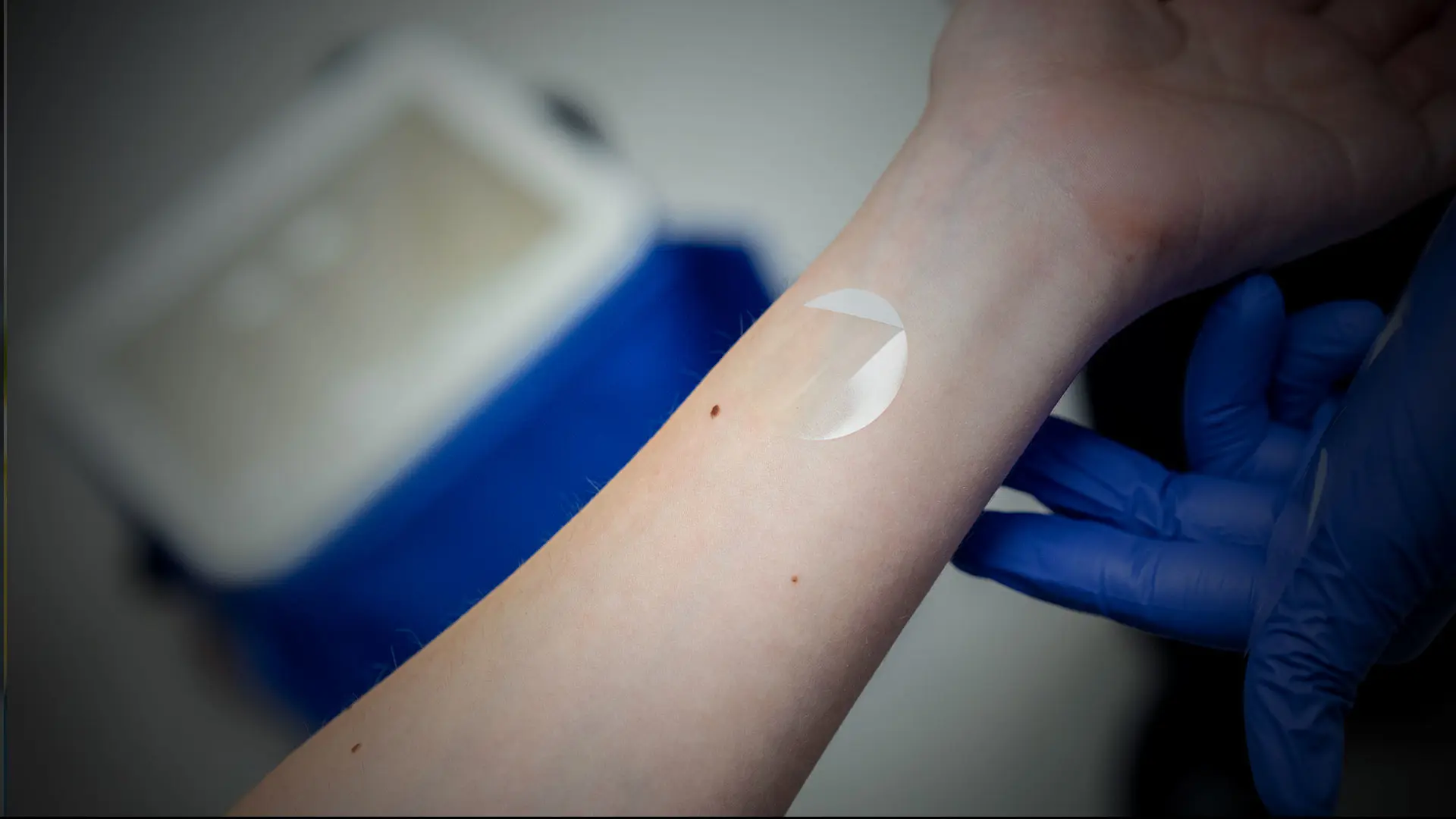
Non-invasive stickers are placed on the skin that give the equivalent of a skin biopsy and afford a window into the patient’s immune problems both in the skin and more broadly in the body, including the gut. Dr. Spencer has already identified immune fingerprints from these skin tapes in patients with IBD that may help with therapy selection. She is following a large cohort of patients with skin tapes to better understand how to use this novel method to target the best single therapy or to combine therapies.
Beyond improving therapy selection for newly diagnosed patients, Dr. Spencer is focusing on the prevention of IBD in high-risk family members. She has an ongoing project tracking unaffected members of families that include multiple people with IBD. She follows their genetics as well as their changing gut microbiome (the bacteria in their stool) and metabolome (the products of the bacteria in the stool, which can have their own effects). She has also been working to establish a dedicated Prevention Clinic in Mount Sinai’s Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center to follow high-risk siblings of patients with IBD. The clinic will use stool, blood, and intestinal ultrasound testing to identify people who may benefit from preventive measures.
These dual initiatives spearheaded by Dr. Spencer aim to seamlessly enhance care for pediatric IBD patients. By intercepting patients before or at diagnosis, Mount Sinai aims to alter the course of their disease, promising a future where lives are forever changed.
Featured

Elizabeth A. Spencer, MD, MS
Assistant Professor of Pediatrics (Gastroenterology)

Emma Guttman-Yassky, MD, PhD
Waldman Chair of Dermatology at Icahn Mount Sinai and Chair of the Kimberly and Eric J. Waldman Department of Dermatology for the Mount Sinai Health System