A Q&A with Brian Coakley, MD, Adolescent Bariatric Surgeon at Mount Sinai Health System
What type of bariatric surgery do you offer teenage patients with obesity?
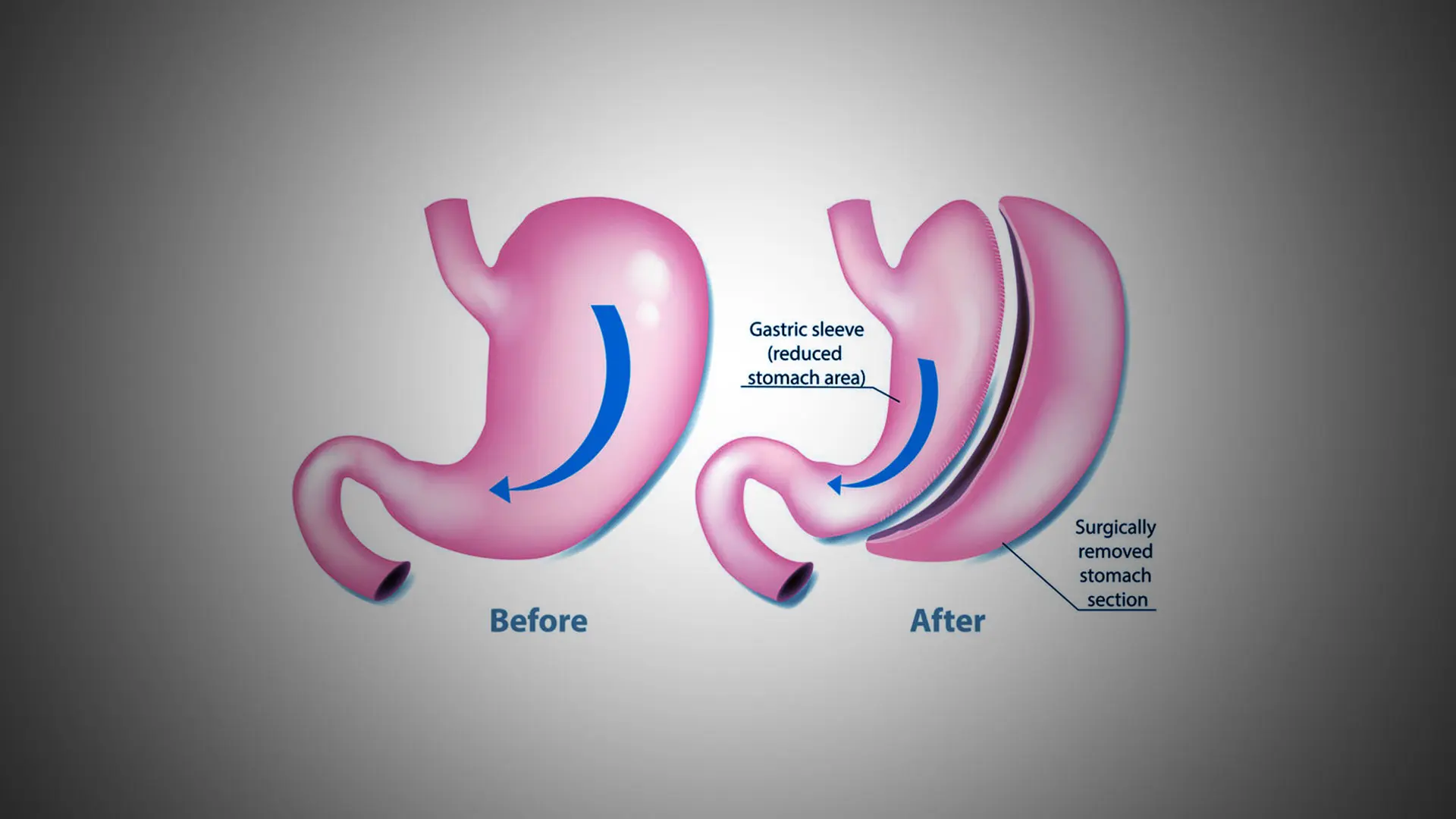
In our adolescent bariatric surgery program, we are currently offering laparoscopic or robotic vertical sleeve gastrectomy (VSG) for most of our teenage patients. For older patients with more severe obesity, and for those with higher burdens of obesity-related comorbidities, the Mount Sinai bariatric surgery program also offers Roux-en-Y gastric bypass (RYGB) as the initial procedure. RYGB is also offered as a revisional procedure for patients who first underwent VSG and either did not achieve adequate weight loss initially or experienced significant weight regain.
How effective and safe is bariatric surgery for adolescents?
Patients undergoing VSG can expect to lose approximately 50-60 percent of excess body weight. Those undergoing RYGB can expect to lose about 65-75 percent of excess body weight. Studies following adolescent patients for 5-10 years after surgery have shown that both VSG and RYGB are effective and safe for long-term weight loss, and in adulthood, both increase overall life expectancy. Having surgery as a teenager significantly improves the chances of reversing conditions such as type 2 diabetes, dyslipidemia, and hypertension compared to waiting until adulthood to perform surgery, so sooner is actually better.
How would a teenager qualify for bariatric surgery?
Adolescents with a body mass index (BMI) of 40 kg/m2 or higher or a BMI of 35 kg/m2 plus a serious complication of obesity are eligible for bariatric surgery. Patients have monthly visits in our clinic for at least six months to promote healthy habits for nutrition and exercise. Medical, psychological, and social assessments ensure that patients are physically, mentally, and emotionally ready for surgery and have a support network at home to help care for them.
If a patient is interested in learning more about lifestyle modification, medications for weight loss, or bariatric surgery, how is a referral to the Healthy Lifestyle Clinic made?
We encourage providers to make a referral here or call 212-241-6936 to learn more.
About the Healthy Lifestyle Clinic
The Healthy Lifestyle Clinic, part of the Mount Sinai Pediatric Endocrinology and Diabetes Clinic, is a multidisciplinary program for pediatric obesity management. Patients with excess weight gain, who often also have other health problems including prediabetes or type 2 diabetes, hypertension, dyslipidemia, fatty liver disease, obstructive sleep apnea, polycystic ovarian syndrome, and depression, are cared for by an endocrinologist, certified diabetes educator, nurse practitioner, nutritionist, exercise specialist, and social worker. If needed, a cardiologist, hepatologist, pulmonologist, psychologist, and adolescent bariatric surgeon are also available. We offer individualized counseling for nutrition, physical activity, sleep quantity and quality, emotional wellness, and, when indicated, meal replacements, weight loss medications, and bariatric surgery. We have specialized equipment for measuring body composition so we can follow muscle mass and percentage body fat as well as visceral fat area as outcome measures.
Featured

Brian Coakley, MD
Associate Professor of Surgery, and Pediatrics