Gabe was 4 months old when the Chronic Lung Care Team at Mount Sinai Kravis Children’s Hospital first met him.
Gabe was born at a gestational age of 24 weeks and the treating team at his referring neonatal intensive care unit (NICU) noted that he required escalating amounts of respiratory support. His physicians sought help, and Gabe was transferred to the NICU at Mount Sinai Kravis Children’s Hospital. Upon arrival, Gabe was requiring significant ventilator support, 100 percent supplemental oxygen, and inhaled nitric oxide to maintain his oxygen levels within a safe range. He was quickly evaluated by the Chronic Lung Care Team, led by co-directors Courtney Juliano, MD, Division Chief of Newborn Medicine, and Douglas Bush, MD, a pediatric pulmonologist. While Gabe was critically ill, they recognized his potential to improve with the right approach.
The multidisciplinary Chronic Lung Care Program at Mount Sinai Kravis Children’s Hospital was established to help care for infants in the NICU, like Gabe, with evolving and established chronic respiratory failure. The program provides individualized care with a family-centered approach, establishing care in the NICU and transitioning infants to the outpatient clinic where they are followed longitudinally. Weekly multidisciplinary rounds provide continuity, enhance communication among providers and families, and help patients achieve individualized goals of care. This collaborative program invests in parents as caregivers and decision-makers with the ultimate goal of improving outcomes for complex patients with severe lung disease.
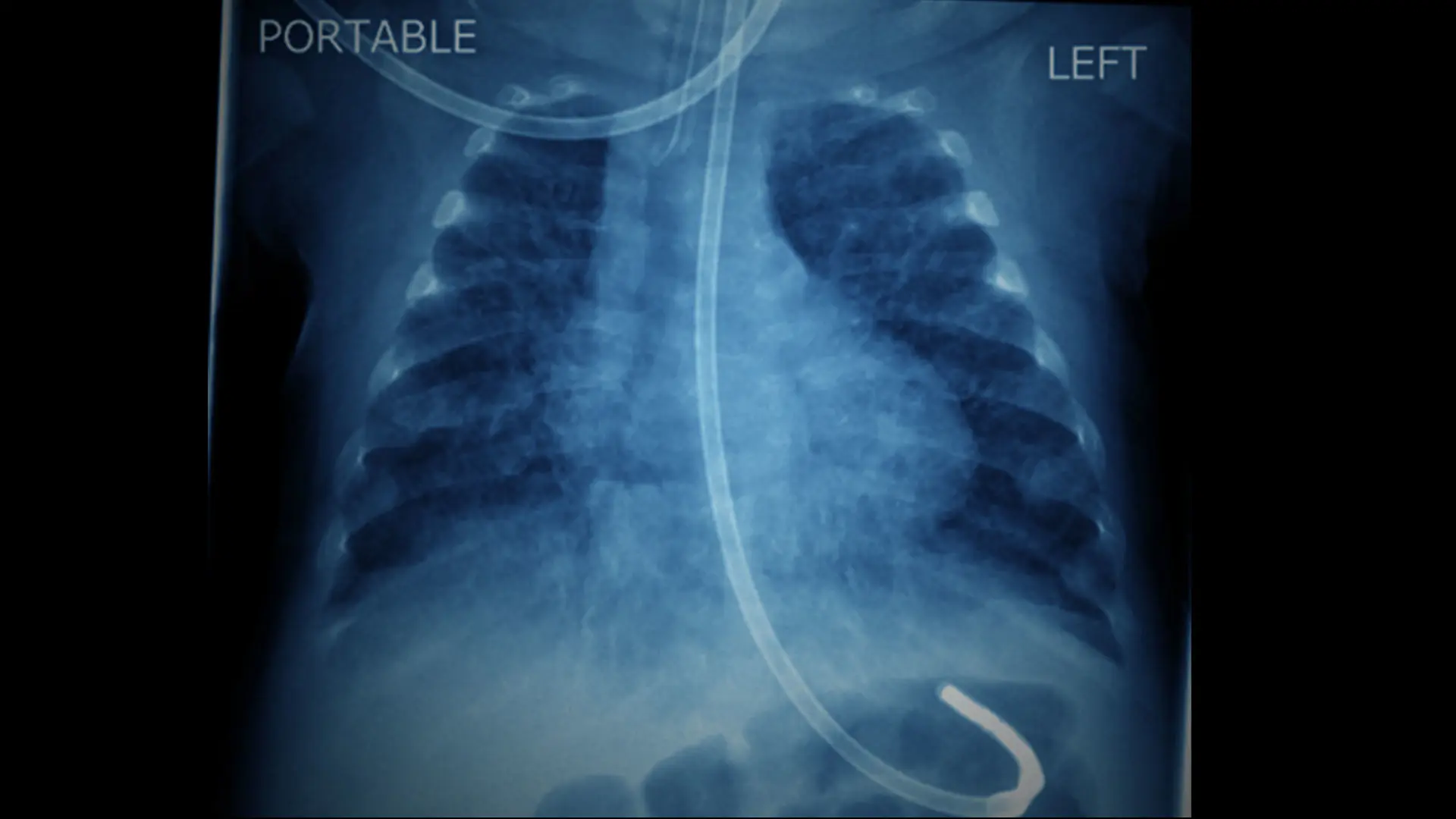
With their expertise in managing acute and chronic respiratory failure, Drs. Juliano and Bush quickly evaluated Gabe’s records, prior imaging, and laboratory studies and surmised that his physiologic challenges required a vastly different approach. A subsequent CT scan of his lungs, an airway evaluation with a flexible bronchoscope, and an echocardiogram quickly confirmed their suspicions, and Gabe was transitioned to a ventilator strategy that better targeted his specific needs. As with many preterm infants with severe bronchopulmonary dysplasia, Gabe’s significant parenchymal lung disease was accompanied by airway malacia and elevated pulmonary vascular resistance. With a change in strategy targeting higher mean airway pressures to stent his airways and recruit his atelectatic lung, his clinical status improved rapidly. His supplemental oxygen requirement was weaned from 100 percent to 30 percent and his inhaled nitric oxide was successfully discontinued within days of his arrival at the Mount Sinai Kravis Children’s Hospital NICU.
As Gabe’s clinical status continued to improve, Drs. Juliano and Bush, in concert with the entire NICU team, engaged Gabe’s parents in discussions about the best next steps for their son. Approximately one month after his arrival at Mount Sinai, Gabe underwent tracheostomy placement. Thereafter, Gabe and his family, with the support of the Chronic Lung Care team and all of the nurses, doctors, and therapists, began the long journey to discharge.
Through weekly rounds and a formal educational curriculum for his parents, Gabe’s team was able to safely send him home before his first birthday, following a seven-month stay at Mount Sinai. He and his family remain deeply connected to Mount Sinai. He now follows up with Dr. Bush in his Chronic Lung Care clinic with both in-person and virtual visits.
Now, as Gabe is approaching his 18-month birthday, he is on track developmentally and meeting all of his motor and cognitive milestones. He loves eating pizza, playing with his baby sister, dancing with his grandmother, running away from Dr. Bush at clinic visits, and causing trouble around the house, including “weaning” himself from his ventilator, which he no longer requires during the day. Through the collaborative efforts of Dr. Juliano, Dr. Bush, and Gabe’s family, Gabe is now a thriving toddler and is well on his way to becoming a happy and healthy child.
Why vote for Mount Sinai Kravis Children's Hospital in U.S. News & World Report’s Best Children’s Hospital rankings?
Neonatology:
We have the largest delivery service in Manhattan (>7000 deliveries annually) and emphasize the provision of expert and evidence-based care for the achievement of excellent long-term outcomes.
We focus strongly on quality improvement with successful programs in place to reduce rates of unplanned extubation, CLABSI, and hypothermia on admission.
We feature multidisciplinary specialty programs for the management of infants with chronic lung disease and inborn errors of metabolism, as well as those requiring neonatal ECMO.
Our point of care ultrasound (POCUS) program emphasizes the use of ultrasound to guide vascular access and assessment of catheter-tip position, assess PDA, and evaluate neonatal hemodynamics. This clinical program is coupled with a fellowship curriculum to teach POCUS skills to training neonatologists.
Our progressive approach to respiratory care is geared toward provision of non-invasive respiratory support for even the most preterm infants. We have very low rates of intubation and ventilation with >90 percent of very-low-birth-weight infants receiving CPAP before ventilation and an approximately 50 percent reduction in average ventilator days per month over the last three years.
We offer an extensive and comprehensive neurodevelopmental follow-up program for high-risk infants including ex-preterm infants, infants with congenital heart disease, infants with bronchopulmonary dysplasia, infants requiring ECMO, and infants affected by hypoxic ischemic encephalopathy.
Pulmonology:
We have the most experienced and comprehensive pediatric bronchoscopy service in the New York metro area, with advanced diagnostic methods including bronchoscopic ultrasound, interventional procedures including cryotherapy, and joint management with a surgical team for complex congenital airway malformations.
We are nationally recognized leaders in severe/refractory asthma.
Our multidisciplinary approach provides comprehensive team care for complex medical conditions including chronic lung disease of prematurity with joint inpatient management with the NICU team, a comprehensive home ventilator program, joint outpatient management of pulmonary hypertension with the Cardiology service, and a comprehensive aerodigestive clinic including pulmonology, GI, ENT, speech/swallow services, sleep medicine, and cystic fibrosis.
We are known for excellent physician communication, with division members recognized in the 99th percentile nationally by CG CAHPS.