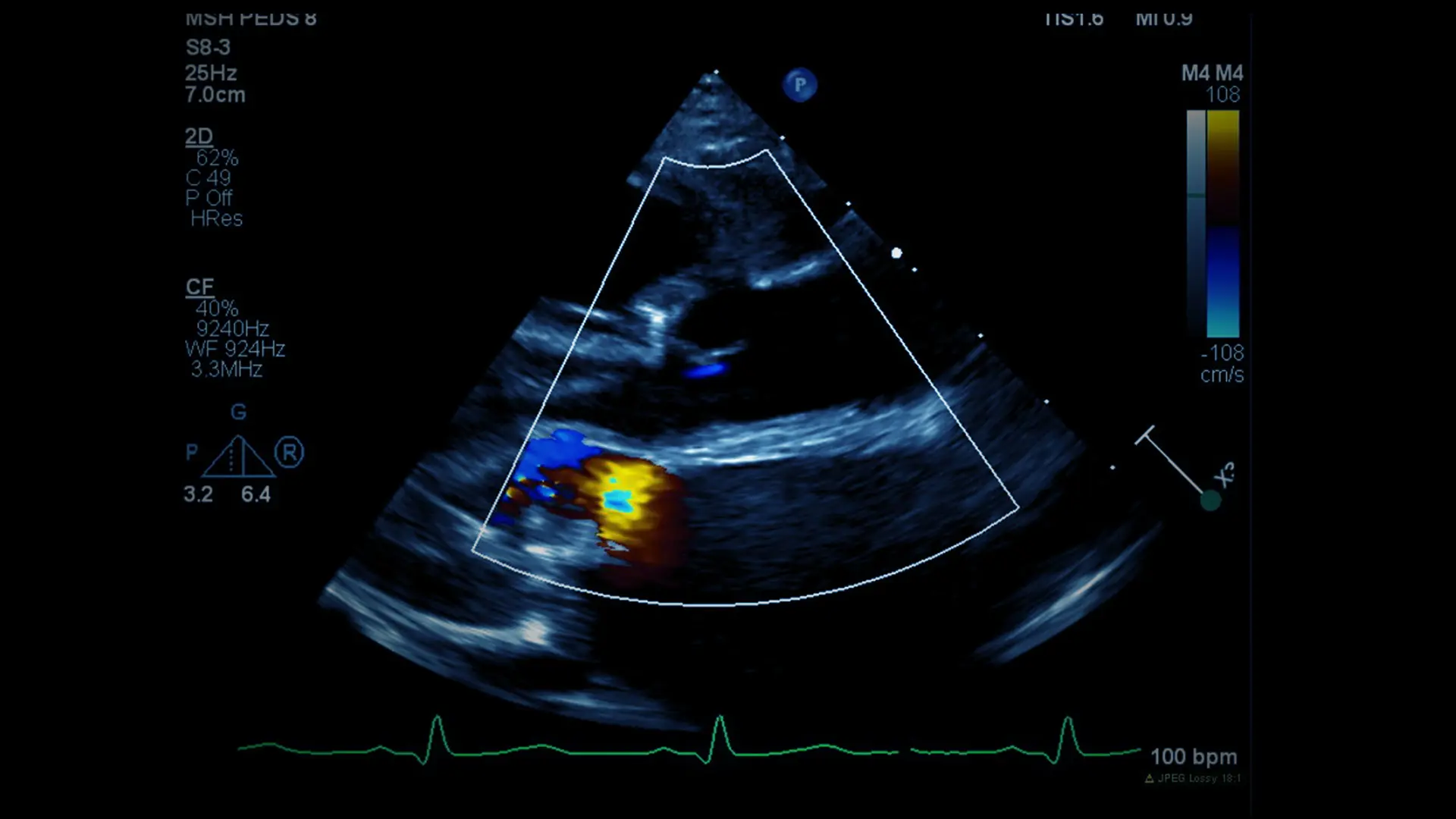
Liba, a 17-month-old girl, was diagnosed with congenital heart valve disease at birth. What sets her apart is that she not only had severe aortic valve stenosis, but also severe mitral valve regurgitation.
When she was just 2 weeks old, Liba’s parents brought her to Robert Pass, MD, Co-Director of the Mount Sinai Kravis Children's Heart Center, and Dr. Pass performed a cardiac catheterization with balloon aortic valvuloplasty. After the catheterization, Liba was left with mild aortic regurgitation, which is not uncommon after a valvuloplasty, but she was still able to go home. Her heart tolerated these residual defects early on, but as Liba grew, she began developing symptoms of heart failure. At approximately 15 months old, she began to appear
weak and her growth plateaued.
Her parents were looking for surgical specialists in congenital heart anomalies, so they brought her to see experts in the Ross procedure and mitral valve repair, respectively: Peter Pastuszko, MD, Co-Director of the Children’s Heart Center, Chief of Pediatric Cardiac Surgery, and Director of Pediatric Cardiovascular Services for the Mount Sinai Health System; and David Adams, MD, Chair of Cardiovascular Surgery and Cardiac Surgeon-in-Chief of the Mount Sinai Health System.
Unfortunately, there are few options for aortic or mitral valve replacement in children her age. By far the best option for replacement of the aortic valve is the Ross operation. During this procedure, the surgeon performs an “autotransplantation” of the healthy pulmonary valve to the aortic valve position and substitutes a homograft, or a valve from a cadaver donor, for the pulmonary valve. The Ross procedure offers a child the potential for proper lifelong function of the aortic valve. The pulmonary valve homograft will need to be replaced in the future, but this is a much simpler and less risky operation compared to a bioprosthetic or mechanical aortic valve replacement.
However, there really is no equivalent procedure for the mitral valve. The best long-term results require a mitral valve repair. Yet the Mount Sinai team was able to repair both of Liba’s aortic and mitral valves during the same operation. Working together, Drs. Pastuszko and Adams performed a successful surgery with excellent results and Liba is now recovered and doing very well.
Her new aortic and pulmonary valves work perfectly, and her mitral valve function has improved tremendously from its leaky and regurgitant state prior to the surgery. Liba is growing well and trending upward along her growth curve. She is an active, delightful, and beautiful baby.
Why vote for Mount Sinai Kravis Children's Hospital in U.S. News & World Report’s Best Children’s Hospital rankings?
We offer the highest level of pediatric cardiac care and experience to tri-state-area patients and families, from fetal care to childhood and beyond.
A team of world-leading experts offers comprehensive and multidisciplinary care offering expertise for children and adolescents with congenital and acquired heart disease. They include congenital heart surgeons and authorities in the areas of fetal cardiology, electrophysiology, interventional cardiology, neurodevelopment, heart failure and transplantation, neonatology, pediatric preventive cardiology, noninvasive imaging, cardiogenetics, and cardiac critical care.
In 2019 we opened a new pediatric cardiac intensive care unit (PCICU) in which expert care is offered from a dedicated team of pediatric cardiac intensivists, surgeons, neonatal intensivists, nurses, nurse practitioners and physician assistants, social workers, and other staff.
The Mount Sinai Adult Congenital Heart Disease Center offers New York State’s only single ventricle survivorship program and many other adult congenital clinics to ensure patients receive proper care as they transition into adulthood.
New leadership of the pediatric cardiac transplant and heart failure team includes the most experienced pediatric heart failure and transplantation experts in the region.