She presented with severe cardiogenic shock (on high-dose milrinone and epinephrine), ventilator dependent respiratory failure, acute kidney injury, and bowel dysfunction, and had had two bradycardic arrests prior to arrival.
Over the next several months, Alexandra was cared for in Mount Sinai’s Pediatric Cardiac Intensive Care Unit (PCICU), under Medical Director Scott Aydin, MD. An extensive heart failure evaluation was performed by Lauren Glass, MD, Interim Medical Director of the Pediatric Heart Transplant Program, and the infant was diagnosed with dilated cardiomyopathy. “Her care was extremely complex and she was very sick when she arrived; the pandemic added a series of hurdles,” says Robert H. Pass, MD, the Richard J. Golinko Professor and Chief of Pediatric Cardiology at the Mount Sinai Kravis Children’s Hospital and Icahn School of Medicine at Mount Sinai.

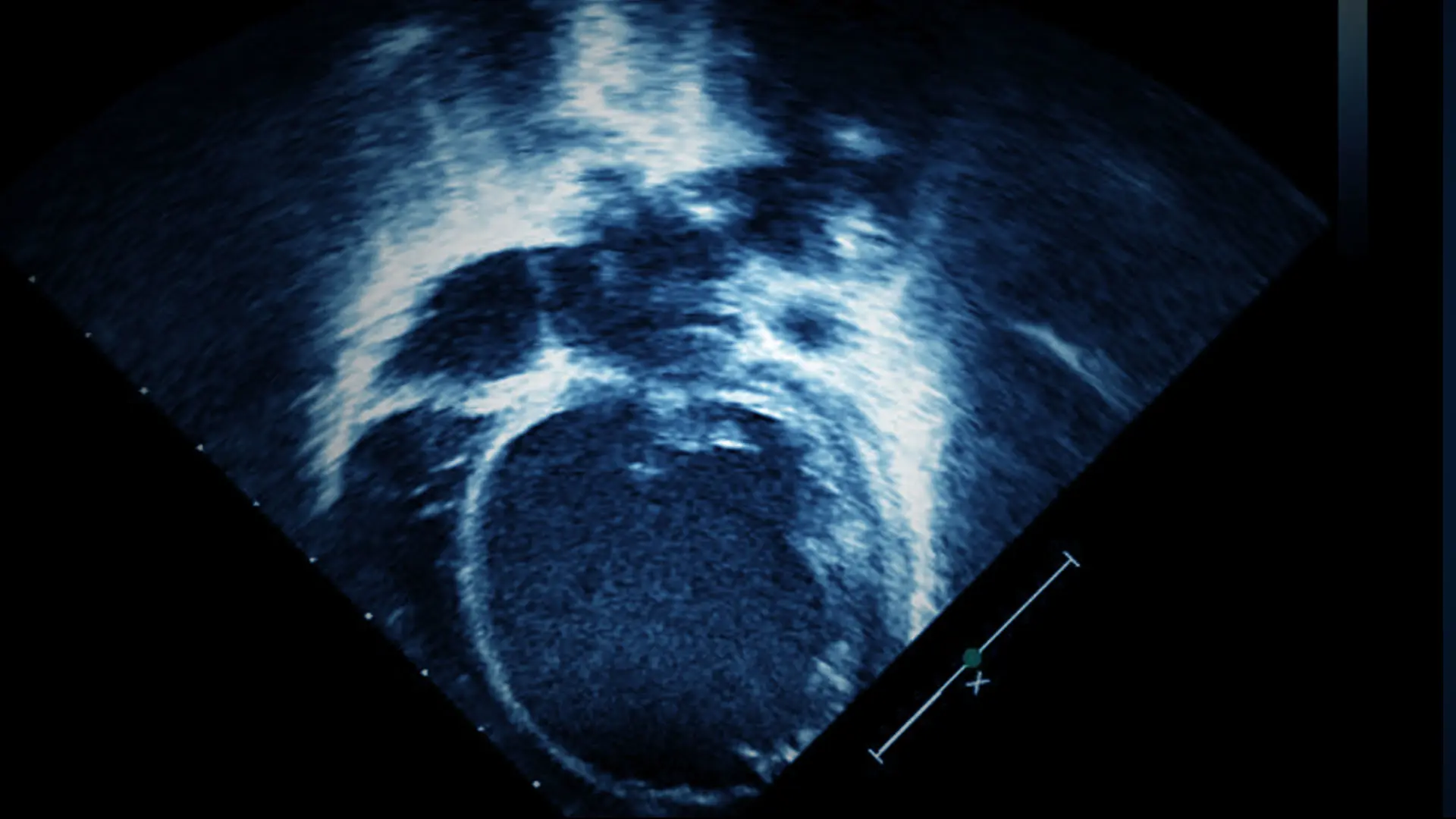
Echocardiogram showing severely dilated left ventricle on arrival to Mount Sinai Kravis Children’s Hospital.

Echocardiogram, s/p orthotopic heart transplantation, showing normal biventricular size.
On Wednesday, March 25, 2020, a team led by Raghav Murthy, MD, Surgical Director of Pediatric Heart Transplant Program, implanted a mechanical ventricular assist device, the Berlin Heart. This is a pulsatile device that can support the circulation while awaiting a suitable heart on the transplant waitlist. The implant was performed on a beating heart using cardiopulmonary bypass via median sternotomy. The inflow cannula was inserted into the left ventricular apex and the outflow cannula to the ascending aorta. The 15 ml pump would provide circulatory support to Alexandra for the next four months. The pump requires anticoagulation to prevent thrombosis. She was maintained on bivalrudin and antiplatelet agents. “On the Berlin Heart, she was extremely vulnerable to infections and strokes, and our critical care team was obsessively vigilant during this time of COVID-19,” says Dr. Aydin.

Alexandra in the PCICU, s/p Berlin Heart implant. Seen in the picture is the 15 ml Berlin Heart pump with inflow and outflow cannula.
Right ventricular failure is a common problem encountered after left ventricular assist device placement. Careful titration of inotropes and diuretics mitigates this problem. Dr. Glass, along with the assistance of the intensivists, was able to get Alexandra back to a much more rehabilitative state. She was able to be extubated, tolerating feeds; weaned off inotropes; and she participated in physical therapy. The maximal benefits offered by mechanical assistance were reaped, allowing Alexandra to be a much better candidate for heart transplantation.
On Thursday, July 9, 2020, Dr. Glass identified a suitable ABO incompatible heart that would be a good match for Alexandra. After all COVID-19 protocols were strictly followed, the donor heart was procured and preserved using the Paragonix SherpaPak Cardiac Transport System. The team, led by Dr. Murthy, performed an orthotopic heart transplant using a bicaval implant technique after explant of the Berlin Heart. Whole blood exchange was performed twice to eliminate any antibodies that would cause hyperacute rejection to the ABO incompatible donor heart. At that time, she was one of only two pandemic-era pediatric heart transplant recipients in the New York region. Our blood bank staff worked around the clock to provide the necessary transfusion support for this procedure. This was an extremely challenging time during the pandemic, as the Mount Sinai blood bank was deeply involved in the donor plasma antibody program to treat COVID-19.
After transplantation, Alexandra was rapidly weaned off inotropic support and mechanical ventilation. She was able to tolerate feeds and participate in physical therapy. After a cardiac catheterization showed excellent hemodynamics and no signs of rejection, Alexandra was discharged home on Wednesday, July 29, 2020. In January 2021, she was 14 months old and thriving. For the team who treated her, she was a ray of sunshine during this pandemic.
Featured

Robert H. Pass, MD
Richard J. Golinko Professor and Chief of Pediatric Cardiology, and Co-Director, Mount Sinai Kravis Children’s Heart Center

Raghav Murthy, MD
Surgical Director of the Pediatric Heart Transplant Program, and Assistant Professor of Cardiovascular Surgery, and Pediatrics

Scott Aydin, MD
Medical Director, Pediatric Intensive Care Unit; and Assistant Professor of Pediatrics (Critical Care Medicine)

Lauren Glass, MD
Interim Medical Director, Pediatric Heart Transplant; and Assistant Professor of Pediatrics (Pediatric Cardiology)