Dylan was 14 years old in the spring and early summer of 2020 when he noticed that his vision was increasingly blurry. His mother scheduled an appointment with an ophthalmologist, thinking he needed glasses, but optic disc edema was noted on his fundoscopic exam. He was referred to Mount Sinai neuro-ophthalmologist Mary-Abigail
Craven, MD, who recognized late-stage papilledema with likely optic atrophy and severe vision loss. Dr. Craven quickly sent him for an MRI.
Dylan was found to have severe hydrocephalus caused by a large pineal region mass and was immediately sent to the pediatric Emergency Room at The Mount Sinai Hospital on Saturday, July 25, for neurosurgical evaluation. He was seen by pediatric neurosurgeon Peter F. Morgenstern, MD, who ordered serum germ cell tumor markers bHCG and AFP, which returned as normal. He then recommended an urgent endoscopic third ventriculostomy (ETV) and tumor biopsy, both to treat the hydrocephalus and attain a diagnosis to guide therapy.
The following morning, Dylan underwent a successful ETV and biopsy. Pathology immediately diagnosed a pineal parenchymal tumor, which necessitated surgical excision.
Dr. Morgenstern and neurosurgeon Saadi Ghatan, MD, Director of Pediatric Neurosurgery for the Mount Sinai System, brought Dylan back to the OR for a craniotomy to resect the tumor using a supracerebellar infratentorial approach in the seated position.
The surgery was prolonged and challenging: Dylan’s chronic hydrocephalus had remodeled his skull, making even the dural exposure difficult and hemorrhagic. Once accessed, the tumor was firm and adherent to the large veins draining Dylan’s thalami, the internal cerebral veins, basal veins of Rosenthal, and vein of Galen.
70% of the tumor was removed.
But these are rare tumors with a high likelihood of recurrence.
Dr. Morgenstern and Dr. Ghatan worked to separate the tumor from Dylan’s brainstem and removed 70 percent of the tumor, leaving the adherent and inaccessible portion behind to avoid injuring these critical veins.
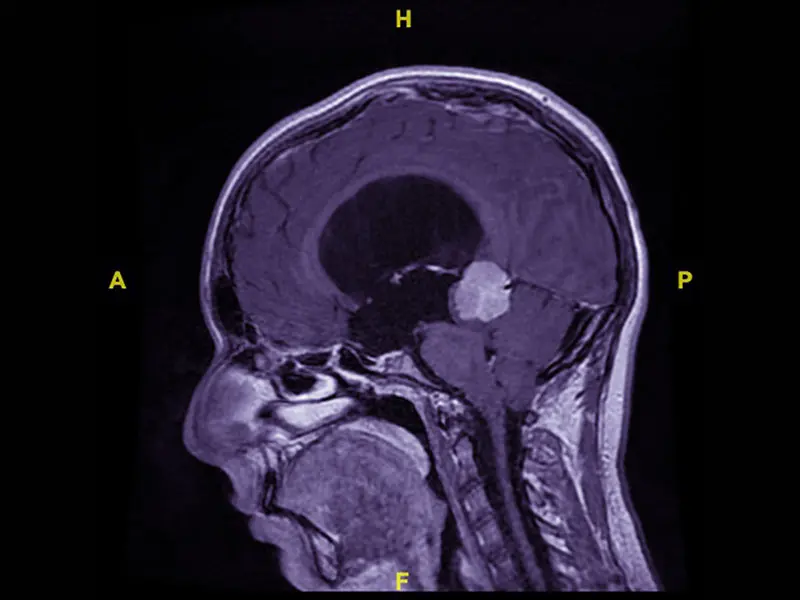
MRI at presentation demonstrating large pineal region contrast enhancing tumor with obstructive hydrocephalus.
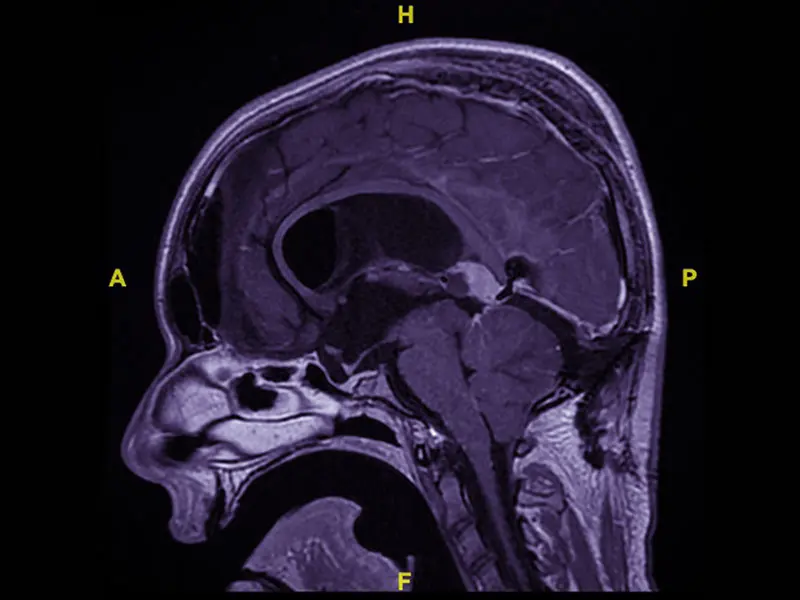
MRI after first resection: This sagittal T1 post-contrast image demonstrates the residual tumor after infratentorial supracerebellar approach for partial resection. The tumor is centered in the posterior roof of the third ventricle, under the splenium of the corpus callosum.
When the specimen from surgery had been processed by pathology, the final diagnosis was a Pineal Parenchymal Tumor of Intermediate Differentiation, WHO Grade II-III. These are rare tumors with a high likelihood of recurrence without maximal resection and adjuvant treatment.
As Dylan recovered in the Mount Sinai Kravis Children’s Hospital PICU, Dr. Morgenstern brought his case to the multidisciplinary neuro-oncology tumor board. It was agreed that further resection would be preferred, if feasible. The remaining tumor was superior to the deep veins and accessible by an interhemispheric transcallosal approach.
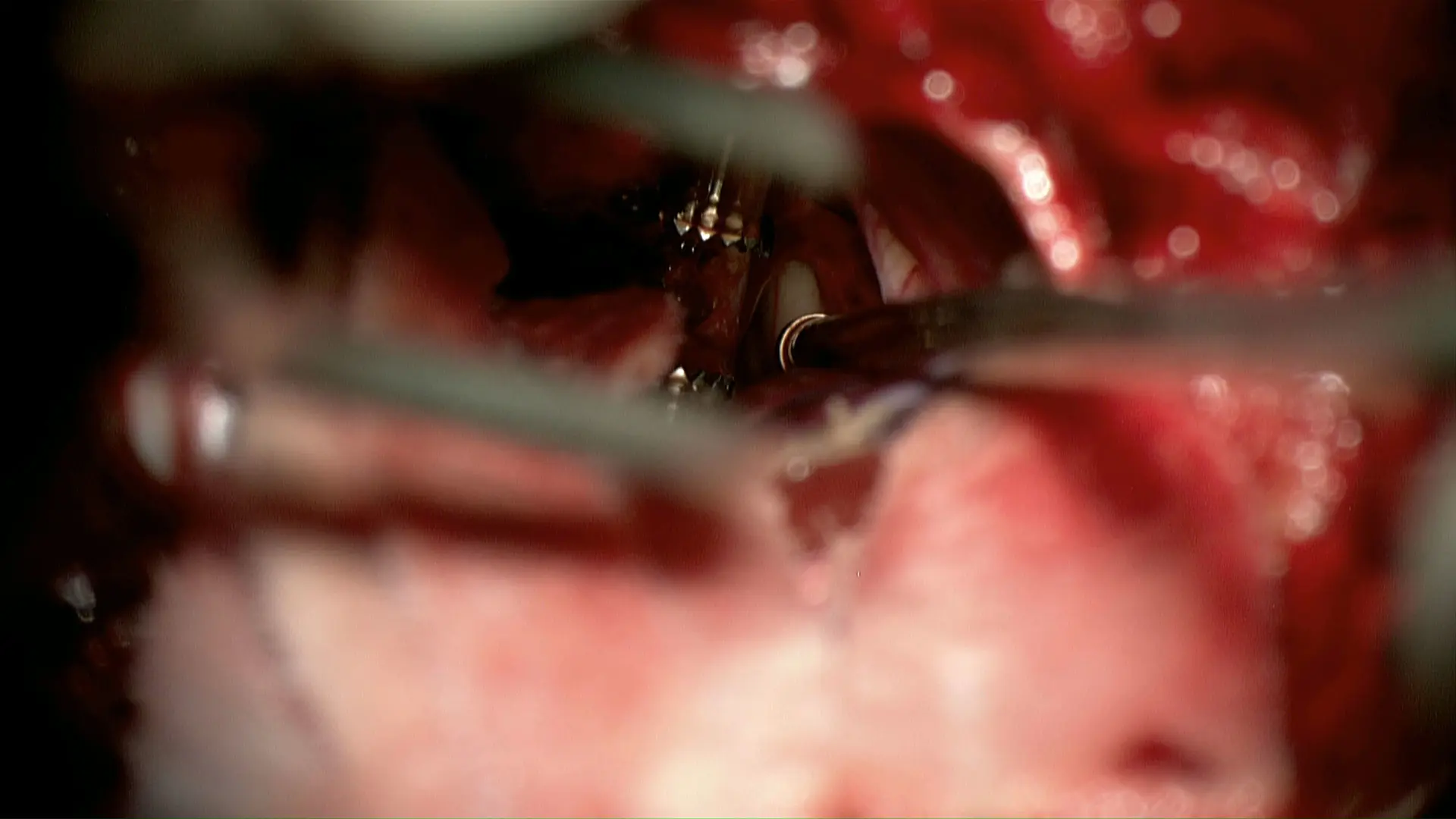
An infratentorial supracerebellar approach was used to debulk the tumor. The third ventricle is seen at the tip of the suction over the top of the cerebellum after the tumor has been partially resected.
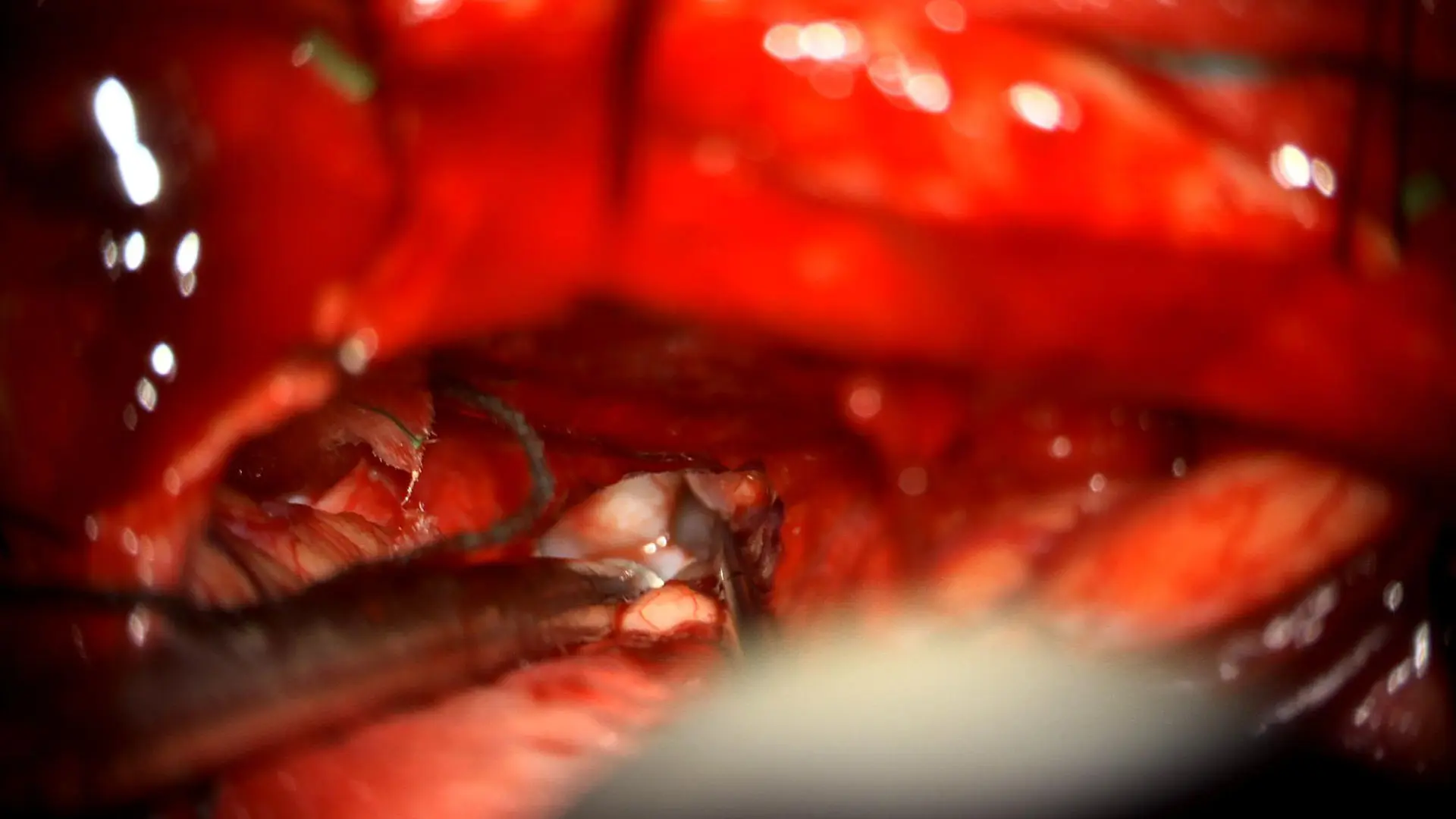
A posterior interhemispheric transcallosal approach was used to access the residual tumor in the third ventricle.
After spending some time in a pediatric rehabilitation center and continuing his recovery, on Friday, September 18, Dylan returned to Kravis to undergo surgery, where Drs. Morgenstern and Ghatan completed a near-total resection of the residual tumor, leaving just a thin layer adherent to the deep veins. Dylan’s recovery from this surgery was much faster, necessitating a one-week hospitalization and another brief stay in rehabilitation.
Dylan is now back home, with plans to continue with adjuvant chemotherapy and radiation under the direction of pediatric radiation oncologist Stanislav Lazarev, MD, and the pediatric oncology team.
Dylan’s case brings together the need for advanced neurosurgical expertise in neuroendoscopy and nuanced brain tumor resection, as well as the critical importance of a multidisciplinary team of experts who can diagnose and treat even the rarest of tumors.
Featured

Saadi Ghatan, MD
Professor of Neurosurgery, and Pediatrics

Peter F. Morgenstern, MD
Assistant Professor of Neurosurgery, and Pediatrics; and Director of Neurosurgery Medical Student Education

Mary-Abigail Craven, MD
Assistant Professor of Ophthalmology, Icahn School of Medicine at Mount Sinai

Stanislav Lazarev, MD
Assistant Professor of Radiation Oncology