When Mount Sinai pediatric patient Arthur Bradley was born prematurely at 33 weeks in December 2024, his parents were prepared for challenges—but nothing could have prepared them for the complexity of his condition. Shortly after birth, Arthur was diagnosed with a type C tracheoesophageal fistula (TEF), a rare congenital anomaly that disrupts the normal connection between the esophagus and trachea.
His condition required immediate surgical intervention, and in December, Arthur underwent an open TEF repair and direct laryngoscopy and bronchoscopy at Mount Sinai Kravis Children’s Hospital. The procedure was successful, and early postoperative imaging confirmed a patent esophagus without obstruction or stricture. However, Arthur’s journey was far from over.
Early Challenges and Coordinated Care
Arthur’s care team quickly recognized the need for a multidisciplinary approach. He was enrolled in Mount Sinai Kravis Children’s Hospital’s Pediatric Aerodigestive Program, where Pediatric Otolaryngology, Pulmonology, Gastroenterology, Speech-Language Pathology, and Surgery collaborated to address his complex needs. The team of clinicians, including program co-directors Chantal Grant, MD, Associate Professor of Pediatrics, and Pediatric Pulmonology, Stephanie Wong, MD, FACS, Assistant Professor, Pediatrics, and Otolaryngology, Joanne Lai, MD, Associate Professor, Pediatric Gastroenterology, all at the Icahn School of Medicine at Mount Sinai, and Beth Kraus, MS, CCC-SLP, Speech-Language Pathology, The Grabscheid Voice and Swallowing Center of Mount Sinai, worked in close collaboration to ensure Arthur’s safety and growth.
Initially, Arthur struggled with feeding coordination and reflux, requiring fortified breast milk and proton pump inhibitor therapy. Speech-language pathologists guided his parents through specialized feeding techniques, including elevated side-lying positioning and nipple adjustments, to ensure safe swallowing and adequate nutrition.
Despite these interventions, Arthur exhibited intermittent stridor and increased difficulty breathing, particularly when agitated. Pulmonary evaluations suggested airway malacia, a condition where the airway walls are softer than normal, leading to collapse during breathing.
“Airway malacia can be frightening for families because symptoms often worsen before they improve,” explains Dr. Grant. “Our goal was to monitor Arthur closely and intervene at the right time—and that collaboration across specialties made all the difference.”
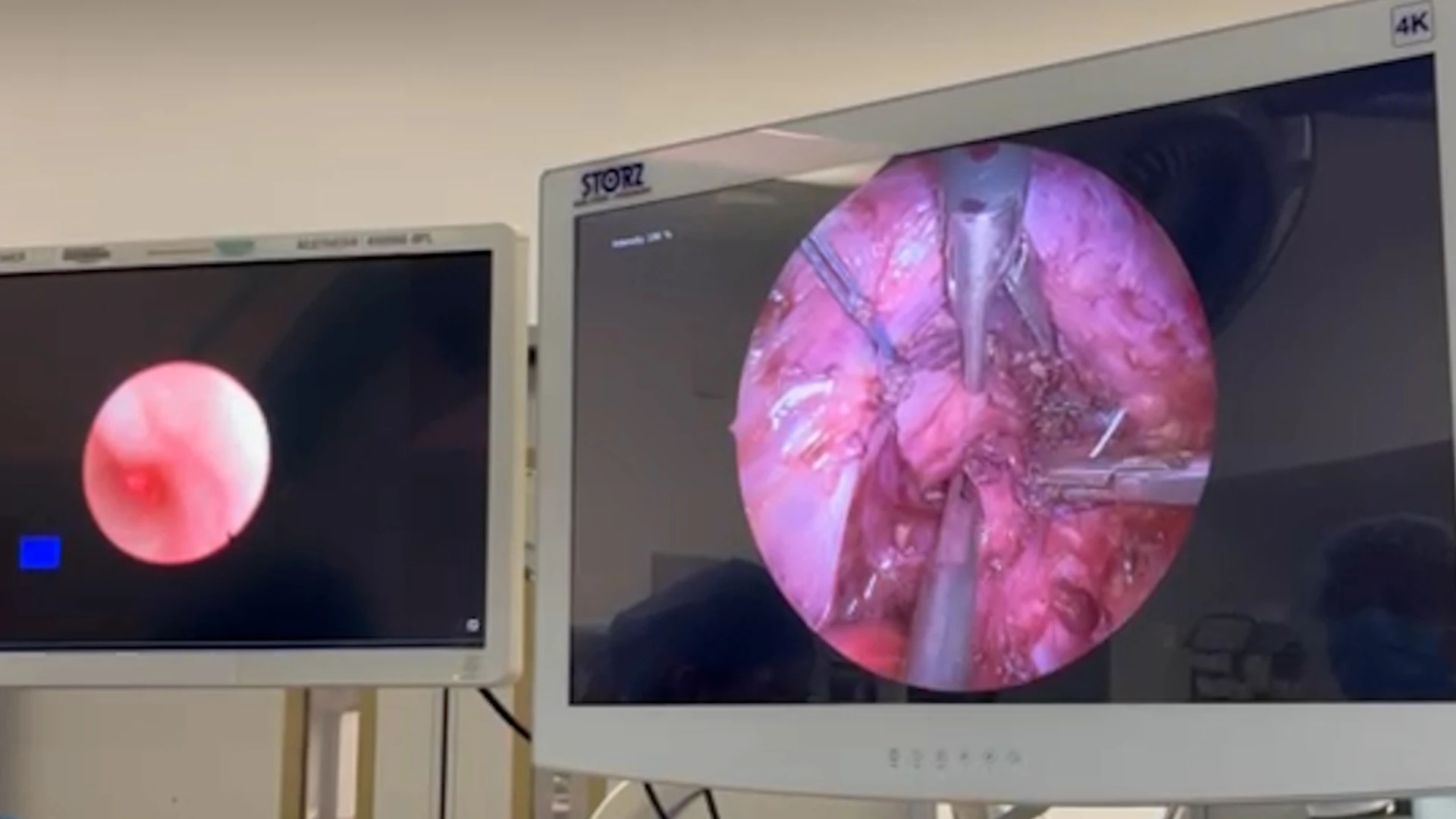
An intra-operative photo with two screens simultaneously showing a thoracoscopic view of the outside of the trachea (right) and an endoscopic view of the inside of the trachea (left) as minimally invasive techniques are used to suture the trachea to the ligaments on the anterior spine.
Escalation and Surgical Innovation
By summer 2025, Arthur was thriving in many ways, gaining weight and meeting developmental milestones, but his airway symptoms persisted. The team made plans for a comprehensive “triple scope” evaluation in the fall. But before that could happen, Arthur experienced multiple brief resolved unexplained events (BRUEs), including episodes of cyanosis and limpness after feeding, prompting urgent hospitalization in August.
“When Arthur turned blue during a feed,” recalls his mother, “it was the scariest moment of our lives.”
A multidisciplinary team performed direct laryngoscopy, rigid bronchoscopy, and esophagoscopy, revealing severe tracheomalacia and distal bronchomalacia. That same month, Arthur underwent a thoracoscopic posterior tracheopexy, a specialized procedure to stabilize the trachea. The procedure was performed by Shunpei Okochi, MD, Surgical Director of Pediatric Intensive Care for the Pediatric Intensive Care Unit (PICU), board certified surgeon at The Mount Sinai Hospital’s Department of Surgery, and Assistant Professor, Surgery, Icahn School of Medicine. Dr. Okochi and his team successfully completed the procedure thoracoscopically, offering a minimally invasive alternative. Postoperatively, Arthur required intensive monitoring in the PICU, but recovered well, transitioning to breathing on his own and being fed by mouth.
“Arthur’s case highlights why early airway evaluation is so critical. His initial repair was successful, but persistent stridor and new BRUEs episodes signaled something deeper,” says Dr. Wong. “The tracheopexy gave him the stability he needed to breathe and thrive.”
Looking Ahead
Today, Arthur is an active, happy infant. He continues to follow up with the aerodigestive team for airway surveillance and feeding therapy. His case exemplifies the power of integrated, family-centered care, bringing together surgical innovation, medical management, and developmental support to achieve the best possible outcome.
“Nutrition was a cornerstone of Arthur’s recovery. We worked closely with his parents to ensure safe feeding strategies and manage reflux, which can complicate airway issues,” says Dr. Lai.
Says Arthur’s mother: “The team at Mount Sinai didn’t just treat him, they supported us every step of the way.”
Learn more about the Pediatric Aerodigestive Program at Mount Sinai Kravis Children’s Hospital.
Featured

Stephanie Wong, MD, FACS
Assistant Professor, Pediatrics, and Otolaryngology

Joanne Lai, MD
Associate Professor, Pediatric Gastroenterology

Chantal Grant, MD
Associate Professor, Pediatrics, and Pediatric Pulmonology
Beth Kraus, MS, CCC-SLP
Speech-Language Pathology, The Grabscheid Voice and Swallowing Center of Mount Sinai

Shunpei Okochi, MD
Surgical Director of Pediatric Intensive Care for the Pediatric Intensive Care Unit, and Assistant Professor, Surgery