In July 2025, pediatric patient Jermaine was delivered full-term at The Brooklyn Hospital Center following his mother’s uneventful pregnancy. But what should have been a joyful beginning marked the start of the newborn’s complex medical journey. Shortly after delivery, he developed signs of respiratory distress and was admitted to the Neonatal Intensive Care Unit (NICU), where he was placed immediately on noninvasive respiratory support. Despite early intervention, his respiratory status and oxygenation continued to decline.
Shortly after, he required intubation and mechanical ventilation to manage his worsening hypoxemic respiratory failure and was ultimately escalated to high-frequency ventilator support. An echocardiogram revealed signs of severe persistent pulmonary hypertension of the newborn. NICU staff initiated inhaled nitric oxide therapy, but the baby’s hypoxia persisted. Recognizing the severity of the situation, Baby Jermaine’s medical team reached out to the Mount Sinai Neonatal Critical Care Transport team to request urgent transfer to the Level IV NICU at Mount Sinai Kravis Children’s Hospital in the Upper East Side/East Harlem, where he could receive the full level of expert care he needed.
It was clear that the situation was both rapidly evolving and potentially life-threatening. The Neonatal Extracorporeal Membrane Oxygenation (ECMO) team was activated in concert with the neonatal transport team to mobilize should ECMO cannulation be necessary. The specialists collaborated with The Brooklyn Hospital Center’s neonatal and cardiology teams remotely to ensure timely access to life-sustaining care.
When the Mount Sinai team arrived at The Brooklyn Hospital Center, they could see time was running short for Jermaine. Knowing that his survival hinged on getting him safely and quickly transported to Mount Sinai, the critical care team transferred him to the ambulance. While en route to Mount Sinai, his clinical status again began to deteriorate, and he went into cardiac arrest. The team immediately initiated CPR and was able to stabilize him.
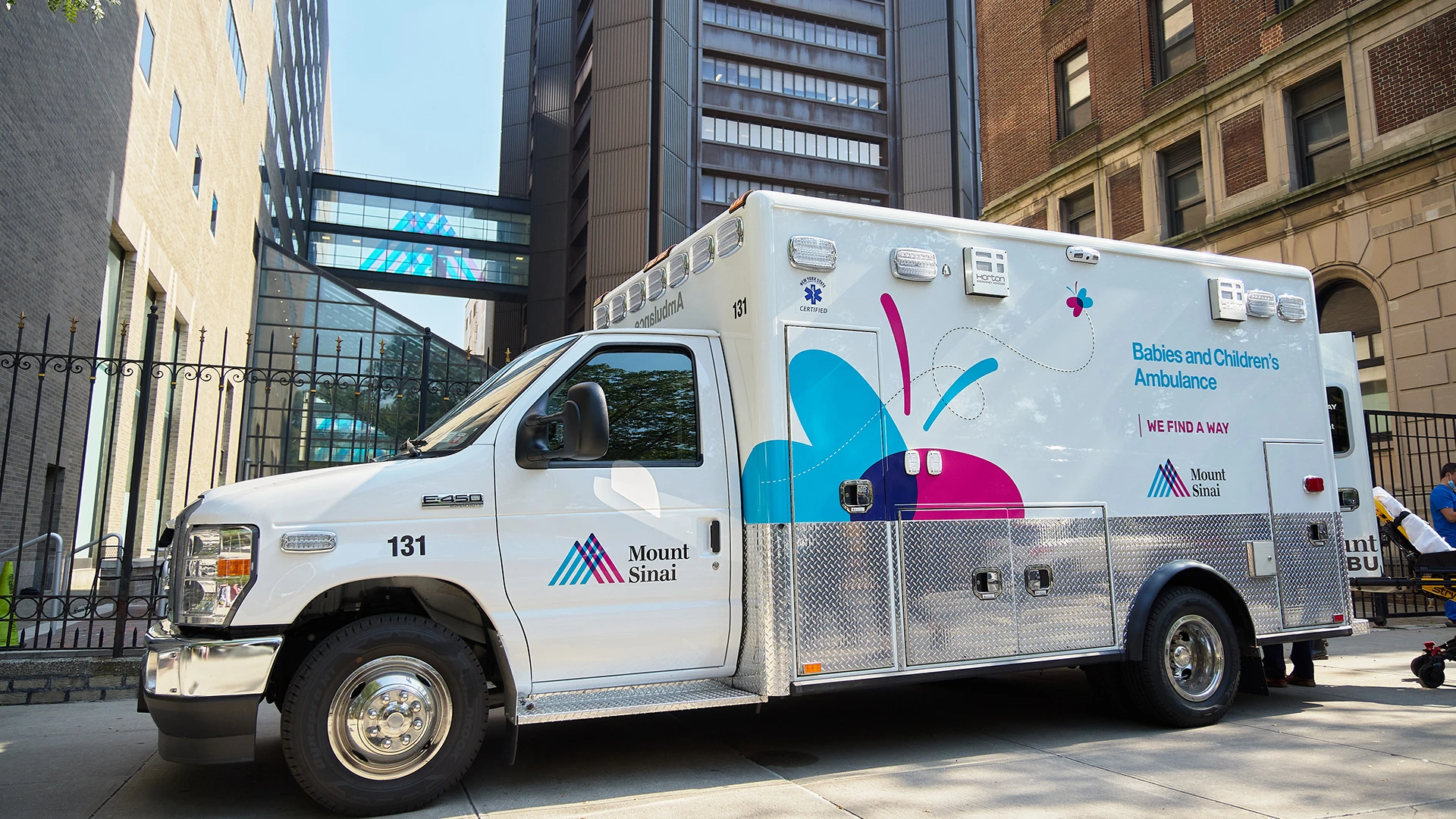
Mount Sinai Kravis Children’s Hospital’s specialized pediatric ambulance is designed for neonatal and pediatric critical care transport.
Following arrival at the Mount Sinai Kravis Children’s Hospital, Jermaine was quickly transferred to the NICU, where Mount Sinai’s multidisciplinary team, including neonatologists, neonatal ECMO attendings, cardiologists, pediatric surgeons, pediatric perfusionists, respiratory therapists, and NICU nurses received him. A brief echocardiogram revealed that the baby’s cardiac function had deteriorated significantly despite escalating inotropic therapy.
Within moments, Jermaine was being prepped for ECMO cannulation, at which point his heart rate again slowed and then stopped. The team again initiated CPR, which continued throughout the duration of ECMO cannulation, and he was successfully initiated on venoarterial ECMO. His hemodynamics and oxygenation stabilized—saving his life and putting him on a path to recovery.
Jermaine remained on ECMO for nine days while his heart and lung function recovered and was ultimately able to come off ECMO support. Over the following days, his ventilator support was weaned; he was successfully extubated and ultimately weaned off all respiratory and cardiovascular support. A team of pediatric subspecialists, including cardiologists, neurologists, and nephrologists, partnered with the NICU and ECMO teams to help manage the complications that resulted from his cardiopulmonary failure and cardiac arrests.
As Jermaine grew more stable, the team shifted their focus from how to help him survive to how to ensure he would thrive. Feeding, occupational, and physical therapists worked in collaboration with neurodevelopmental specialists to help Jermaine reach his full potential. He eventually underwent G-tube placement to facilitate his transition to home while continuing to work on oral feeding. Eight weeks after his eventful admission, he was discharged from the hospital.
“This case is a humbling reminder of how narrow the gap can be between a story of survival and resilience like Jermaine’s and a more tragic outcome,” says Veniamin Ratner, MD, Director, NICU ECMO Program, Mount Sinai Health System; Associate Professor, Pediatrics, and Newborn Medicine, Icahn School of Medicine at Mount Sinai.
From the first moments of life to complex ECMO management and recovery, Mount Sinai’s neonatal transport and multidisciplinary NICU teams exemplify the Health System’s commitment to delivering the highest level of care for the most fragile patients. Thanks to the expert care of Mount Sinai’s team, Jermaine is at home with his family, where his health continues to improve.
“The outcome here was the result of extraordinary communication, coordination, and teamwork coupled with a shared perspective that every baby, no matter how unlikely the odds, deserves a fighting chance,” says Courtney Juliano, MD, Chief of Newborn Medicine, Mount Sinai Health System; Vice Chair of Clinical Innovation, Jack and Lucy Clark Department of Pediatrics; and Associate Professor, Pediatrics, and Newborn Medicine, Icahn School of Medicine.
Featured

Juliano Courtney, MD
Chief of Newborn Medicine, Mount Sinai Health System; Vice Chair of Clinical Innovation, Jack and Lucy Department of Pediatrics; and Associate Professor, Pediatrics, and Newborn Medicine

Veniamin Ratner, MD
Director, NICU ECMO Program, Mount Sinai Health System; Associate Professor, Pediatrics and Newborn Medicine
