A multisite study led by researchers at the Icahn School of Medicine at Mount Sinai has introduced a novel way to interpret patient-reported outcomes in children after liver transplantation. The study, directed by Eyal Shemesh, MD, Chief of the Division of Behavioral and Developmental Health in the Department of Pediatrics, Mount Sinai Kravis Children’s Hospital, and Professor of Pediatrics, and Psychiatry, Icahn School of Medicine, evaluated how differences in perception between children and their parents relate to children’s well-being after undergoing a transplant. The study was funded by the Agency for Healthcare Research and Quality.
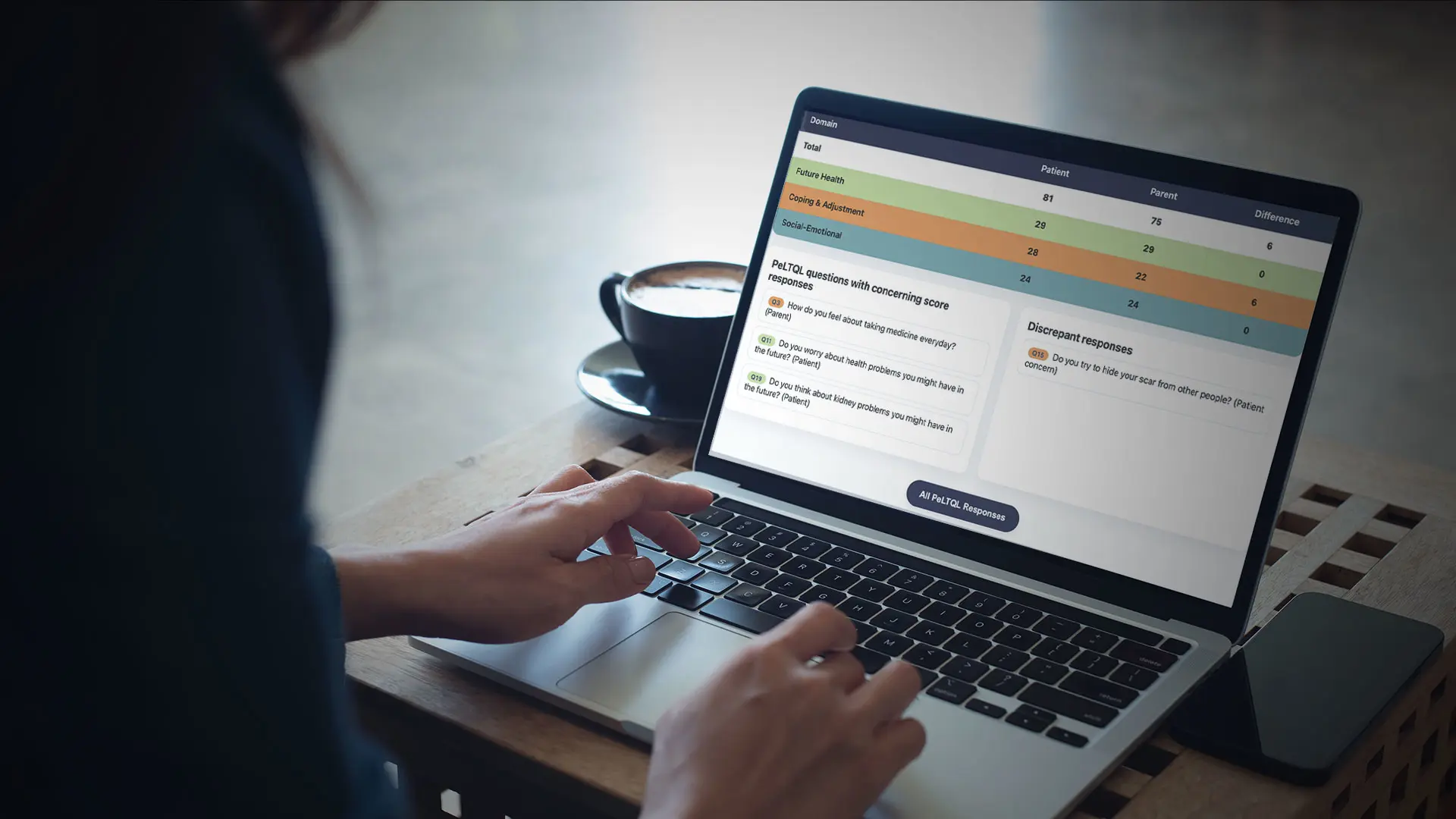
In collaboration with seven pediatric liver transplant centers across the United States and Canada, the Mount Sinai team developed an innovative electronic application that computes in real time, via a questionnaire, the difference between how children and their parents rate the child’s quality of life. The researchers found that larger discrepancies between parent and child responses were linked to lower child-reported quality of life, regardless of medical or liver-related outcomes. When parents and children saw the child’s adjustment differently, the child tended to feel worse—even if their medical recovery was going well.
“What we found is that the story isn’t just in what the child or parent reports individually—it’s in the space between those two perspectives,” says Dr. Shemesh. “The degree to which parents’ perception of the child’s quality of life differs from what the children themselves report tells us something powerful about how a child is truly coping, and how we can make it better.”
These findings highlight a new way to interpret patient-reported outcomes, focusing not only on what children or parents say individually, but on how their views align. This “discrepancy score” offers a powerful lens into psychosocial and emotional adjustment that could help clinicians identify children and families in need of additional support.
“By paying attention to where parent and child perspectives diverge, we can uncover hidden challenges in adjustment,” Dr. Shemesh explains. “This insight gives clinicians a new, practical way to support families, well beyond what traditional medical measures can tell us.”
While the study focused on liver transplant recipients, this approach could be applied broadly to children with other chronic illnesses.
“By integrating this digital, real-time analysis into clinical care, we may gain deeper insight into the lived experience of pediatric patients and improve quality-of-life outcomes across a wide range of conditions,” says Dr. Shemesh.
Featured

Eyal Shemesh, MD
Chief of the Division of Behavioral and Developmental Health in the Department of Pediatrics, Mount Sinai Kravis Children’s Hospital, and Professor of Pediatrics, and Psychiatry, Icahn School of Medicine at Mount Sinai