One of the biggest challenges in managing patients who present with glenoid bone loss through shoulder arthroplasty is the limitations of standard implants. In some cases, the degree of deformity is so severe that these implants either cannot be placed or quickly fail, thus limiting patient mobility and quality of life.
Mount Sinai’s Leesa Galatz, MD, has applied her extensive expertise in successfully treating patients to overcome that challenge. Using advanced three-dimensional (3D)-printed shoulder arthroplasty, she has been able to restore stability and function to patients who had previously been told there were no viable treatment options available to them.
“This technology has almost obviated the realm of the impossible,” says Dr. Galatz, Professor and Chair of the Leni and Peter W. May Department of Orthopedic Surgery at the Icahn School of Medicine at Mount Sinai.
This 3D shoulder arthroplasty restores the ability to do daily tasks, as well as the ability to live pain free. Moreover, it has made replacement surgery more precise and efficient, which is beneficial for Dr. Galatz and her patients.
“We have a customized component, and we have drill guides and instruments attached to the component, which means we are able to place it precisely in less time with fewer adjustments,” she says. “It is reducing the incidence of failure compared to placing a standard component.”
Creating Precise, Customized Components for Each Patient
Development of the customized component begins with a patient assessment to determine whether the patient’s degree of bone loss is beyond the scope of management with an off-the-shelf solution. Once confirmed, Dr. Galatz orders a computed tomography scan of the patient’s shoulder with a slice thickness reference protocol of less than one millimeter to ensure the resulting component addresses the patient’s degree of deformity. After uploading the scan to a surgical planning software tool, Dr. Galatz works with the manufacturer, Zimmer Biomet, to develop the 3D-printed component that will be implanted during surgery, starting with a plastic model to assess fit.
“That is what is new and exciting about this approach,” Dr. Galatz says. “We can log in to the software to look at the surgical plan and make changes. We can test the model and then request the component be more lateral or medial, or we can change the trajectory of the screws. All that enables us to achieve more precision in what we provide our patients.”

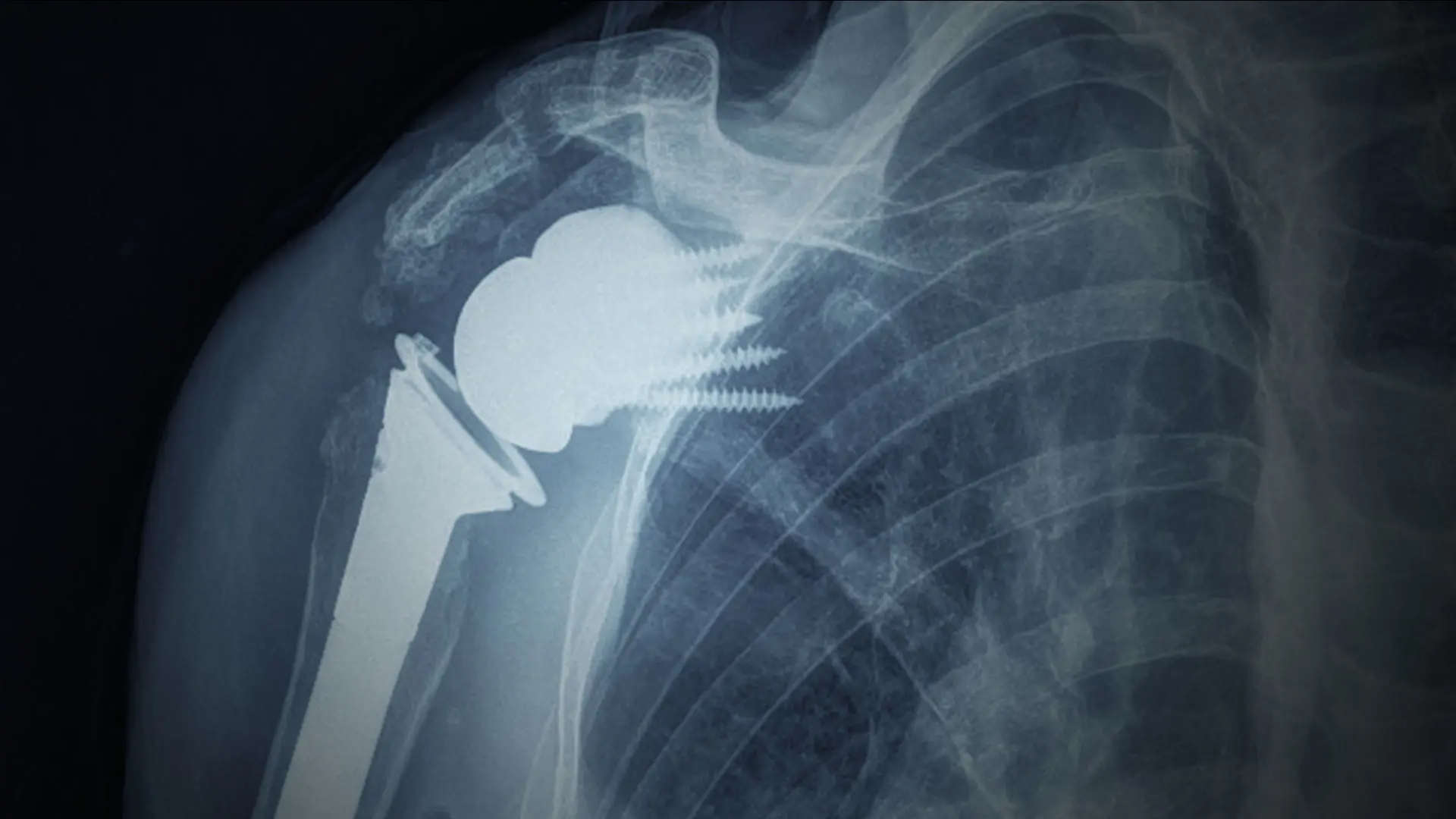
X-ray of a patient's shoulder after undergoing 3D-shoulder arthroplasty.
“This technology has almost obviated the realm of the impossible."
Dr. Leesa Galatz
The customized components created for each patient actually snap into place like building blocks. That fit, combined with the surgical expertise of Dr. Galatz and her Mount Sinai colleagues, has resulted in exceptional results. Dr. Galatz attributes these positive outcomes to the high volume of shoulder surgeries she and her Mount Sinai colleagues perform annually. It is that experience, and their research and innovation, that she believes sets them apart from other centers that are offering this treatment modality.
Dr. Galatz’s goal now is to apply this expertise to help advance the design of implants and instrumentation, and to explore the potential of performing robotic procedures. This, she says, will further benefit patients through less-invasive surgery, reduced operating time, and increased precision, but the real breakthrough has already been achieved.
“We are now able to provide a solution to patients who have been told there is nothing that can be done for them,” Dr. Galatz says. “The patients we have seen are really happy to have access to this treatment and even more happy to have the quality of life they enjoy back.”
Featured

Leesa M. Galatz, MD
Professor and Chair, Orthopedic Surgery