The Spine Bioengineering Laboratory at Mount Sinai is taking a big-picture look at how the spinal organ system interacts with the central nervous system to understand how intervertebral disc pathologies can lead to a lifetime of pain and disability for many. This expansive view is in an effort to unravel one of the world’s leading clinical and socioeconomic health burdens—discogenic back pain. To develop innovative new strategies to treat and prevent degenerative disc disease, the Spine Lab has become a highly collaborative and multidisciplinary site, drawing on physicians, biologists, bioengineers, neuroscientists, and other specialists.
“Our program is focused on bringing together researchers and clinicians to not just understand the fundamental science, but to significantly improve patient care,” says James Iatridis, PhD, Vice Chair for Research in Orthopedics at the Mount Sinai Health System and Principal Investigator for the Spine Bioengineering Laboratory. “Historically, neuroscientists have focused on nerve tissues while orthopedists have looked at intervertebral disc, cartilage, bone, and ligaments. We are now working directly with neuroscientists to understand the cross-talk between cells of the spinal disc and the neighboring nervous system. Similarly, we are working with immunologists to understand how inflammatory systems modulate disc degeneration and pain.”
That systemic approach has been channeled across basic science to study the pathophysiology and potential treatments—particularly regenerative therapies—for discogenic back pain.
Promising Therapies for a Complex Diagnosis
No area has been more pivotal to the work of Dr. Iatridis and his team than nonspecific discogenic back pain. Involving degenerative changes to the intervertebral discs, including structural defects that result in biomechanical instability and inflammation, these disc changes closely intersect with the peripheral and central nervous systems to cause nerve sensitization and, in turn, produce chronic pain. Physicians often struggle to identify the source as well as the right therapeutic strategy for this pain because it is multifactorial.
“Discogenic back pain is often difficult to treat and while many interventions currently exist, they have limited efficacy,” points out Dr. Iatridis, who is Professor and Vice Chair for Research within the Department of Orthopedics. “Our research showed that minimally invasive and specific interventions will likely be the most important first-line treatment.” Their studies published in JOR Spine and PloS One show that early immunomodulatory treatments have potential to slow disc degeneration and pain. Their review, which was published in JBMR Plus, found that regenerative therapies such as biologics, cell-based therapy, intervertebral disc repair, and gene-based therapy, hold the greatest promise over more invasive surgical approaches, once their safety and efficacy are proven in human trials.
Innovating Surgical Techniques to Repair Annulus Fibrosus Defects
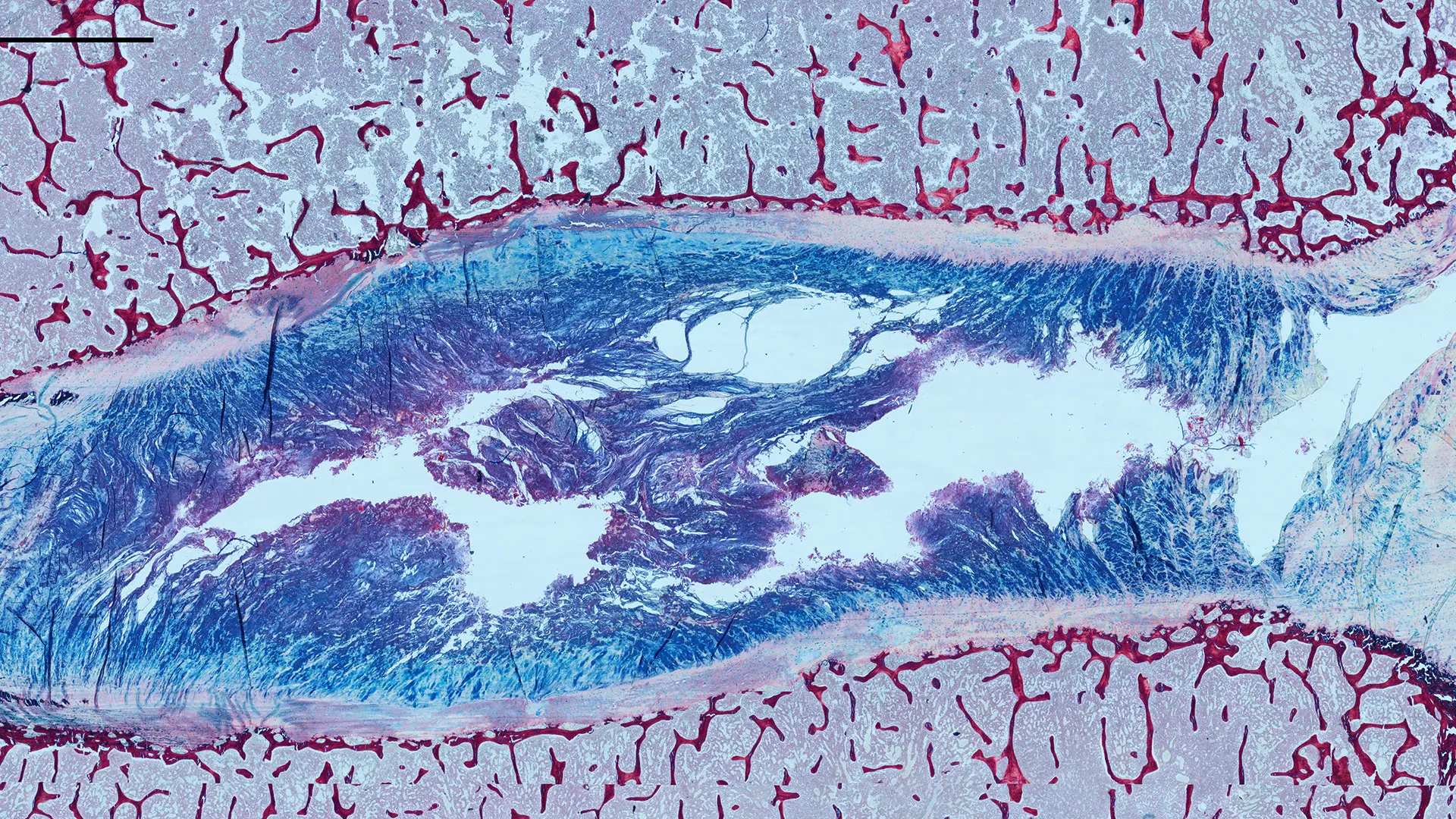
The translational science application of Dr. Iatridis’ approach can be seen in the development of a breakthrough, two-part biomaterial adhesive strategy for annulus fibrosus repair. For this type of debilitating back pain—particularly intervertebral disc herniation—surgery is indicated. The challenge facing the team: once herniation occurs, there is no effective method to repair annulus fibrosus defects after herniated tissue directly compressing the nerves has been surgically removed. Here, the Iatridis lab has been focused on finding innovative ways to seal annular defects and improve discectomy procedures.
Dr. Iatridis elaborates: “Given the high biomechanical loads on the intervertebral disc, a huge unmet clinical need exists for an implantable hydrogel system with strong adherence to annulus fibrosus tissue so it can durably seal annular defects.”
Scientists at Mount Sinai responded to this need with a two-part adhesive strategy to seal and repair defective intervertebral discs. It involves the first-ever hydrogel system capable of preventing recurrent herniation by covalently bonding the biomaterial directly to annulus fibrosus tissue through a new chemical formulation. This unique method of integrating adhesive with native collagen was described in a paper published in Biomaterials. Dr. Iatridis and lead author Tyler DiStefano, PhD, a bioengineer and recently graduated doctoral student in his lab, are now translating the technique to a large animal model to see how it performs on a human-type scale.
The work of Dr. Iatridis and his team has also led to a series of papers in high-profile journals, including a recent study in Advanced Healthcare Materials on extracellular vesicles (known to facilitate intercellular communication) exploring their potential as a next-generation treatment for intervertebral disc degeneration by modulating chronic inflammation.
“What really pushes our translational research in areas such as annular repair is the need to improve existing procedures, while finding robust new ways to treat degenerative disc disease for patients globally,” sums up Dr. Iatridis. “With regenerative therapies poised to open up a new chapter, now is truly an exciting time to be a scientist in this field.”
Featured

James C. Iatridis, PhD
Professor Orthopedic Surgery and Neurosurgery